Introduction
Pertussis infection, also known as "whooping cough," is a highly contagious respiratory disease caused by Bordetella pertussis, a gram-negative coccobacillus bacterium and strict human pathogen. Other Bordetella species (Bordetella parapertussis, Bordetella bronchiseptica, Bordetella holmesii) can cause a similar but generally less severe clinical syndrome.1 This infection can affect people of all ages, but is more severe and potentially fatal in children, especially infants.
The whole-cell pertussis (wP) vaccine was introduced in Portugal in 1965, resulting in a significant reduction in disease incidence. The newer acellular pertussis (aP) vaccine was introduced in 2006. Doses are given at two, four, six, 18 months, and five years of age. Although the wP vaccine may be slightly more effective and provide more durable protection than the aP vaccine, wP is associated with a higher incidence of adverse effects.2
Despite high vaccination coverage, this infection remains a concern due to its significant morbidity and mortality. According to the World Health Organization (WHO), more than 151,000 cases of pertussis were reported globally in 2018, with 86% of the target population covered by the diphtheria-tetanus-pertussis (DTP3) vaccine, which protects against pertussis infection.3 A significant advance was the recommendation to vaccinate pregnant women between 20 and 36 weeks of gestation, which was implemented in Portugal in 2016.
According to a Portuguese review, pertussis infection has not been eradicated and there is no prospect of eradication with current vaccination strategies.4 It is acknowledged that immunity following infection or vaccination is not long-lasting and that B. pertussis infection is common and endemic in adolescents and adults. Considering the age-specific cost of pertussis cases and the accessibility of vaccination, vaccination of adolescents, vaccination of household contacts of newborns who have not been vaccinated for up to five years, or a vaccination strategy for both adolescents and household contacts are the most promising strategies to further reduce pertussis morbidity and mortality. Vaccination of newborns remains controversial because safety is not fully established and immune response to other vaccines may be compromised.4
Pertussis infection is spread by respiratory droplets that are aerosolized by paroxysms of coughing and sneezing. The risk of transmission is greater during the catarrhal stage.5) The incubation period for B. pertussis ranges from one to three weeks (most commonly seven to ten days).1
The clinical presentation and course of pertussis infection may vary with age and immunity, and is usually less severe in immunized children.6 Groups at the highest risk of pertussis-related morbidity and mortality include infants, especially those younger than six months, young children who have not been fully immunized, and older adults over 65 years of age.6
The classic presentation includes paroxysms of cough, inspiratory whoop, and post-tussive vomiting. This presentation typically occurs as a primary infection, mostly in unvaccinated children under ten years of age, but is also possible in vaccinated children and adults.1 Classic pertussis is divided into three stages: catarrhal, paroxysmal, and convalescent. The catarrhal stage, with a mild cough that gradually worsens, coryza, and low-grade fever, lasts one to two weeks.1 The paroxysmal stage is characterized by paroxysms of cough between which there is little or no inspiratory effort and occurs with gaging, cyanosis, or apnea and with or without terminal whoop and post-tussive vomiting.1) Paroxysms of cough may develop spontaneously or be precipitated by an external stimulus and occur mainly at night. This stage usually lasts from two to eight weeks. The transition to the convalescent stage is gradual. It is associated with an initial decrease in the frequency of paroxysms and a subsequent decrease in the severity of the events. The convalescent stage usually lasts one to two weeks, but is occasionally prolonged.1 Complications such as apnea, seizures, respiratory distress, pneumonia, pulmonary hypertension, hypotension/shock, renal failure, and death may occur.6
Pertussis infection can be diagnosed without laboratory testing in patients who have a cough illness lasting two or more weeks, no more likely diagnosis, and at least one of the following: paroxysms of cough, inspiratory whoop, post-tussive vomiting, and apnea with or without cyanosis (in infants). Laboratory diagnosis is made by real-time polymerase chain reaction (RT-PCR), culture, or serology.7 Culture is the most specific method, but it is only valid if samples are collected within the first two to three weeks after the onset of cough. RT-PCR is more sensitive than culture. Serology is used as an indirect method by detecting specific antibodies, but cannot be used as a diagnostic method during the first year after vaccination because it cannot distinguish between antibodies due to vaccine and those due to natural infection.8 Although laboratory testing is not required to diagnose pertussis infection, it is often used to confirm it, especially for contact prophylaxis or during an outbreak. However, laboratory confirmation should not delay treatment initiation. Infected individuals with pertussis are considered infectious until they have completed five days of appropriate antibiotic treatment, primarily with macrolide antibiotics.9
Case report
The authors report the case of a healthy two-year-old female with an updated national vaccination program and unremarkable family history.
The girl was admitted to the Emergency Department for loss of consciousness during an episode of paroxysmal cough. The episode lasted one minute, during which the child became cyanotic while unconscious. After regaining consciousness, she became drowsy. When she was admitted to the hospital, she had another episode with cough and cyanosis, which resolved after oxygen supplementation. On observation, she had a third cough paroxysm with signs of respiratory distress, inspiratory cough, and perioral cyanosis, which recovered after stimulation. The remaining physical examination and laboratory workout were negative. Nebulized adrenaline was administered and the girl was admitted to the hospital.
The family described a one-month history of dry paroxysmal cough, usually on falling asleep and awakening, with inspiratory whoop that worsened with crying and was sometimes associated with coughing. Regarding the infectious epidemiologic context, the girl’s ten-year-old sibling had similar clinical symptoms starting two weeks earlier. Given the hypothesis of pertussis infection, the patient was empirically treated with azithromycin for five days. Her household contacts, three siblings and parents, received the same treatment.
During hospitalization, the patient was observed by an otolaryngologist. Nasopharyngoscopy revealed inadequate adduction of the vocal cords leading to paradoxical closure of the cords on forced inspiration. She was discharged after eight days with rare episodes of dry cough, sometimes with inspiratory stridor, but without apnea, cyanosis, or loss of consciousness. RT-PCR for B. pertussis was positive, confirming the diagnosis. The child was referred to a Pediatrics appointment.
Over time, after ten months, she remained asymptomatic and with no long-term clinical complications.
Discussion
Whooping cough is a significant cause of infant morbidity and mortality worldwide and continues to be a public health problem despite high vaccination coverage. The disease is endemic in all countries, and epidemic cycles have occurred every two to five years (typically three to four years), even after the introduction of effective vaccination programs and the achievement of high vaccination coverage.1
Possible explanations for this global change in epidemiology with increased reporting of pertussis cases include the emergence of genetic changes in B. pertussis that render vaccines less effective, decreased vaccine efficacy with progressive loss of vaccine-induced immunity, and better knowledge of the bacteria and availability of better diagnostic tests.10
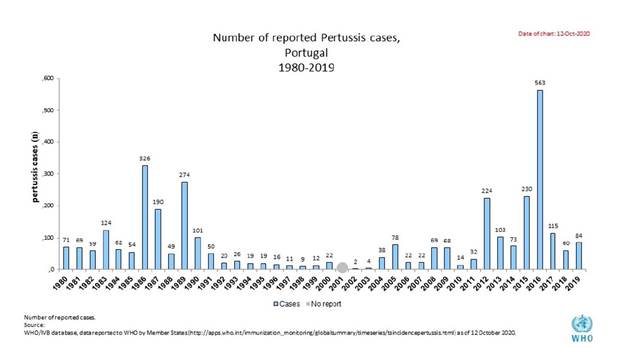
The introduction of effective infant vaccination programs has been associated with a sharp decline in pertussis cases and infant death.(11) A shift in the age distribution of pertussis cases toward older age groups (adolescents and young adults) has recently been reported in some high-income countries, particularly where aP have replaced wP vaccines in the primary series. This age shift may be partly explained by increasing recognition of less typical disease manifestations in older patients, more sensitive laboratory tests, and more sensitive surveillance extended to the entire life span. The waning of vaccine-derived protection and reduced boosting of immunity by circulating B. pertussis are likely to increase the susceptibility of adolescents and adults. As a result, pertussis infection is frequently reported as a cause of persistent cough in adolescents and adults.10 A resurgence of pertussis cases has occurred in some countries several years after the switch from wP to aP vaccine (Australia, Portugal, UK, USA). In the UK and Portugal, a higher incidence of pertussis cases has been observed in unprotected infants, including those too young to be vaccinated.11 Figure 1 shows this increase in pertussis cases in Portugal over the last few decades, as published by the WHO.
Based on the hypothesis of pertussis infection, the patient in this case was treated with azithromycin, the first-line treatment for this disease, even before laboratory confirmation. Early treatment within seven days of symptom onset can reduce the severity of symptoms. However, most patients do not seek medical care until the paroxysmal phase, which occurs one to two weeks after the onset of illness. Over the years, several studies focusing the paroxysmal phase have yielded inconsistent results regarding the ability of treatment to alter the clinical course. A systematic review of randomized and quasi-randomized antibiotic trials for the treatment of pertussis concluded that antibiotic treatment does not alter the clinical course.12 However, in many of the included trials, treatment was initiated after the paroxysmal phase.
The Centers for Disease Control and Prevention supports postexposure antibiotic prophylaxis for all household contacts of pertussis cases; for persons at high risk of developing severe pertussis; and also for persons who will have close contact with those at high risk of developing severe pertussis, such as infants, women in their third trimester of pregnancy, immunocompromised people, or those with moderate to severe medically treated asthma.13
This case report should raise awareness of clinicians to the possibility of severe, life-threatening pertussis infection in younger infants and even children who have completed their primary immunization. Debate remains as to whether wP vaccines are more effective than multi-component aP vaccines, but adverse events are known to be fewer with the latter.14
More research is needed to determine whether additional childhood vaccinations should be considered.15