Introduction
Adolescence is a vulnerable period for the occurrence of deliberate self-harm (DSH). Increased levels of impulsivity and emotional reactivity can occur due to a brain that is still developing.1 The occurrence of DSH is always considered pathological, as a maladaptive and unhealthy attempt to regulate emotions.2
Different definitions and terms are used to describe self-injurious behavior, including “parasuicide”, “self-mutilation”, “deliberate self-harm”, “deliberate self-injurious behavior”, and “non-suicidal self-injury”. Non-suicidal self-injury (NSSI) is intentional, self-directed damage to body tissues without suicidal intent.3 The disorder was recently listed as a condition in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DMS-5).4 Previously, it was classified as a prelude to suicide or as an element of personality disorders.5,6 DSH encompasses self-injurious behaviors, regardless of intent, with nonfatal outcome, and includes methods such as self-poisoning.7,8
Self-injurious behaviors are common among adolescents and young adults, with a global lifetime prevalence of 13.7% for DSH and 22.1% for NSSI.9 In Portugal, the Health Behavior in School-aged Children study estimated 19.6% of DSH in 2018.10
DSH can vary in characteristics, motivation, and severity and may be associated with risk factors, morbidity, and mortality. The most common method is cutting, which is often used to escape terrible thoughts and feelings.11-13 Individuals report that DSH allows them to express pain, release tension, feel in control, or experience some relief from pain or numbness. Most individuals don’t seek help and go unnoticed by their families, making them a high-risk “hidden” population.13 Higher frequency, longer duration, greater variety of methods, and a history of self-cutting in hidden places have all been suggested to increase the risk of suicidal thoughts and behaviors.12 In addition to physical consequences, DSH is strongly associated with depression, hopelessness, social isolation, and difficulty regulating emotions.3,8,14-16 Neurobiological factors such as abnormal stress processing, altered hypothalamic-pituitary-adrenocortical axis, and increased pain threshold also appear to play a role in predicting DSH.1,17,18 Problems in relationships with family members and peers, abuse or a history of bullying, internet addiction, and visiting websites with self-harm content increase the likelihood of DSH.3,6,19,20 Exposure to negative life events can be extremely stressful, and adolescents may use DSH as a coping strategy to reduce stress.21,22
These multitude of biological, psychological, and social factors can help identify a risk profile of adolescents who engage in DSH and prevent future consequences.
Most studies have described an association of DSH with higher odds of subsequent suicidal ideation.23 Globally, suicide is the third leading cause of death among 15-19 year olds and the second leading cause of death among girls in this age group.15 More than two-thirds of those who have attempted suicide also reported a history of NSSI.12
The high prevalence of DSH and the associated risk of suicide make it a natural target for intervention to prevent adverse outcomes in this age group. The aims of this study were to (i) determine the prevalence of DSH in a sample of adolescents; (ii) characterize patterns of DSH; and (iii) assess how lifestyle, adverse life events, and other psychosocial factors are associated with DSH.
Methods
Study design and sample
An observational, analytical, cross-sectional survey-based study was conducted in a Portuguese secondary care hospital. Adolescents aged 12 to 17 years attending an outpatient clinic were asked to complete a questionnaire. Approval from the hospital ethics committee was obtained before study start. Written informed consent was obtained from legal guardians and adolescents. The questionnaire was completed anonymously, confidentially, and voluntarily within 15-20 minutes.
Respondents who did not answer the DSH question were excluded. Data were collected between August and November 2019.
Measures
The study questionnaire was based on the “Lifestyle and coping questionnaire” from the Child & Adolescent Self-harm in Europe (CASE) study and adapted to Portuguese language.2,24
The first section of the questionnaire covered sociodemographic factors, health-related questions, and lifestyle habits such as exercise, dietary habits, alcohol, tobacco, and drug use/abuse. The second section consisted of the World Health Organization’s five-item Well-Being Index (WHO-5) to assess individual emotional well-being. A score <13 or a response of 0 to 1 on any of the items indicated poor well-being.25 The third section consisted of 15 questions to assess the presence of negative life events, such as difficulties making friends, conflicts with peers and family, bullying, history of self-harm, suicide or death of a close relative, violence or sexual abuse, use of the Internet with self-harming content, or concerns about sexual orientation. Self-harm was assessed by the question “Have you ever tried to hurt yourself (e.g., by cutting or burning yourself, overdosing, or overusing alcohol or drugs) with the intention of hurting yourself?” with response options of “no”, “yes, once”, or “yes, more than once”. DSH was assessed instead of NSSI, regardless of suicidal intent and the inclusion of overdose. It has been suggested that adolescents’ perception of self-harm is more concordant with DSH.2 The criteria for DSH were the same as those used in the CASE study.24
Upon an affirmative answer to DSH, respondents were asked about the time of the last episode, the methods used, where the episode took place, the reasons that motivated it, and whether they sought help. There was also an open-ended question to describe in their own words why they hurt themselves.
The final part of the questionnaire was about attitudes toward self-harm and the adolescents’ opinions about these behaviors, with “agree”, “don’t know”, or “disagree” as possible answers. This was measured by the following questions: “Do you think people hurt themselves because they are alone or depressed?”, “...because they want attention?”, “…because they want to die?”, “…in the heat of the moment?”. This was followed by an open-ended question about what they thought should be done to improve quality of life and prevent DSH.
Data analysis
Responses were analyzed using descriptive statistics, followed by bivariate analysis to compare adolescents with and without DSH. Categorical variables were compared between groups using the Pearson chi-squared test, Fisher’s exact test, and Cramer’s V test. In addition, an ordinal regression model was used to examine factors that could be associated with an increased risk of DSH. Associations between self-harm and risk factors were estimated by calculating the adjusted odds ratio (aOR) with 95% confidence interval (CI). Statistical significance was defined as a p-value <0.05.
Analyses were conducted in the Statistical Package for the Social Sciences® (SPSS), v25.0.
Results
Characteristics of the study population
A total of 159 valid responses were obtained from participants with a mean age of 15 years (standard deviation [SD] ±1.59) and female predominance (66.7%). Most families were nuclear (59.7%), followed by single-parent families (21.4%). Nearly 33% of participants had failed at least one grade in school. Nearly 30% had health problems, mainly allergies and asthma. Most adolescents expressed concerns about healthy eating and frequent exercise. Others showed risky behaviors: 23.3% had been under the influence of alcohol at least once in the past year, 3.8% smoked regularly, and 7.5% used drugs. More than a third (34.6%) had a poor sense of well-being.
DSH patterns
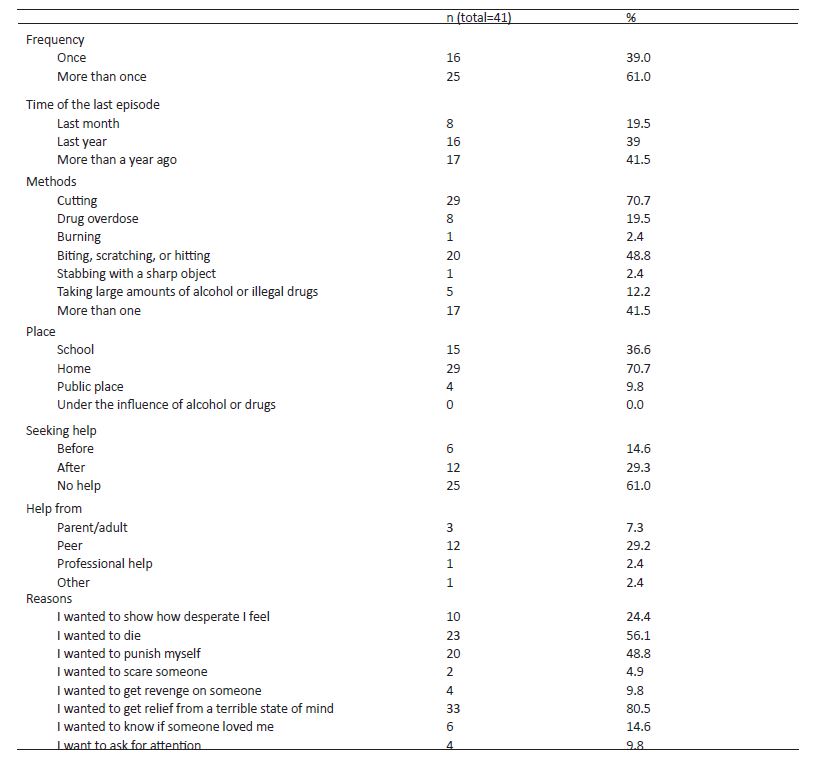
The rate of DSH in the study population was 25.8% and was more common among female adolescents. Sixty-one percent of adolescents who engaged in DSH reported having done it more than once. The majority had cut themselves (70.7%), and almost half (41.5%) had used more than one method. Most had done it at home (70.7%) and were motivated by the urge to “escape from a terrible state of mind” (80.5%), and some said they “wanted to die” (56.1%). In addition, about 61% of these adolescents coped alone, and those who sought help did it by seeking peer support. Table 1 describes the characteristics of DSH in the study population.
Factors associated with DSH
No significant differences were found in gender distribution, age, family organization, or school retention according to DSH status (p>0.05). On the other hand, having health problems and not exercising were significantly more common in the DSH group, while never using illegal drugs, alcohol, or tobacco was more common in the non-DSH group (p>0.05). Almost half of adolescents with DSH (48.8%) had poor well-being, which was more frequent (although not statistically significant) than in the non-DSH group.
Negative life events were significantly more frequent in the DSH group. On bivariate analysis, the DSH group had significantly more difficulty making friends (51.2%, p=0.011) and more frequent conflicts with peers (58.5%, p<0.001), boyfriend/girlfriend (36.6%, p<0.001), or parents (46.3%, p=0.032). Similarly, the prevalence of DSH was higher among adolescents who were victims of bullying (73.2%, p<0.001) and who searched for ways to hurt themselves on the Internet (36.6%, p<0.001). A history of physical (22%, p=0.017) or sexual abuse (14.6%, p=0.010) was significantly associated with DSH. DSH was also more prevalent among adolescents who had someone close attempting suicide or self-harm (56.7%, p=0.001). No significant differences were found in the prevalence of DSH among adolescents whose parents were divorced, who had someone close die, or who had concerns about their sexuality. Compared to adolescents who did not engage in DSH, more adolescents engaging in DSH believed that people who engaged in this behavior wanted to die (53.7%, p<0.001) and disagreed that it was a call for attention (51.2%, p=0.019) . Table 2 shows the characteristics of adolescents who engaged in DSH compared to those who did not.
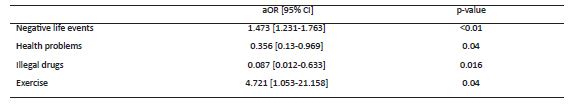
The results of the ordinal regression model are shown in Table 3. This analysis revealed that an increase in negative life events was associated with a 47.3% increase in the odds of engaging in DSH (aOR 1.473, CI 1.231-1.763; p<0.01). The odds of engaging in DSH were 64.4% lower among adolescents without health problems than among those with health problems (aOR 0.356, CI 0.13-0.969; p=0.04). Adolescents who had never used drugs were 91.3% less likely to engage in DSH than those who had (aOR 0.087, CI [0.012-0.633], p=0.016). Finally, adolescents who had never exercised were four times more likely to engage in DSH than those who exercised more frequently (aOR 4.72, CI 1.053-21.158; p=0.04). It should be noted that in the latter case such a strong association may be questionable due to the moderately large standard error (0.765) of the aOR estimate.
Table 2 Characteristics of adolescents who engage vs. who do not engage in DSH
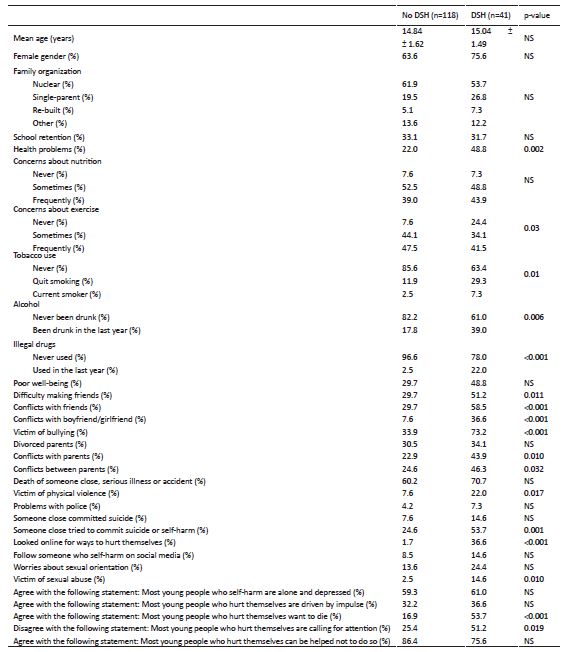
Data are presented as mean ± standard deviation. Categorical variables are presented as percentage and compared between groups using. Pearson chi-squared test, Fisher’s exact test, and Cramer’s V test. Abbreviations: NS, non-significant.
Discussion
The prevalence of DSH among adolescents in this study was 25.8%, a finding that is consistent with data in the literature: the CASE and Saving and Empowering Young Lives in Europe (SEYLE) studies, two of the largest and most important studies in this area, reported a prevalence of DSH among adolescents of 17.8% and 27.6%, respectively.24,26 A recent meta-analysis of DSH found that lifetime estimates of DSH in 12-20 year olds ranged from 5.5 to 30.7% across 20 studies.11 Overall estimated prevalence rates in community and clinical settings vary between 7% and 60%.1,8 In Portugal, a community sample of 1713 adolescents aged 12-20 years in Lisbon reported 7.3% self-harm.27 A major reason for the variation in prevalence estimates may be the heterogeneity of terminology and definitions used to describe self-harm and the diversity of tools used to assess the phenomenon.11 DSH, NSSI, and suicide have been erroneously used interchangeably.
According to a review of longitudinal studies, DSH typically occurs between the ages of 14 and 16 years, and girls are most affected, which is consistent with the findings of this study.11,28 However, no statistically significant difference between genders was found in the present study, a finding that seems to contradict previous research suggesting that girls are more likely to self-harm than boys.4,11,14,29-31
Consistent with other studies, self-cutting was the most common method of DSH, followed by biting, scratching, and hitting.14,24 Less common methods of DSH were drug overdose, burns, and use of large amounts of alcohol or illegal drugs.
Regarding help-seeking, the prevalence rates found in this study were similar to those previously reported.13 Most adolescents had not sought help before or after engaging in DSH. DSH is a hidden problem, and Crouch’s study had already highlighted secrecy as a hallmark. In addition, one of the DSH respondents in that study expressed hatred for the “attention seekers”.32 Once help is sought, peers are the most sought after. Thus, the peer selection group hypothesis postulates that adolescents who engage in DSH are likely to select friends who share the same vulnerabilities, thus exposing them to this behavior.33 This suggests the need for programs that can assist and empower adolescents to support peers who self-harm.11
Consistent with previous findings, the two most commonly cited reasons for DSH in this study were “to get relief from a terrible state of mind” or “to want to die”.24,31 The literature describes four functions of DSH (intrapersonal and interpersonal processes that can be positively and negatively reinforced), while the findings of this study suggest that autonomic negative reinforcement is the most commonly used.1,14 This behavior can be used as a coping strategy and quickly progress to more aggressive methods (e.g., suicide) when DSH fails to achieve the desired outcomes.28 In their own words, adolescents in this study self-harmed because “I felt apart from others”, “no one would miss me”, “I didn’t feel good about myself”, “I was in a bad place”, “I felt empty”. Conversely, a positive intrapersonal response was also obtained: “I self-harmed to be relieved of stress”. These results suggest that avoiding unwanted internal states may be more desirable than inducing positive states, and that the social environment plays an important role in DSH. Shen et al.34 showed that positive social reinforcement was higher in males and served as a powerful form of communication to signal psychological distress and avoid abandonment or seek understanding.
Assessment of DSH patterns may provide a brief window of opportunity to intervene and mitigate the consequences of these acts. Consistent with other findings, a high percentage of adolescents used more than one method and did so more than once. Research suggests that the earlier and longer one engages in DSH, the more likely there will be an increase in the frequency, versatility, and severity of co-occurring psychopathology and suicide.28,30 Adolescents who began self-harming at or before age 12 and who self-cut in hidden places reported a significantly greater tendency toward chronic, severe, and long-lasting conditions.4,12,35
The association between depression and DSH has been well studied and reported in many studies.14,29 Contrary to expectation, no significant difference in poor well-being was found between the DSH and non-DSH groups (48.8% vs. 29.7%; p>0.05). This may be partly explained by the small sample size. Nevertheless, a high percentage of poor well-being was observed in the overall study sample and regardless of DSH, which should not be overlooked, as depression is the ninth leading cause of illness and disability in adolescents.36
On the other hand, previous reports have shown that peer relationships, family conflicts, and academic stressors play a key role in determining DSH.4,7,31 Poor academic functioning and inconsistent school attendance are early signs of emerging or existing mental health problems during childhood and adolescence.14 In addition, poor family relationships, reduced parental involvement, and poor perceived family support predict DSH.3,14 There is also evidence of a bidirectional relationship between parental rejection and DSH, because when parents learn of their children’s DSH, they become overwhelmed with guilt and doubt about their care abilities, with a tendency to reject their children even more, leading to persistent behavior.37,38 Although no significant association was found in this study between DSH and school retention, a higher percentage of DSH was found in adolescents who were victims of bullying or had frequent conflicts with parents or peers. This is in line with other findings showing that reducing family conflict, addressing peer victimization and bullying, and strengthening school support and community belonging predict well-being and are considered strong protective factors for DSH among adolescents.23,39
A robust body of evidence supports the existence of an association between social media and DSH, although its complexity and causality are not well established.19,40 This study showed a high prevalence of DSH among adolescents using the Internet to facilitate this behavior. Parental control of Internet use can play an important role in preventing Internet addiction and access to self-harming content.41
Some research suggests that stressful life events alone are rarely sufficient to elicit a suicide attempt. It is the accumulation of stressful life events with vulnerability factors that appears to increase the likelihood of DSH.7,23 A vicious cycle occurs when engagement in DSH predicts subsequent increase in stressful events.3,14 This study findings support this hypothesis, showing a 47% increased risk of DSH when negative life events are reported.
Previous findings have reported a high prevalence of DSH with risk-taking behaviors.35 Drug and alcohol misuse are associated with increased impulsivity, psychological distress, and thoughts turning into actions.7,14 In the present study, regression analysis showed that adolescents who did not use drugs were less likely to engage in DSH. Study results also showed a lower rate of DSH in healthy adolescents, suggesting that the disease may be perceived as overwhelming and difficult to cope with, predisposing adolescents to DSH.
Overall, it has been suggested that people use DSH as a maladaptive strategy to cope with their affective and social experiences resulting from stressful events.6 This study highlighted the protective effects of positive lifestyles in reducing DSH. In fact, previous findings have shown that high self-worth, high social self-competence, high use of adaptive coping, and resilience are associated with less severe impact of negative life events and consequently less DSH in adolescence.3,21
This study aimed to investigate key factors for identifying individuals at risk of DSH and to develop better screening and intervention strategies to prevent rather than treat DSH within a multidimensional and holistic approach.
The study findings should be interpreted in the context of intrinsic limitations that should be acknowledged. The differences in methodology, age range of participants, sociodemographic factors, and definitions used in the different studies make comparisons difficult. Future research should encourage the use of a standardized definition and tool to assess DSH. On the other hand, the study evaluated a small clinical sample, and its single-center nature limits the generalizability of the findings. Future research may replicate the current study in other geographic areas of the community to help strengthen the model. Another limitation is the possible response bias associated with the use of a self-reported questionnaire. Finally, methodological features such as the cross-sectional nature of the study preclude conclusions about causality.
Conclusion
The present study provided insight into DSH. Although common, it is often a hidden problem that needs to be addressed with appropriate care and support. Negative life events and conflicts with peers and family were strongly associated with DSH, whereas exercise and non-drug use appeared to be protective factors. Awareness of the extent of the problem and identification of those most at risk are critical to prevent negative consequences of distress and discomfort for adolescents. Given the complexity of DSH, health professionals should know the functions of this behavior in order to understand it, identify potential treatment targets, and develop effective approaches. The key message from these findings is that much more attention needs to be paid to adolescents with DSH, and discussion and awareness of this problem should be promoted.
Authorship
Joana Mendes: Conceptualization; Methodology; Investigation; Visualization; Writing - original draft; Writing - review & editing
Miguel Martins: Investigation; Formal Analysis; Writing - review & editing
Isabel Azevedo: Investigation; Writing - review & editing
Sofia Ferreira: Conceptualization; Methodology; Investigation; Project administration; Writing - review & editing
Pedro Patrício: Methodology; Formal Analysis; Writing - review & editing