Introduction
The publication of the report "To err is human: building a safer health care system" by the Institute of Medicine (IOM) in 2000 promoted a greater focus on health safety by revealing the high number of deaths resulting from clinical errors considered preventable, and the obvious problems of systems that aim to avoid them (Institute of Medicine, 2000). Given the impact of these data, in 2004, in response to the World Health Assembly Resolution 55.18, the World Health Organization (WHO) established the World Patient Safety Alliance, renamed WHO Patient Safety in 2009, to coordinate and accelerate global efforts to improve safety (World Health Organization, 2013).
Yet, current data shows that every year there is an unacceptable number of clients who suffer healthcare errors or die from a lack of safety and poor quality of care.
According to the World Health Organization, 1 in 10 clients is subject to errors resulting from the healthcare care process, of which at least 50% are considered avoidable (Jha et al., 2013; World Health Organization, 2017). Of these errors, 1/3 cause slight to moderate damage and 5% cause serious damage (World Alliance For Patient Safety, 2008).
Available evidence suggests that 134 million adverse events occur annually due to the lack of healthcare safety in hospitals in underdeveloped and developing countries, contributing to 2.6 million deaths over the same period (The National Academies Press, 2018 cit. by World Health Organization, 2018). These errors represent billions of euros of damage to healthcare systems worldwide and 15% of hospital activity and funding is consumed as a result of complications resulting from healthcare errors (Slawomirski, Auraaen, & Klazinga, 2017).
Safety, in accordance with the Conceptual Framework of the International Classification for Patient Safety, is defined as “reducing the risk of unnecessary damage to an acceptable minimum. An acceptable minimum refers to the collective notion in the light of current knowledge, available resources, and the context in which care was provided as opposed to the risk of nontreatment or another treatment.” (Directorate General for Health, 2011, p. 14 ).
Improving quality and safety of care is a common focus for managers, health professionals, policy makers and healthcare users (Schenk, Bryant, Van Son, & Odom-Maryon, 2018). But despite continued efforts to improve hospital safety, damage to hospital care persists (Institute for Patient and Family Centered Care, 2017; National Patient Safety Foundation, 2015; Schenk et al., 2018).
Among the strategies identified to promote quality and safety of healthcare is the recommendation to focus care on the client and their family and to involve both the client and family in this process (Institute for Patient and Family Centered Care, 2017; Institute of Medicine, 2001; World Health Organization, 2013).
Thus, “by placing the client and his family at the center, forces us to reinvent the health system (and the research logic itself) in a perspective increasingly based on aspects of citizenship and health gains.” (Sousa, Uva, & Serranheira, 2010, p.94) This recommendation is grounded in the fact that the client and family are the only ones who are continually present throughout the care process and the notion that, when involved and capable, can be critical to safer health care (World Health Organization, 2013). They are therefore an indispensable source of information on healthcare system failures (World Health Organization, 2013). An example of measures taken in this direction is the application of visiting policies in more open hospital institutions.
In 2005 WHO created the Patient Safety Program and its vision involves engaging, empowering, encouraging and facilitating clients and families to build and/or participate in the healthcare process, to partner with health professionals and policymakers to make health services safer, more integrated and client-centered (World Health Organization, 2013).
Accordingly, clients are increasingly included, not only in identifying adverse events, but also in participating in investigations to identify the causes of health safety problems (Zhu et al., 2011). In addition, healthcare professionals seek to partner with clients and families to improve quality and safety (Institute for Patient and Family Centered Care, 2013; World Health Organization, 2013).
When healthcare administrators, caregivers, clients, and family members work in partnership, quality and safety of healthcare increases, costs decrease, and worker and patient and healthcare professional satisfaction increases. (Institute for Patient and Family Centered Care, 2017).
However, some professionals view the presence of families and visitors as an obstacle to care, a reason to fear increased workloads and a risk to client safety (Bélanger, Bussières, Rainville, Coulombe, & Desmartis, 2017; Correia, 2017).
Despite the increase in patient satisfaction with these measures, the theoretical support developed and the institutional guidelines, it is clear that nursing care delivery is still client-centered and based on the biomedical model and that the family is not seen as the target of care (Martins et al., 2010; Oliveira et al., 2011; Schenk et al., 2018).
In short, there remain some antagonistic opinions by nurses regarding the value given to family involvement in the care provided, which is reflected in practice (Martins et al., 2010).
In this context, the involvement of the client and the family and its relationship with harm reduction is not well understood and thus, the objective of this paper is to develop a systematic review that allows us to recognize the existing evidence on the implications of family presence on the safety of the hospitalized client.
1. Methods
The systematic literature review aims to gather existing evidence respecting predetermined prerequisites in order to answer a specific research question (Donato & Donato, 2019; Oxman, Cook, & Guyatt, 1994). It involves systematic and explicit methods in order to gather primary studies of good quality, thus ensuring a high level of evidence that substantiates conclusions and decisions (Donato & Donato, 2019; Oxman et al., 1994).
In order to guarantee the accuracy and reproducibility that characterizes this type of research, the methods of research, selection and analysis are clearly defined in advance. Firstly, the research question should be established as well as the research objective, inclusion and exclusion criteria, the research methodology, databases to be consulted, the study selection methodology, the quality evaluation and the extraction of the data. To this end, it is beneficial to produce a research protocol that specifies these determinations to guarantee the consistency, transparency and integrity of the research, as is the case here (Donato & Donato, 2019).
In order to answer the research question: What are the implications of family presence for for inpatient safety?, we propose to develop a systematic literature review following the reference scheme (Fig.1) recommended by the Joanna Briggs Institute for systematic reviews prevalence and incidence (Aromataris, Munn, & Joanna Briggs Institute, 2017) and this protocol is registered with the JBI and the registration process with the International Prospective Register of Systematic Reviews (PROSPERO) has started.
1.1 Inclusion and exclusion criteria
This systematic review will consider studies in which participants are over 18 years old and hospitalized.
Therefore, studies conducted in the context of pediatrics and obstetrics will be excluded.
Studies that assess the impact of family presence on the safety of hospitalized patients will be considered, due to the occurrence of adverse events or quasi-events, in this sense, the intervention will be within the scope of optimizing the presence of the family in this context.
The current systematic review will consider studies comparing the presence of the family or interventions that optimize this presence with the lack of it or interventions that restrict this presence in relation to its implications for the hospitalized patient's safety.
In this sense, the possible outcomes of interest include all relevant indicators for patient safety: infections associated with healthcare, falls, pressure ulcers, identification errors, medication errors, surgical errors, frequency of notification of adverse events or almost events.
This review will include quantitative observational, analytical and descriptive studies published in the last 10 years, therefore from 2009 to the present, whose language is English, Portuguese, Spanish, French, German and Italian.
1.2 Research strategy
In the search strategy the terms to be used in the research according to the Health Sciences Descriptors (DeCS) are: Patient Safety, Nursing Care, Family and Hospitalization. In this case, the search phrase could be:: (Patient Safety) AND (“Nursing Care”) AND (Famil*) AND (Hospit*)
In the databases that use Medical Subject Headings (MeSH), the terms to be used will be: Patient Safety, Family, Family Centered Nursing and Hospitalization.
Free terms like family centered care can be used.
The databases for the research include: PubMed, Web of Science, CINAHL and Scopus. The search for documents that are not available in the usual ways of publication, known as grey literature, will be carried out in Open Grey, Grey Literature Report and Open Access Scientific Repository in Portugal (RCAAP).
Following the search, all identified citations will be uploaded to EndNote X9 reference management software and duplicates removed. Titles, abstracts, and keywords will be checked to exclude those that do not meet the inclusion criteria of this review. In the operationalization of this stage, two reviewers will be used to minimize the bias and ensure that relevant papers are not excluded. The third reviewer may be consulted in case of doubt or disagreement. Subsequently, the full texts are evaluated.
The evaluation of the methodological quality of the selected studies will be performed, once again, by two reviewers and using the tools recommended by JBI (Aromataris et al., 2017) in the evaluation of the reliability, relevance and results of the published articles. JBI's standardized critical assessment tools will be used depending on the study design: Critical Appraisal Checklist for Cohort Studies, Critical Appraisal Checklist for Case Control Studies, Critical appraisal checklist for analytical cross-sectional studies, Critical Appraisal Checklist for Case Series or Critical appraisal checklist for case reports. A cutoff score of 4 (four) is set for each JBI verification checklist, a score of 4 (four) to 6 (six) is considered moderate quality and higher than 7 (seven) indicates high quality. Studies with low methodological quality will be excluded. As described above, in cases of disagreement or doubt, the third reviewer should be consulted.
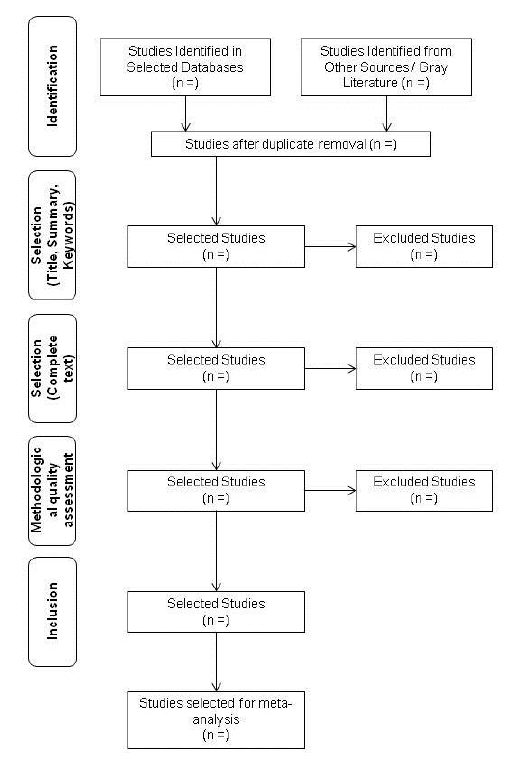
Figure 1 Blank flow diagram of the methodology of this systematic review based on JBI recommendations (Aromataris et al., 2017).
1.3 Data extraction and analysis
In the data extraction phase, the descriptive evaluation of each study will initially be made using the extraction instrument recommended by JBI (Aromataris et al., 2017). Information such as population, study methodology and results relevant to the research focus of this review will be included. Again, it will be done by two independent reviewers and the disagreements shall be discussed with the third reviewer.
The data will be presented in textual format and using tables. If the necessary conditions are met, a meta-analysis should be carried out by applying statistical methods to work together and summarizing the data from two or more studies and thus finding more accurate and comprehensive estimates than those presented by each study individually (Donato & Donato, 2019). This will be done, once again, using tools provided by JBI.
Conclusions
Considering the current customer safety issues, as well as the recommendations for the humanization of care, patient and family centrality and involvement of the latter in this process, it is important to understand, from a safety point of view, the implications of the presence of the family in this context.
In this sense, with this protocol we intend to meet the conditions to start the review research in order to know the current evidence on what the implications of family presence for the safety of the hospitalized patient.
As a result of this systematic review, we believe we may contribute to the knowledge and arguments for the theme of family involvement in the provision of hospital care in the context of client safety as well as potential guidelines for future investigations.
Understanding the impact of family presence on the safety of inpatients has the potential to influence family involvement and inclusion interventions in the context of hospital health care.














