Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. vol.20 no.5 Lisboa set. 2013
https://doi.org/10.1016/j.jpg.2013.04.004
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Autoimmune pancreatitis: A demanding clinical challenge
Pancreatite autoimune: um desafio clínico
Paulo Salgueiro∗, Ricardo Marcos-Pinto, Paula Lago, Isabel Pedroto
Gastroenterology Department, Hospital Santo António, Porto, Portugal
* Corresponding author
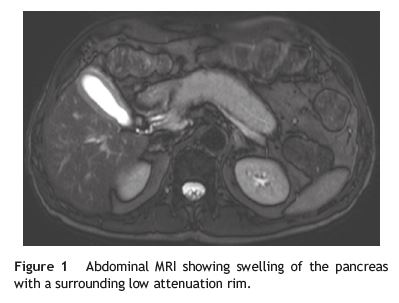
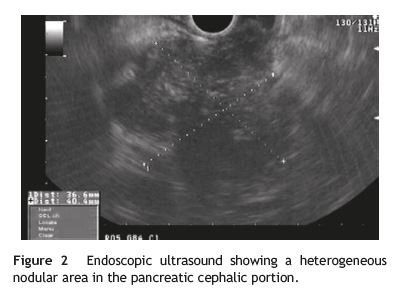
A 59-year-old man presented with a two-week history of epigastric pain associated with itching and jaundice. Laboratory investigation: direct bilirubin 15xN; alkaline phosphatase3xN; gamma-GT 6xN; glucose 2.5xN, and normal levels of both amylase and lipase. CT scan of the abdomen showed diffuse large pancreas with delay in the uptake of contrast product, as well as loss of normal pancreatic lobulation and a heterogeneous nodular area in the cephalic portion. Abdominal MRI revealed sausage like swelling of the pancreas with a surrounding low attenuation rim and a heterogeneous nodular area in the cephalic portion (Fig. 1). Endoscopic ultrasound confirmed the heterogeneity of the pancreatic cephalic portion with a 40mm nodule (Fig. 2). Aspiration cytology guided by endoscopic ultrasound was performed, and showed marked parenchymal lymphoplasmacytic infiltration, storiform fibrosis and obliterative phlebitis without malignant cells (Fig. 3A and B). Serologically, quantification of IgG subclasses allowed the discrimination of a raised IgG4 7xN. The diagnosis of autoimmune pancreatitis (AIP) was thus established, and the patient was proposed for corticosteroid therapy that, however, he has refused. A normalization of cholestatic enzymes was observed while the patient was still at the hospital and, after 8 months from diagnosis, the patient remains asymptomatic without any laboratory abnormality or evidence of involvement of other organs by the sclerosing process namely salivary glands, biliary tract, lungs, thyroid or kidneys.
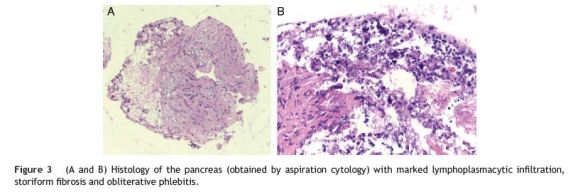
AIP is the pancreatic manifestation of a rare, systemic disease.1 Its diagnosis relies on a combination of clinical, serological, histological and imaging criteria.2 It is imperative to differentiate AIP from pancreatic cancer owing to the vastly different prognostic and therapeutic implications.1,2 In the case presented above features such as sex, age, symptoms, diabetes and typical imaging raised the suspicion of AIP that was then confirmed by the presence of an increased IgG4 and the exclusion of pancreatic cancer. Although the patient refused therapy with corticosteroids there was a complete clinical and laboratorial remission, which did not surprise us since, while therapy with corticosteroids is recommended especially for patients with obstructive jaundice,3 there have been reports of spontaneous resolution of pancreatic masses, strictures, and jaundice in the context of AIP.4
References
1. Zandieh I, Byrne MF. Autoimmune pancreatitis: a review. World J Gastroenterol. 2007;13:6327-32. [ Links ]
2. Finkelberg DL, Sahani D, Deshpande V, Brugge WR. Autoimmune pancreatitis. N Engl J Med. 2006;355:2670-6. [ Links ]
3. Hirano K, Tada M, Isayama H, Yagioka H, Sasaki T, Kogure H. Longterm prognosis of autoimmune pancreatitis with and without corticosteroid treatment. Gut. 2007;56:1719-24. [ Links ]
4. Ozden I, Dizdaroglu F, Poyanli A, Emre A. Spontaneous regression of a pancreatic head mass and biliary obstruction due to autoimmune pancreatitis. Pancreatology. 2005;5:300-3. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflicts of interest
The authors have no conflicts of interest to declare.
*Corresponding author
E-mail address: paulosalgueiro@gmail.com (P. Salgueiro).
Received 28 February 2013; accepted 13 April 2013













