Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Jornal Português de Gastrenterologia
Print version ISSN 0872-8178
J Port Gastrenterol. vol.21 no.4 Lisboa Aug. 2014
https://doi.org/10.1016/j.jpg.2013.06.002
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
An aggressive case of anorectal melanoma
Um caso agressivo de melanoma anorretal
Susana Marquesa,b,∗, Raquel Silvaa,b, Miguel Bispoa,b, Francisco Silvaa,b, Leopoldo Matosa,b
a Gastroenterology Department, Centro Hospitalar de Lisboa Ocidental, Lisboa, Portugal
b Medicine II Department, Centro Hospitalar de Lisboa Ocidental, Lisboa, Portugal
*Corresponding author
Introduction
All melanomas originate from the melanocyte. They may arise not only from the skin, but also from mucosal epithelium lining of the respiratory, alimentary and genitourinary tracts. Anorectal melanoma accounts for 1-3% of all anal tumors and 0.3% of all melanoma. The majority of cases arise from the mucocutaneous junction (dentate line).1,2
It usually occurs in the 5th or 6th decades of life. The most common presenting complaints are bleeding, anal pain or mass, pruritus, tenesmus and change in bowel habits. Weigh loss, anemia and fatigue may indicate metastatic disease. At presentation, 60% of the patients have lymph node involvement and 30% have distant metastases.
This very rare tumor can be classified into three different stages of disease progression: localized disease (I), regional lymph node involvement (II) and distant metastases disease (III), which account for a median survival of 24, 17 and 8 months respectively.3
Surgical resection is the gold standard treatment. Chemotherapy and radiation therapy alone have not been shown to be effective, but may provide some benefit when used as adjuvants. Despite treatment, the prognosis remains poor.4
Case report
This case presents a 55-year-old female patient with a past medical history significant for hemorrhoids and prior depression who was admitted to our medical facility for syncope. As associated symptoms, she reported intermittent rectal bleeding, usually after a bowel movement, and involuntary weigh loss over the past 6 months.
Due to family history of colorectal cancer in her father at the age of 47, she had had a total colonoscopy the year before which confirmed just internal hemorrhoids. She also had had CEA and CA 19.9 measurements two months prior to admission and both markers were within normal range.
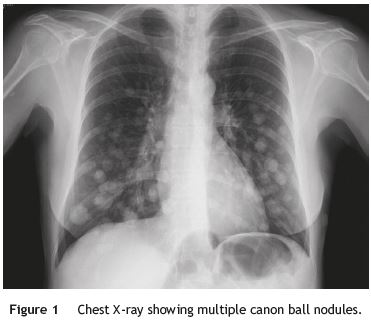
On physical examination, conjunctiva pallor was noted and digital rectal exam revealed a 5 cm rectal mass palpated 3 cm from the anal verge. Admission laboratory studies were significant for iron-deficiency anemia. Chest X-ray showed multiple bilateral pulmonary cannon ball nodules suggestive of metastasis (Fig. 1).
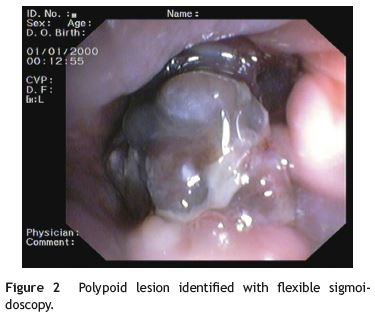
Flexible sigmoidoscopy was performed. A dark polypoid lesion measuring 5 cm in diameter was identified at the anorectal junction (Fig. 2). Histologically, tumor cells contained apparent brown pigment and were positive for S-100 protein and Melan-A immunohistochemical staining. These findings were consistent with the diagnosis of anorectal melanoma.
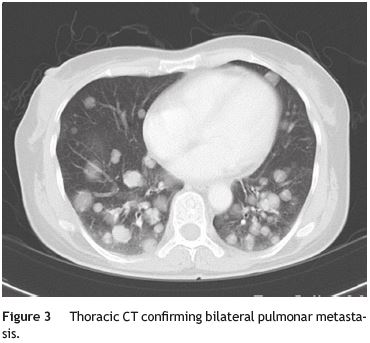
Tumor staging included standard head, thoracic, abdominal and pelvic CT imaging. Multiple bilateral pulmonar metastases of varying sizes were observed on thoracic CT (Fig. 3). In addition, head CT revealed six lesions involving the frontal and temporal lobes bilaterally, some showing necrotic degeneration. The greatest was 3 cm in diameter and presented extensive surrounding edema, causing lateral ventricular displacement (Fig. 4).
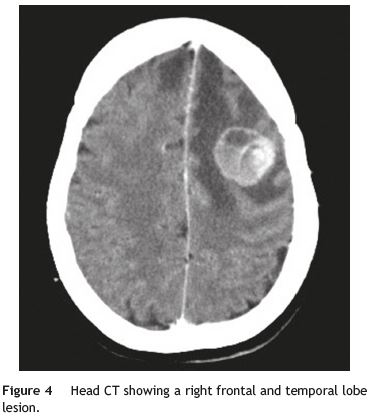
She was immediately placed on high dose corticosteroid therapy and prophylactic antiepileptic drugs. On day 5, she developed rapid focal progressive neurological deterioration with confusion, aphasia, right hemiparesis and sphincter control loss. Due to the advanced tumor stage, she was discharged and referred to a palliative care center just one week after admission. She passed away 8 weeks after the initial diagnosis.
References
1. Stefanou A, Nalamati SP. Anorectal melanoma. Clin Colon Rectal Surg. 2011;24:171-6. [ Links ]
2. Cagir B, Whiteford MH, Topham A, Rakinic J, Fry RD. Changing epidemiology of anorectal melanoma. Dis Colon Rectum. 1999;42:1203-8. [ Links ]
3. Iddings DM, Fleisig AJ, Chen SL, Faries MB, Morton DL. Practice patterns and outcomes for anorectal melanoma in the USA, reviewing three decades of treatment: is more extensive surgical resection beneficial in all patients? Ann Surg Oncol. 2010;17:40-4. [ Links ]
4. Singer M, Mutch MG. Anal melanoma. Clin Colon Rectal Surg. 2006;19:78-87. [ Links ]
*Corresponding author
Email address: xsusanamarx@gmail.com (S. Marques).
Ethical responsibilities
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflicts of interest
The authors have no conflicts of interest to declare.
Received 13 May 2013; accepted 10 June 2013













