A previously healthy 16-year-old male presented to the Emergency Department with a 10-day history of edema and pain in the left upper eyelid and complaints of pain in the left thigh. He had no fever. On examination, erythema and edema with fluctuation of the left upper eyelid and frontal region were observed associated with proptosis and blurred vision. Additionally, he had edema, redness, heat and pain, and claudication in the left thigh and gluteal region. There were no signs of trauma, insect bites, or foreign bodies. The boy denied illicit drug use, namely intravenous use. Blood tests revealed leukocytosis (33,700 cells/μL) with neutrophilia (30,600 cells/μL) and elevated C-reactive protein (303 mg/L). Creatine kinase was normal. Computed tomography (CT) scan showed a multiloculated collection in the muscle planes of the thigh (Figure 1) and a partial thrombus in the left femoral vein. It also showed an expanding intraorbital lesion with proptosis and optic nerve extension (Figure 2). Empiric antibiotic therapy with ceftriaxone, clindamycin, and vancomycin was initiated, and the patient underwent surgical drainage of the intraorbital abscess and deep loculated collection in the left thigh. Methicillin-susceptible Staphylococcus aureus was isolated from blood and exudate cultures. During hospitalization, the boy remained persistently febrile despite analytical improvement. Thoracic, abdominal, and pelvic high-resolution CT scans were performed on day 8, showing bilateral cavitary lung lesions (Figure 3).
What is your diagnosis?

Figure 1 CT scan of the left lower limb on admission showing a multiloculated collection in the muscle planes of the left thigh.
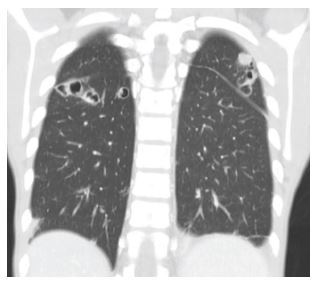
Figure 3 Chest CT scan on day 8 of hospitalization showing bilateral cavitary lung lesions suggestive of septic embolism.
Diagnosis
Staphylococcus aureus bacteremia with multiple foci of infection.
On day nine, a PICO negative pressure wound therapy system was applied to the postoperative wound on the left thigh, with favorable outcome. The patient completed a long course of antibiotherapy with clindamycin (22 days) and flucloxacillin (40 days) with clinical, analytical, and imagiological improvement. On hospital discharge, he presented amyotrophy due to disuse, more pronounced in the left lower limb. The boy underwent a three-month rehabilitation program, with complete wound healing and no motor sequelae. Pediatric immunologic follow-up was unremarkable for potential immunodeficiency disorders, including lymphocyte subpopulations, immunoglobulins, and immune response to vaccines. The case was discussed with an immunodeficiency reference center. In the absence of a relevant personal history suggestive of immunodeficiency disorders, it was decided not to pursue this investigation. After two years of follow-up, the boy remained without further infectious complications. Given this clinical picture, bacterial strains with increased virulence factors were the most likely etiology.
Discussion
Staphylococcus aureus is acknowledged as an important cause of invasive disease in children.1 The global incidence of pediatric Staphylococcus aureus bacteremia varies from 4 to 20 per 100,000.2 It has increased in this century, particularly in regions where successful widespread implementation of infant conjugate vaccines has reduced the incidence of invasive Haemophilus influenzae and Streptococcus pneumoniae disease.1
Bacteremia may be primary or secondary, depending on whether there is an identifiable focus of infection. The majority of pediatric cases are associated with a localized source of infection. Bacteremia caused by Staphylococcus aureus can be divided into community-associated and healthcare-associated, which includes hospital-onset and community-onset. Community-associated cases (40-50%) are due to bone and joint infections (53%), skin and soft tissue infections (14%), or pneumonia (5%). In contrast, hospital-onset/healthcare-associated Staphylococcus aureus bacteremia (50-60%) is associated with central venous catheter and other device infections (34%), sepsis or unidentified source (30%), or skin and soft tissue infections (13%). Community-onset healthcare-associated infections are defined as cases with community onset and at least one healthcare-associated risk factor.2)
Risk factors for Staphylococcus aureus bacteremia include intravascular catheters, indwelling foreign bodies, history of surgery, hospitalization, or dialysis in the previous year, dermatologic diseases, injection drug use, and nasal Staphylococcus aureus colonization. Underlying host susceptibility to recurrent staphylococcal infections includes defects in the immune response and white blood cell function, and malignancy.2-3
Clinical manifestations vary with the site of infection, and severity depends on local suppuration, systemic dissemination, and the effects of toxin production. Staphylococcus aureus is the most common cause of pyogenic infection of the skin and soft tissues and can cause deep soft tissue involvement, including cellulitis, abscesses, and, rarely, necrotizing fasciitis. Localized staphylococcal abscesses in muscle have been termed pyomyositis and may be multiple in 30-40% of cases. Respiratory manifestations include upper respiratory tract infections and inhalation or hematogenous pneumonia, which may be secondary to septic emboli from endocarditis or thrombophlebitis. Necrotizing pneumonitis, empyema, pneumatoceles, and bronchopleural fistulas are known complications associated with this agent. In cases of bacteremia, other sources of infection, such as arthritis, osteomyelitis, or endocarditis, should be considered.4
The management of invasive Staphylococcus aureus infection requires the removal of potential foci of infection. The choice of empiric therapy depends on the site, severity, local susceptibility patterns, and community prevalence of methicillin-resistant Staphylococcus aureus infection. Definitive antimicrobial therapy is determined by culture. Duration varies with site of infection and clinical response to treatment.5
In terms of prognosis, Staphylococcus aureus bacteremia is associated with increased morbidity and mortality. Community-acquired infection is associated with a propensity for metastatic complications, which may be related to the longer time to recognition of bacteremia and possibly the presence of Panton-Valentine leukocidin.6-7 In the present case, the possibility of immunocompromised status was excluded. The absence of previous recurrent infections makes this hypothesis less likely. Therefore, the possibility of bacterial strains with increased virulence factors should be taken into account.
With this case, the authors hope to emphasize that Staphylococcus aureus bacteremia may be associated with multiple foci of infection that should be promptly recognized.
Authorship
Catarina Andrade - Conceptualization; Writing - original draft
Beatriz Câmara - Conceptualization; Writing - original draft
Andreia Forno - Writing - review & editing
Cristina Freitas - Writing - review & editing
Maria João Borges - Writing - review & editing
Maria José Gomes - Writing - review & editing
António Jorge Cabral - Writing - review & editing
















