Introduction
Five percent of the Portuguese population is between 10 and 19 years old.1 Adolescence is a unique period of physical and emotional growth, crucial for the development of habits important for mental well-being. Several factors can affect mental health, such as exposure to adversity (violence, abuse, socioeconomic issues), peer relationships, and identity exploration. Globally, it is estimated that 10-20% of adolescents experience mental health problems, which remain largely unrecognized and untreated.2,3 These adolescents are at higher risk of social exclusion, discrimination, educational difficulties, and risk-taking behaviors.2
Following the global COVID-19 outbreak in March 2020, countries set different standards for dealing with the disease to prevent its massive spread. As of August 2020, 143 countries worldwide had closed schools and other educational facilities.4 In Portugal, schools remained mostly closed from March 2020 to May 2021, and social distancing measures were in place until October 2021.5 These restrictions severely impacted the daily lives of millions of people worldwide, with as yet unclear consequences for mental health. According to one study, young people under the age of 21 experienced more severe psychological distress than other age groups during the COVID-19 pandemic.6 Stressful life events, prolonged confinement at home, sudden school closure, bereavement, intrafamilial violence, and overuse of the internet and social media are factors that may have affected the mental health of adolescents during this period, triggering psychiatric emergencies in individuals with and without pre-existing mental disorders.7,8
The most common contact of adolescents with health care facilities is in the Emergency Department (ED), mainly due to acute conditions.9 Therefore, analyzing the causes of adolescents’ admission to the ED is a useful and important way to evaluate the health status of this population.
The aim of this study was to compare the reasons for adolescents' visits to the ED in the period before the COVID-19 pandemic and after the relief of social distancing measures.
Material and methods
A retrospective cohort study was conducted, including individuals aged 13 to 18 years admitted to the ED of a Portuguese level II hospital. Two 6-month periods were analyzed: from January to June 2019 (Group 1; before the COVID-19 pandemic) and from January to June 2022 (Group 2; after the lifting of social distancing measures).
Data on epidemiological and clinical variables were collected, including date of admission, date of birth, age, sex, Manchester triage system, and final ED diagnosis according to the 11th revision of the International Classification of Diseases (ICD-11).10 For patients with an ED diagnosis of mental disorders, data on pre-existing mental health conditions and follow-up were also retrieved. Data were extracted from electronic medical records. All data were kept confidential. This project was approved by the Ethics Committee of the participating hospital and conforms to the Declaration of Helsinki.
Statistical analysis was performed using the Statistical Package for the Social Sciences (IBM SPSS Statistics 28). Categorical variables were presented as frequencies (n) and percentages (%), and continuous variables as means (M) and standard deviations (SD) or medians (Mdn) and interquartile ranges (IQR) for variables with skewed distributions. Normality was assessed using the Shapiro-Wilk test or skewness and kurtosis, as appropriate. Independent samples t-tests were used to compare quantitative variables after testing for homogeneity of variance using Levene’s test. If the normality assumption was not met, the Mann-Whitney U test was used. Chi-squared tests were used to compare proportions of qualitative variables. Alternatively, Fisher’s exact test was used when the expected frequency in more than 20% of the contingency table cells was less than 5. Odds ratios (OR) and 95% confidence intervals (CI) were calculated. Statistical significance was set at p<0.05.
Results
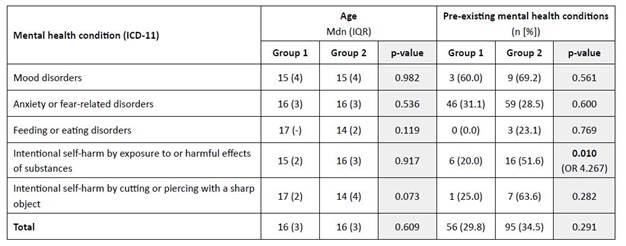
A total of 5135 adolescents were included, 2499 in Group 1 and 2636 in Group 2. Most were female (n=3025; 58.9%) and the median age was 15 years (IQR 2). Adolescents represented approximately 13% of the total ED admissions in both groups. No statistical differences were found between groups regarding demographic characteristics. The Manchester triage was similar in both groups, with a predominance of urgent (yellow) and standard (green) admissions with no statistical differences between groups. Infectious diseases were the most common ED diagnosis in both time periods, followed by musculoskeletal or connective tissue disorders and anxiety disorders.
Comparing ICD-11 diagnoses between the two groups, Group 2 had a significant increase in the proportion of infectious diseases (OR=1.219; p=0.001) and a decrease in endocrine, nutritional, and metabolic diseases (OR=0.270; p=0.013), circulatory system diseases (OR=0.682; p=0.035), skin diseases (OR=0.620; p<0.001), and musculoskeletal diseases (OR=0.687; p<0.001). There was also a significant increase in mental health disorders in Group 2, with a 1.354-fold increase in anxiety or fear-related disorders (p=0.006) and a 12.380-fold increase in feeding or eating disorders, particularly anorexia nervosa (p=0.002), as well as an increase (although not statistically significant) in mood disorders (n=5 vs. n=13; p=0.076) and intentional self-harm by cutting or piercing with a sharp object (n=4 vs n=11; p=0.163). No differences were found between groups in intentional self-harm by exposure to harmful effects of substances (n=30 vs. n=31, p=0.936).
Table 1 shows the characterization of the study population by group.
Table 1 Characterization of the study population by group
CI, confidence interval; IQR, interquartile range; Mdn, median; OR, odds ratio
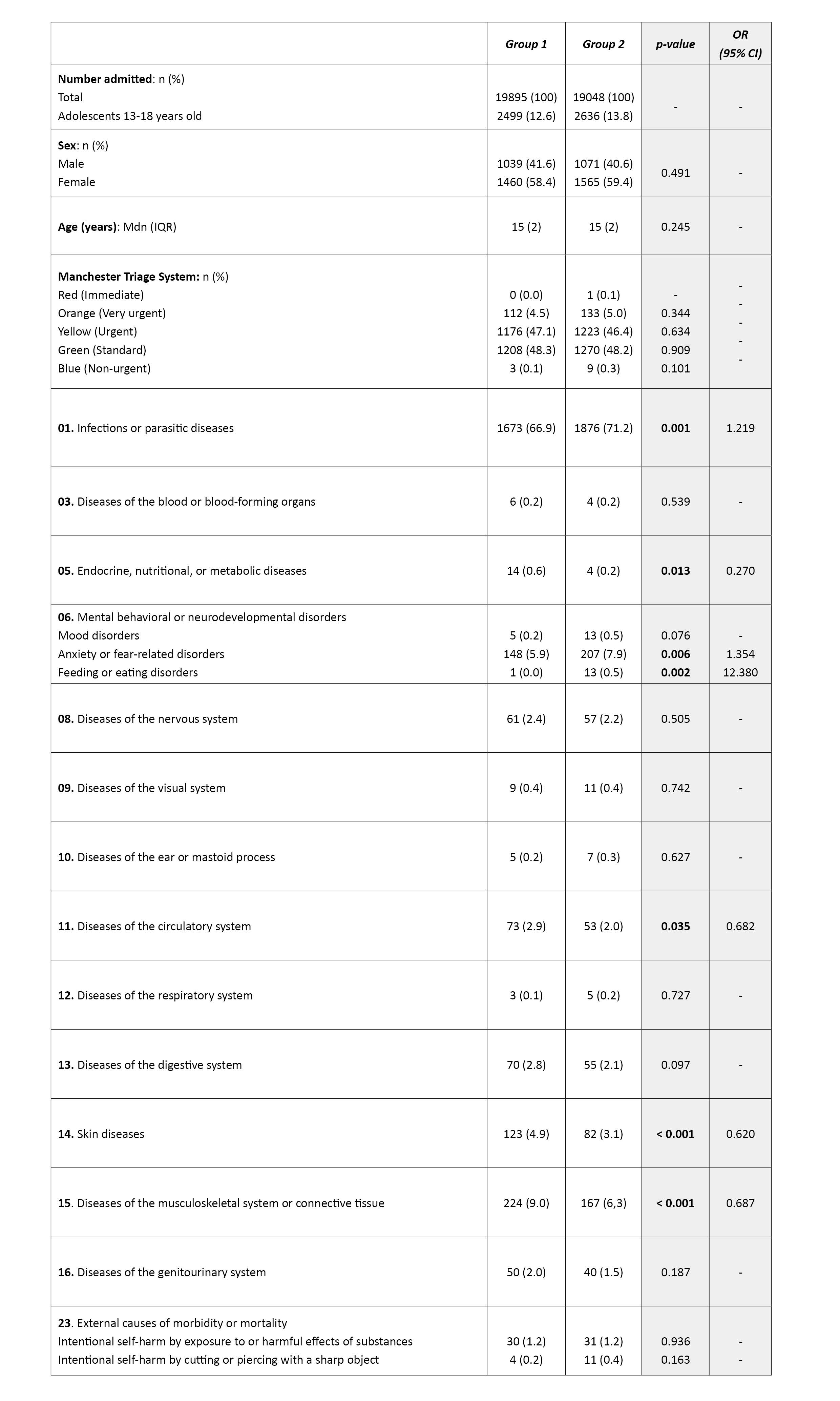
No significant difference was found between groups regarding the median age of adolescents presenting to the ED with mental health disorders, but an important (although not statistically significant) difference was found in the median age of adolescents presenting to the ED with a diagnosis of feeding or eating disorders and intentional self-harm by cutting or piercing with a sharp object, which was three years lower in Group 2. In addition, no differences were found in pre-existing mental health conditions or follow-up between the two groups, except for patients admitted for intentional self-harm by exposure to harmful effects of substances, who were four times more likely to have previous follow-up for mental health disorders (OR=4.267, p=0.010).
Table 2 shows the characterization of adolescents presenting to the ED with mental health conditions.
Discussion
Acute infectious diseases were the most common cause of ED visits among adolescents in the present study. The higher prevalence of this diagnosis in Group 2, i.e., after the lifting of social distancing measures, is probably due to the overestimation of acute symptoms such as fever and cough by the population in the aftermath of the COVID-19 pandemic. Similarly, the decrease in the use of the ED for dermatological conditions could be explained by the reduced use of health services for non-urgent conditions during this period. However, no differences were found between the two groups in the severity of cases admitted to the ED, suggesting that this difference does not seem to be explained by severity-related self-selection.
This study also documented the impact of the COVID-19 pandemic on the mental health of adolescents, particularly regarding anxiety and feeding or eating disorders, the latter being more than twelve times more likely to occur after the pandemic.
The findings of this study are in line with data from the 2022 Health Behavior in School-aged Children (HBSC/WHO) study of Portuguese adolescents, which showed an increase in self-harm from 19% to 24% and feelings of sadness from 9% to 11%, as well as a decrease in the perceived quality of social relationships and health quality compared to data from 2018.11 The HBSC/WHO study also found that 30% of adolescents considered mental health to be the area most affected by the COVID-19 pandemic, followed by physical activity, which is also an important habit for mental well-being.2,11 This is also consistent with the results of the present study showing an increase in mental health conditions and a decrease in osteomuscular diseases. The decrease in the number of adolescents presenting to the ED with musculoskeletal disorders may be explained by the reduction in physical activity due to school closure and the resulting end of physical education classes, as well as by social distancing and lockdown measures that made it more difficult for adolescents to exercise.
This study is also consistent with the findings of Leeb et al. showing a 31% increase in the proportion of mental health-related ED visits among adolescents aged 12-17 years in 2020 compared to 2019.12 Conversely, Erez et al. described a significant decrease in ED visits, especially among adolescents diagnosed with stress-related, anxiety, and mood disorders.13 On the other hand, Breaux et al. showed that the increase in mental health symptoms seen in the early stages of the COVID-19 pandemic did not persist after the summer of 2020.14
This study showed that adolescents presenting to the ED for mental health conditions after the COVID-19 pandemic had a lower median age than those presenting to the ED before the COVID-19 pandemic, particularly those presenting to the ED for feeding or eating disorders and intentional self-harm. This differs from the findings of Davico and colleagues showing a higher mean age of adolescents presenting to the ED for psychiatric conditions during the COVID-19 period.15
Except for intentional self-harm due to exposure to harmful substances, no differences were found in this study in preexisting mental health conditions or follow-up of adolescents presenting to the ED before and after the COVID-19 pandemic. This is in contrast to the studies by Guessoum et al., Chevance et al., and Fegert and Schulze et al., which showed that adolescents with mental health problems were less likely to tolerate a lockdown due to exposure to stressors and lack of continuity of care.7,16,17 A survey conducted in the United Kingdom also reported that 83% of adolescents with a history of mental health problems agreed that the pandemic had worsened their mental health, and 26% reported that they were no longer able to access mental health support.18
The large sample size is a major strength of this study. However, its findings should be interpreted with caution due to limitations such as convenience sampling and the exclusion of adolescents aged 10-12 years.
Conclusion
COVID-19 has undoubtedly been associated with a great deal of collective and individual stress. Adolescents are particularly vulnerable, and their individual, familial, and social vulnerability, as well as their individual and family coping skills, are key factors related to their mental health in times of crisis. This population requires careful consideration by caregivers, and healthcare adaptations - especially during and after a pandemic - represent a growing challenge in ED Pediatrics practice. Protecting adolescents from adversity, promoting socio-emotional learning and psychological well-being, and ensuring access to mental health care are critical to their health and well-being in adolescence and adulthood.
Authorship
Inês Aires Martins - Conceptualization; Data Curation; Formal Analysis; Investigation; Methodology; Project Administration; Validation; Visualization; Writing - original draft; Writing - review & editing
Joana Carvalho Queirós - Conceptualization; Data Curation; Formal Analysis; Investigation; Writing - original draft; Writing - review & editing
Sónia Lira - Methodology; Project Administration; Writing - review & editing
Maria Do Céu Ribeiro - Methodology; Project Administration; Validation; Writing - review & editing