Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. vol.20 no.3 Lisboa maio 2013
https://doi.org/10.1016/j.jpg.2012.08.002
CLINICAL CASE
Endo-SPONGE® treatment for anastomotic leakage after colorectal surgery
Deiscência de anastomose após cirurgia colorectal - tratamento com Endo-SPONGE®
Nuno Velosoa,∗, João Dinis Silva a, Manuel Carvalhob, Isadora Rosaa, Isabel Medeirosa, Lurdes Gonçalvesa, Rogério Godinhoa, Celeste Viveirosa
a Department of Gastroenterology, Hospital Espírito Santo, Évora, Portugal
b Department of Surgery, Hospital Espírito Santo, Évora, Portugal
*Corresponding author.
ABSTRACT
Anastomotic leakage following colorectal surgery is a serious, fearful and the most important complication mainly after anterior resection of the rectum and is the main cause of postoperative morbidity and mortality. Endo-SPONGE (B-Braun Medical®), an endoluminal vacuum therapy minimally invasive, was shown to be an effective alternative in the treatment of colorectal anastomotic leakage with local infection in the minor pelvis. A case of endoscopic closure of anastomotic leakage is shown after anterior resection of the rectum using an endosponge and the role of this new device in the treatment of anastomotic leakage is discussed.
Keywords: Anastomotic leakage; Endo-SPONGE (B-Braun Medical®); Endoluminal vacum therapy
RESUMO
A deiscência da anastomose colo-rectal é uma complicação séria e temida após ressecção anterior do recto, sendo a principal causa de morbilidade e mortalidade pósoperatória. O Endo-SPONGE (B-Braun Medical®), terapia de vácuo endoluminal minimamente invasiva, mostrou ser uma alternativa efectiva no tratamento da deiscência da anastomose colorectal com infecção local na pélvis minor. Apresenta-se um caso de encerramento endoscópico de deiscência da anastomose colo-rectal, após ressecção anterior do recto, utilizando o Endo- SPONGE® e discute-se qual o seu papel no tratamento.
Palavras-Chave: Deiscência da anastomose colo-rectal; Endo-SPONGE (B-Braun Medical®); Terapia de vácuo endoluminal
Introduction
Anastomotic leakage following colorectal surgery is a serious, fearful and the most important complication occurring mainly after anterior resection of the rectum, with an incidence ranging from 1% to 24%.1
It is associated with a mortality rate between 6% and 22% and is found mostly in patients with distal rectal anastomoses and following neoadjuvant radiotherapy and/or chemotherapy.2
The classical treatment for these patients, if the peritonites is localized to the minor pelvis, is a conservative one (broad-spectrum antibiotic coverage and transrectal rinsing and drainage), until surgical rescue can be endeavored (loop colostomy or finally abdominoperineal extirpation) if the sepsis is not controlled.
However, there are no randomized and controlled trials in the literature to assess the best treatment and currently it depends on the extent and location of the anastomotic leakage as well as on the patients comorbidities.
In the last years, Endo-SPONGE® (B. Braun Aesculap AG, Germany), a minimally invasive endoluminal vacum therapy, has been shown to be an effective alternative in the treatment of colorectal anastomotic leakage with local infection in the minor pelvis.3-6
The Endo-SPONGE® is an open-pored polyurethane sponge with 7 cm in length and 3 cm in diameter that is cut according to the size of the wound cavity and placed transanally after diagnostic examination with a flexible gastroscope. Depending on the size of the cavity one or more sponges can be placed. An overtube and endoscope are inserted into the deepest point of the wound cavity. After removing the gastroscope the lubricated Endo-SPONGE® is placed through the overtube by using a pushing probe. The position of the sponges can be adjusted endoscopically. The sponge is subsequently connected to a low vacuum suction bottle (Redyrob Trans Plus®, B. Braun Aesculap AG, Germany) that is fixed to the skin of the buttock with adhesive tape. The Endo-SPONGE® allows continuous drainage, debridement and rapid cleaning of the presacral cavity, promoting the formation of granulation tissue, decreasing the size of cavity and healing of the presacral abscess.
We report a case of anastomotic leakage after anterior resection of the rectum which was successfully treated with Endo-SPONGE®.
Case report
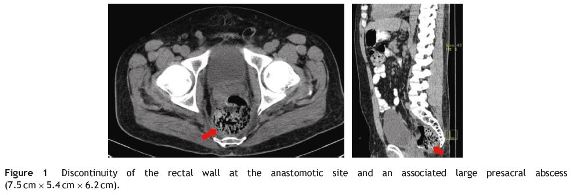
A 40-year-old man diagnosed with stage II (T3N1M0) rectal adenocarcinoma in April 2009 was submitted to neoadjuvant chemoradiotherapy before a low anterior sphincter-preserving rectal resection in August 2009. Eight days after the procedure, the patient developed fever (38.5 ◦C) and rectal bleeding. At this time a diagnostic CT scan of the abdomen and pelvis with intravenously administered contrast media was ordered and it revealed an anastomotic leakage with a large presacral abscess (7.5 cm×5.4 cm×6.2 cm) (Fig. 1).
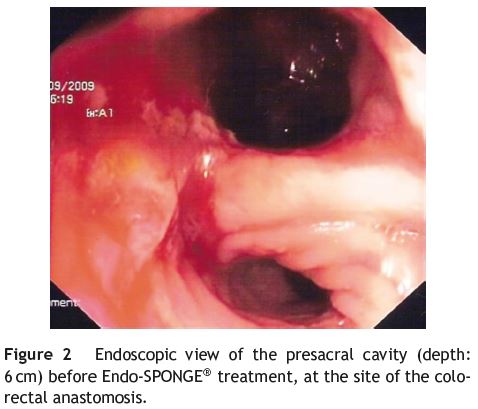
He was treated on broad-spectrum antibiotics and transrectal rinsing and drainage without clinical improvement. Thirty-three days after the initial surgery, a diverting loop ileostomy (double-barrel) was performed and on day 53 he began endoluminal vacuum therapy. Endoscopy before Endo- SPONGE® treatment showed anastomotic leakage of 180◦ of the internal circumference, 10 cm above the anal verge with the presacral cavity measuring 6 cm at the deepest point of the cavity (Fig. 2).
Endo-SPONGE® treatment was performed under mild sedation (midazolam 1 mg plus meperidine 25 mg) and using a small-caliber flexible gastroscope (GIF-145 Video Gastroscope, Olympus, 9.8mm diameter). After the initial two sessions the patient was discharged with the following procedures being conducted on an outpatient basis.
During the treatment sessions as the cavity reduced in size, being filled with granulation tissue, the size of the sponge used was also reduced to a length of 0.8 cm in the last session (Fig. 3).

Every two days a session was performed, except on weekends, with the sponges being exchanged to prevent the growth of granulation tissue into them and to reduce painful sponge exchanges.
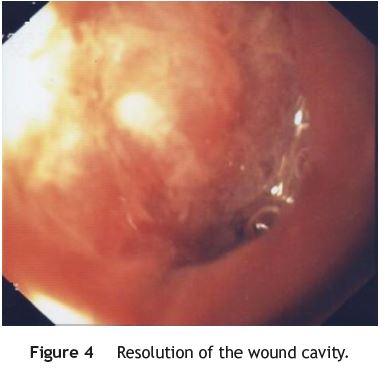
Thirty-four sponge exchanges were executed with a median number of sponges per session of two, ranging from one to three, without any particular complication (occasional bleeding in presacral cavity). The resolution of the wound cavity was achieved 75 days after the beginning of the treatment (Fig. 4).
In follow-up, 60 days after the end of treatment, a MRI scan (Fig. 5) showed only an organized fibrous tissue collection (1.2 cm×1.4 cm) without any evidence of abscess or fistula.

Diverting loop ileostomy could be closed 341 days after the beginning of the treatment, without complications.
Discussion
Vacuum-assisted closure therapy has been applied in surgery, for several years for complicated wounds (complex diabetic foot wounds, traumatic wounds, postoperative infected wounds) with good outcomes. Its beneficial effect on wound healing is related with an increase of blood flow, stimulation of granulation tissue formation and decrease of bacterial contamination.7,8 Recently Endo-SPONGE®, na endoluminal vacuum therapy, was introduced alike as a method for the treatment of anastomotic leakage after colorectal surgery, allowing continuous drainage, debridement and rapid cleaning of the wound cavity. It was shown to be an effective alternative in the treatment of colorectal anastomotic leakage with local infection in the minor pelvis.3-6
The main goal of any therapeutics for anastomotic leakage will be to close and drain the presacral cavity in the shortest period of time, since the prolonged pelvic sepsis and fibrosis are related with functional outcome after ileostomy closure.9 Continuous and effective drainage of the wound cavity plays a major role in the final outcome and it is ensured by the Endo-SPONGE® either by the negative pressure drainage system that bypasses the physiologic anal sphincter tonus or by the barrier effect that avoids permanent contact of infected secretions and gas with the perirectal tissue in the minor pelvis.
In 2008 Weidenhagen et al.4 described a series of 29 patients of which 28 (97%) achieved definitive closure in a median of 34 (range 4-79) days. One year later Von Bernstorff et al.10 showed closure of the presacral cavity in 23 of 26 patients (88.5%) with an average duration of 49.9 (range 10-221) days. Van Koperen et al.6 found inferior results with regard to the closure of the cavity (56%) in a series of 16 patients, which could be related to late onset usage of Endo-SPONGE®.
In our patient the number of days required until resolution of the cavity can be explained by three factors: the late onset of the vacuum therapy (number of days elapsed between the beginning of the therapeutic and colorectal surgery), the fact that the patient was submitted to neoadjuvant chemoradiotherapy and finally the size of the presacral abscess.
Van Koperen et al.6 showed that patients who promptly started Endo-SPONGE after colorectal surgery (<6 weeks), had higher closure rates of the presacral cavity than patients who started later (>6 weeks). On the other hand Von Bernstorff et al.10 demonstrated that patients who started endo-sponge following neoadjuvant treatment had significantly longer time (days) until closure of the presacral cavity, more sponge exchanges and larger cavities.
In the case that we report, the patient was submitted to a diverting loop ileostomy (double-barrel) with the aim of making fecal diversion to keep the wound clean and promote a faster healing. But was it really necessary? The Endo-SPONGE® is a vacuum-assisted closure therapy that obturates totally the presacral cavity preventing the communication of the sinus with fecal content. Weidenhagen et al.4 treated successfully five patients without performing a diverting stoma, requiring only in one case the creation of a stoma for infection control. Randomized controlled studies will be needed in this area.
Endo-SPONGE® placement can be helpful in the treatment of anastomotic leakage after colorectal surgery and may prevent chronic presacral sinus and avoid definitive colostomy.
References
1. Rullier E, Laurent C, Garrelon JL, et al. Risk factors for anastomotic leakage after resection of rectal cancer. Br J Surg. 1998;85:355-8. [ Links ]
2. Buchs NC, Gervaz P, Secic M, et al. Incidence, consequences, and risk factors for anastomotic dehiscence after colorectal surgery: a prospective monocentric study. Int J Colorectal Dis. 2008;23:265-70. [ Links ]
3. Nagell CF, Holte K. Treatment of anastomotic leakage after rectal resection with transrectal vacuum-assisted drainage (VAC). A method for rapid control of pelvic sepsis and healing. Int J Colorectal Dis. 2006;21:657-60. [ Links ]
4. Weidenhagen R, Gruetzner KU, Wiecken T, Spelsberg F, Jauch KW. Endoscopic vacuum-assisted closure of anastomotic leakage following anterior resection of the rectum: a new method. Surg Endosc. 2008;22:1818-25. [ Links ]
5. Mees ST, Palmes D, Mennigen R, Senninger N, Haier J, Bruewer M. Endo-vacuum assisted closure treatment for rectal anastomotic insufficiency. Dis Colon Rectum. 2008;51:404-10. [ Links ]
6. Van Koperen PJ, Van Berge Henegouwen MI, Rosman C, Bakker CM, Heres P, Slors JF, Bemelman WA. The Dutch multicenter experience of the endo-sponge treatment for anastomotic leakage after colorectal surgery. Surg Endosc. 2009;23: 1379-83. [ Links ]
7. Morykwas MJ, Argenta LC, Shelton-Brown EI, McGuirt W. Vaccum-assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg. 1997;38:553-62. [ Links ]
8. Argenta LC, Morykwas MJ. Vaccum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997;38:563-76. [ Links ]
9. Nesbakken A, Nygaard K, Lunde OC. Outcome and late functional results after anastomotic leakage following mesorectal excision for rectal cancer. Br J Surg. 2001;88: 400-4. [ Links ]
10. Von Bernstorff W, Glitsch A, Schreiber A, Partecke LI, Heidecke CD. ETVARD (endoscopic transanal vacuum-assisted rectal drainage) leads to complete but delayed closure of extraperitoneal rectal anastomotic leakage cavities following neoadjuvant radiochemotherapy. Int J Colorectal Dis. 2009;24:819-25. [ Links ]
Conflicts of interest
The authors have no conflicts of interest to declare.
*Corresponding author.
E-mail address: nuno_veloso@hotmail.com (N. Veloso).
Received 26 February 2012; accepted 1 May 2012













