Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Medicina Interna
versão impressa ISSN 0872-671X
Medicina Interna vol.27 supl.1 Lisboa maio 2020
https://doi.org/10.24950/rspmi/COVID19/J.L.Ascensao/S/2020
ARTIGOS DE OPINIÃO / OPINION ARTICLES
Anatomy of a Pandemic: Perspectives for the other Side of the Atlantic
Anatomia de uma Pandemia: Perspetivas para o outro Lado do Atlântico
Joao L. Ascensão
Professor of Medicine, The George Washington University
Clinical Professor of Medicine, USUHS
Adjunct Professor of Medicine, Georgetown University Chief, Hematology-Oncology Section
Abstract:
The recent pandemic caused by COVID-19 has had major worldwide repercussions across all levels, in particular in health care and the economy. The US has been has been severely affected and remains the country with the highest recorded number of infections and deaths due to this corona virus. The heterogeneous distribution of cases appears to due to a number of factors: individualized responses across different states, a lack of a coherent federal policy, a lack of preparation, the climate of mis/disinformation and the politicization as a result of it occurring in an election year. Add to that a global worsening of health measures for many Americans including obesity, diabetes, hypertension, smoking among others. On the positive side, the scientific collaboration, the observations of astute clinicians and the continued efforts of the public health sector to re-direct the conversation towards scientific truths have played a good part in the fight against this infection. While there is a concern for the hype associated with incessant reporting of the news, let us try to find a common and safe path to live with this virus while protecting the older population and those at risk. Achieving herd immunity or effective vaccination will go a long way towards a return to a new kind of normality.
Keywords: Coronavirus; Coronavirus Infection; COVID-19; Pandemics; United States
Resumo:
A recente pandemia provocada pelo coronavírus COVID-19 tem tido repercussões mundiais a todos os níveis desde a saude a economia. Os Estados Unidos da America têm sido seriamente afectados, embora de uma maneira heterogénea. Isto deve-se a uma reacçao tardia, uma má coordenação entre os estados, na ausência de uma política federal, um a politização (estamos em ano eleitoral) das medidas necessárias, falta de preparação para este tipo de epidemia, e o advento de informação destorcida. Para isso também contribuiu muito uma pioria da saúde dos americanos, com elevada taxa de obesidade, diabetes, hipertensão entre outras. Vale-nos a colaboração científica que transcende fronteiras, clínicos perspicazes, e uma luta dos elementos de saude publica por uma veracidade de notícias, embora a media seja de culpar, em parte, pelo histerismo causado por notícias incessantes sobre a morbilidade e mortandade deste vírus. Vamos ter de aproveitar para descobrir um melhor modo de viver com este vírus enquanto não houver imunidade de manada ou vacinação eficaz e universal.
Palavras-chave: COVID-19; Coronavírus; Estados Unidos; Infecções por Coronavírus; Pandemia
Introduction
Corona viruses have been around for millennia and are often responsible for the common cold. Some of these viruses are zoonotic -i.e.: capable of adapting/infecting different hosts including humans. Recent encounters with SARS and MERS, two of the more dangerous/lethal versions should have had us thinking of other dangerous viruses. Several prescient talks, think Bill Gates in a TED talk in 2015 and the film Contagion by Steven Soderbergh (2011) brought into focus the need to prepare for another onslaught. As the billionaire Warren Buffet once remarked, “its not until the tide goes down that you see who has been swimming naked”.
COVID-19 in the US
Two coasts, two stories, both linked by air travel. COVID-19 got its name by being discovered in 2019, not by being the 19th known corona virus, as opined by some ill prepared media folk. It is believed to have originated in the city of Wuhan (population 11 million). From there, it traveled to Seattle. Patient zero, diagnosed January 19, 2020 continued his subsequent travels setting in motion some of the earlier infections.
The inability to recognizethe myriad of cases as part of the pandemic, hampered early efforts to contain it. Add to this the very contagious nature of this virus, extensive traveling, a pre-symptomatic infectious phase and you have the ingredients for a perfect storm. Although the west coast experienced some of the first cases, the recognition of the disease and rapid implementation of isolation/social separation mitigated its effects. Not so for New York City, which was swamped by the disease and to this date continues to have very high levels of cases and fatalities. The political impasse and indecision of the Federal government, with its initial reluctance to recognize and declare a disaster emergency, contributed significantly to the spread of the disease. Particularly at risk are residents of nursing homes.
So what were the measures taken to control this infection?
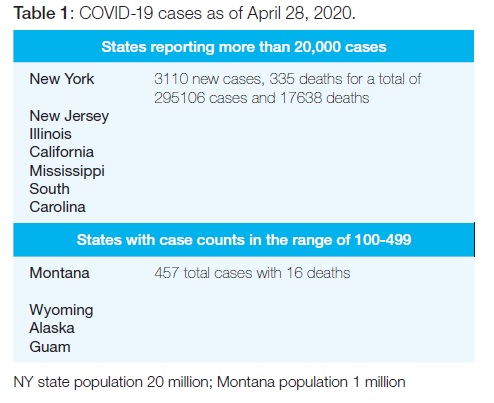
The imposition of physical distancing was predicated on the scientific information available at that time, and the need to decrease the number of cases, to avoid flooding the hospitals, the so called flattening the curve. Patients who become ill remain so for weeks at a time, blocking needed hospital beds. So, while New York was a major epicenter, other cities and states suffered as well, New Jersey, New Orleans, Connecticut and others. Clearly spared were the more rural states, as can be seen in Table 1. In New Orleans it was felt that the Mardi Gras celebration contributed to the spread of the virus, thus providing some support to earlier decisions to quarantine the population. Many models of disease expansion have been created and more have tried to ascertain its mortality. Such efforts have resulted in disparate figures and led to different approaches. At this time, it is unclear if the strategy of isolation is beneficial, beyond its ability to slow down the new cases. This approach, which may be essential for older individuals, given high mortality in this group, prevents the development of herd immunity; only this or successful vaccination will stop the progression of the pandemic. Of course, to find out about herd immunity we need to be able to test all individuals, and such tests are abundant, more than 90 over here, only eight approved by Food Drug Administration (in a very short period).
So, what is happening on the medical side?
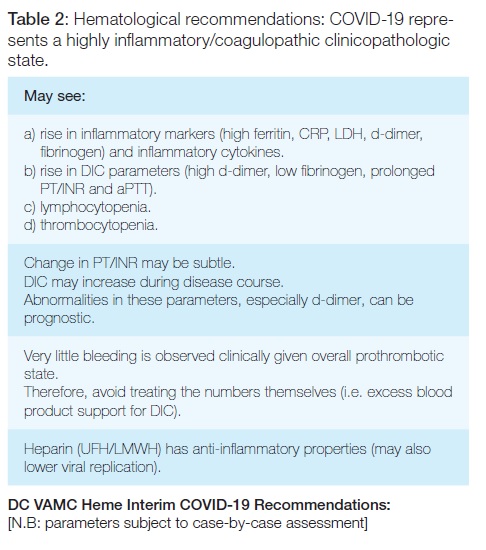
Much was and continues to be learned from ourcolleagues in China, Italy and Spain, as it pertains to clinical course, response to treatments, recovery. We learned from South Korea and Taiwan about preparation and preventions. The rapid dissemination of information has been, for the most part, beneficial allowing clinicians to veer off uncharted paths and ineffective approaches. We are all aware of the debates regarding ventilation. The debacle over the potential benefits of hydroxychloroquine, continues to this day. Medical societies have gathered and provide guidance for practitioners, with the caveat that this is a rapidly evolving field. We now know that this virus can cause a severe inflammatory reaction, akin to a cytokine storm and it is this late effect that often kills patients. This situation is particularly evident in Hematology; astute clinicians observed alterations in coagulation with consequent end-organ damage. A number of societies, including the American Society of Hematology and American Society for Thrombosis and Hemostasis, have issued guidelines for anticoagulation; in addition there is a plethora of recommendations form other hospitals, (Mount Sinai in New York, Emory in Atlanta, Beth Israel in Boston, among others) This is clearly an evolving field. At our institution we have created our own set of guidelines modeled on the more conservative recommendations, Table 2. Hopefully, data will soon accrue to help us in this area. Another area of great interest is the use of “recovery plasma” to treat infected and very ill patients. Although randomized data are lacking, early results suggest a beneficial effort in small cohorts. The American Red Cross together with the Mayo Clinic have stepped in to establish a registry of potential donors, as well as of the recipients. Again, questions regarding long-term efficacy, when best to administer and to whom, will need to be sorted out. In these times collaboration is essential and, we see the best of research, public health and clinical trial come together in a spirit of cooperation.
The Veterans Health Administration manages about 170 hospitals and 1063 clinics, caring for approximately nine million veterans. Most are middle-aged to older men with a number of comorbidities (diabetes, hypertension, chronic kidney disease, obesity, hepatitis C, etc.) that places them at higher risk. Many of the veterans come from ethnic groups that appear to be at higher risk (Blacks, Hispanics), but whether this is due to a different genetic make-up or to the presence of the co-morbid conditions described above is unknown. Our hospital in Washington DC, interestingly, is seeing less ill patients than some of the other local Institutions (Georgetown, George Washington), and that does not appear to be due to a migration of Veterans to those Institutions.
Table 3 shows the numbers of affected individuals. We have established triage clinics, separate from the ER (emergency room), rapid testing of all suspected cases and admission to negative pressure rooms for those who test positive and are ill. Individuals who are mildly symptomatic are sent home with appropriate recommendations. As the pandemic evolves, we have begun to test any patient admitted to the hospital and providing a clearly visible link in their EMR (electronic medical record) All staff are required to wear surgical type masks; those caring directly for COVID-19 patients have been issued and use N95 protective masks and other equipment. We are still in emergency mode, such that elective admissions/surgeries are being delayed.
Our laboratory department in currently evaluating various antibody tests; the hope is to have one available to identify “immunized” patients and eventually extend it to all hospital personnel. We have transitioned to a virtual modality of care, though we still see ill patients and those that require treatment, particularly chemotherapy or other biotherapies. Those individuals are at higher risk and we follow recommendations issues by the American Society for Clinical Oncology (ASCO).
What now and what next?
This pandemic has had major impacts on the US and world economy, creating a recession (4.8% drop in GDP) loss of jobs (more than 22 million), loss of health insurance and development/worsening of psychiatric illnesses. These will reverberate for decades to come. And yet, we are unclear as to whether the virus will reappear in the fall. With regards to this pandemic, much financial support is being provided to biotech and pharmaceutical companies to develop effective drugs and vaccines. Different approaches are being tried, and with scientific rigor, we will likely prevail. Interjection of politics, “fake news” and unproven theories have led to a bevy of approaches, from hydroxychloroquine to cleaning agents that are completely useless. Common sense and scientific approaches have the highest likelihood of success and together with careful reintegration of society, based preliminary on testing may allow us to a new normal.
ARE WE READY FOR THE NEXT PANDEMIC?
Perhaps we were lucky with this one. A more lethal and equally infectious pathogen could easily wipe out a large seg- ment of the population. We will need to restore the funding and hiring of experts that used to populate the White House. We will need to find/create “alarm bells” such as the ones used for approaching tsunamis, to alert us earlier of such infections. We will need to fight disinformation. And we should always make sure there is sufficient toilet paper available.
Can we look into the future? The words of Yogi Berra, a renowned baseball player came to mind “its tough to make predictions, especially about the future” but perhaps we will be better prepared. In the meantime, we will have to learn to live with this virus.
The statements included in this article are the opinions of the author and do not represent the views of the American government or its agencies.
REFERÊNCIAS
1. Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LF. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020 (in press). doi: 10.1038/s41577-020-0311-8. [ Links ]
2 Centers for Disease Control and Prevention (CDC).Coronavirus Disease 2019 (COVID-19) | [accessed 2020-04-30] Available from: http://www.cdc.gov coronavirus 2019-ncov. [ Links ]
3. Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF. The proximal origin of SARS-CoV-2. Nat Med. 2020;26:450-2. doi: 10.1038/s41591-020-0820-9. [ Links ]
4. Siddartha Mukherjee What the Coronavirus Crisis Reveals About American Medicine. New Yorker. 2020 May 4th issue. [ Links ]
5. U.S. Department of Veterans Affairs. Public Health. Novel Coronavirus Disease (COVID-19). [accessed 2020-04-30] Available from: https://www.publichealth.va.gov/n-coronavirus/ [ Links ]
Responsabilidades Éticas
Conflitos de Interesse: Os autores declaram a inexistência de conflitos de interesse na realização do presente trabalho.
Fontes de Financiamento: Não existiram fontes externas de financiamento para a realização deste artigo.
Proveniência e Revisão por Pares: Comissionado; sem revisão externa por pares.
Ethical disclosures
Conflicts of interest: The authors have no conflicts of interestto declare.
Financing Support: This work has not received any contribution, grant or scholarship.
Confidentiality of Data: The authors declare that they have followed the protocols of their work center on the publication of data from patients.
Provenance and Peer Review: Commissioned; without externally peer re-viewed.
© Autor (es) (ou seu (s) empregador (es)) 2019. Reutilização permitida de acordo com CC BY-NC. Nenhuma reutilização comercial.
© Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY- NC. No commercial re-use.
Correspondence/Correspondência:
Joao L. Ascensao - Joao.Ascensao@va.gov
Professor of Medicine, The George Washington University
Clinical Professor of Medicine, USUHS
Adjunct Professor of Medicine, Georgetown University
Chief, Hematology-Oncology Section DC VA Medical Center
Chair, ICR BOD
Washington, DC 20422
Received/ Recebido: 04/05/2020
Accepted/Aceite: 04/05/2020
Publicado / Published: 8 de Maiode 2020














