Introduction
Guidelines for management of patients with ischemic acute stroke highlight the need for early assessment of any clinical condition that might negatively influence the outcomes, namely dysphagia (Powers et al., 2018). However, no recommendation on any screening tool is made resulting that, in Portugal, informal detection is frequently used by nurses in stroke units to screen dysphagia in acute stroke patients (Oliveira, Couto, & Mota, 2020). Several screening tools have been developed for patients with oropharyngeal dysphagia (Oliveira, Mota, Freitas, & Ferreira, 2019), but possibly due to its dietary recommendations, the Gugging Swallowing Screen (GUSS) is frequently used in clinical practice in acute stroke patients across several countries, with good validity and reliability (Park, Kim, & Lee, 2020). In an effort to provide stroke unit nurse’s a valid and reliable screening tool for dysphagia, and giving the reliability and validity of the original version of GUSS, a study was designed to translate, culturally adapt to the Portuguese language and test this screening tool in different stroke units.
1. Literature review
Stroke is currently the second leading cause of death in the world (World Health Organization, 2018). A common complication after a stroke is dysphagia, and its incidence in the acute phase can reach up to 80% (Takizawa, Gemmel, Kenworthy, & Speyer, 2016). The presence of dysphagia after a stroke is associated with an increased risk of pneumonia, dehydration and malnutrition, resulting in worse functional results and quality of life (Cohen et al., 2016). The gold standard for dysphagia assessment is videofluoroscopy swallowing study (VFSS), however, there are several limitations to perform it related to the patient’s ability to undergo an invasive procedure, availability of equipment and trained professionals to make the VFSS, making it impractical for routine use in clinical practice (Cohen et al., 2016). Consequently, swallow screening is considered the first step to identify patients at risk for dysphagia and therefore recommended for all acute stroke patients, as soon as clinically possible, after hospital admission and prior to any medication, fluids or food oral administration (Powers et al., 2018). There is growing evidence that suggest that early screening reduces the incidence of pneumonia and disability after stroke (Al-Khaled et al., 2016). In a study developed to determine the factors associated with hospital morbidity and mortality in stroke patients, the analysis of clinical records of 16 518 acute stroke patients indicated that two thirds of early mortality and worse results are attributable to non-modifiable factors, such as age and neurological deficit severity, however, pneumonia emerged as one of the main modifiable factors for poor prognosis, thus emphasizing the importance of intervention in this field in order to improve prognosis (Koennecke et al., 2011).
Several health assessment and measurement instruments have already been developed, many of which measure the same construct, developed for the same population and yet there are new ones being developed (Oliveira et al., 2019). So, the decision to adapt an instrument with documented validity, instead of creating a new one, proves to be effective and less time consuming, since cross-cultural adaptation is faster and is supposed to produce an equivalent measure (Amaral, Veiga, Pereira, Coelho, & Pereira, 2016). Choosing a health measurement instrument, in this case, a screening tool, depends on the consideration of several factors: clinical settings management and organization, patient related clinical aspects and the availability of health care professionals and resources (Donovan et al., 2013). Therefore, mainly due to its good psychometric proprieties, dietary recommendations and ease of use, it was considered the GUSS (Trapl et al., 2007) for translation, cultural adaptation and validation.
GUSS is a widely used screening tool for dysphagia in stroke patients in clinical practice across several countries and validity and reliability are known (Park et al., 2020). Sensitivity (97.0%), specificity (67.0%), inter-rater reliability (0.835) and area under the receiver operating characteristic curve (0.938) evidence good psychometric properties (Park et al., 2020; Trapl et al., 2007). The results of a review of eight studies pertaining GUSS that sought to investigate its validity and benefit, showed that screening performed by nurses using GUSS reduced screening time and pneumonia rate when compared to control the group, concluding that GUSS is a sensitive and reliable tool, however requiring further studies to confirm its effectiveness (Trapl et al., 2020).
2. Methods
The translation and cultural adaptation of a health measurement instrument implies its own methodology that guarantees the equivalence between the original version and the translated / adapted version, comprising a process that goes beyond literal translation, seeking to capture the existing meanings in the instrument (Wild et al., 2005).
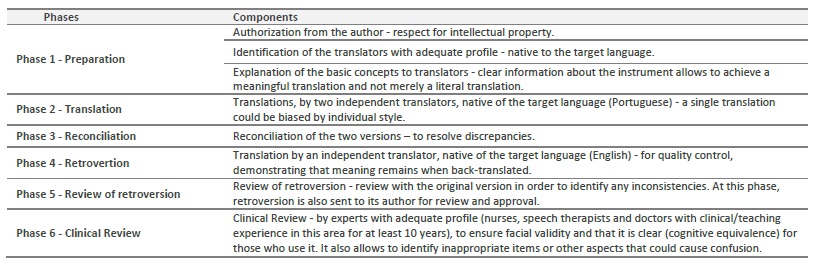
Once consent was obtained from the author, a translation and cultural adaptation plan was drawn that guided the whole process that considered the specificities of this type of instrument: it was developed for health care professionals use and its application requires adequate interpretation of the items used in it for correct use. This process was performed according to the International Society for Pharmacoeconomics and Outcomes Research principles of good practice (Wild et al., 2005) as summarized in table 1.
This study was approved by the ethics committee of the five hospitals.
2.1 Data collection
The Portuguese version obtained was then used in a prospective study conducted in stroke units of five hospitals from February of 2018 to April 2019. The inclusion criteria were defined in conformity with the original study: patients (over 18 years old) consecutively admitted to the stroke unit, with first ever stroke, either ischemic or hemorrhagic; confirmed by imaging; with no prior history of swallowing disorders; not previously screened for dysphagia or given any oral food or medication and that gave written consent (or by proxy whenever the patient was not able to provide consent). Stroke severity was assessed by National Institute Health Stroke Scale (NIHSS) and consciousness level with Glasgow Coma Scale (GCS) at time of unit admission. Other demographic and clinical data were collected: age, sex, stroke type, revascularization treatment (thrombolysis and/or thrombectomy), time from stroke onset to screening and risk factors.
For data collection GUSS was used, which is a two-part screening test. In the first part indirect swallowing items are tested (level of consciousness, saliva swallowing, voice changes, drooling and voluntary cough) that, if successfully achieved, leads to a second part, where swallowing items are tested (deglutition, coughing, drooling and voices changes), with different consistencies and volumes of semisolid, liquids and solid textures, in this specific order, in a series of sequential subtests. Scoring system attributes one point to items successfully achieved and zero to failed items. Each test and subtest comprise different items that must all be successfully performed to achieve the maximum score and move from the first to the second test and then from one subtest to the next. GUSS score produces four categories of severity: from zero to nine points patients are rated as severe dysphagia, from 10 to 14 as moderate, from 15 to 19 as mild, and 20 corresponds to no dysphagia. The cut-off of 19 identifies the risk of dysphagia and 14 the aspiration risk (Trapl et al., 2007). As optional recommendations, from scores of 19 or less, further functional assessments of swallowing, such as fibreoptic endoscopic evaluation of swallowing (FEES) or VFSS and referral to speech therapy are suggested. To be able to perform the test, patients must be able to sit in an upright position (or at least 60o), to understand simple orders and to perceive the screener’s face.
In each stroke unit, two experienced nurses, with over 10 years of clinical practice, and therefore considered experts, were recruited for data collection. Training was provided by the main researcher to all recruited nurses, including detailed explanation of specific procedures to administer the GUSS and the viewing of demonstrative videos of each subtest. Prior to data collection a one-month trial period was established so that the nurses would have the opportunity to administer the GUSS in order to improve the ability to perform it and clarify any doubts arising from its application. The GUSS was performed at bedside at admission to stroke unit according to the steps indicated in the original publication (Trapl et al., 2007) and patients were rated accordingly. Nurses were also asked to rate patients according to dysphagia severity (no dysphagia, mild, moderate or severe), based on their clinical judgement, prior to the administration of the GUSS. A second rater performed screening, blinded to the results of GUSS and clinical judgement within 24 hours of the first assessment, for inter-rater calculation purpose.
Considering that this study was not funded it was not possible to perform VFSS or FEES for criterion validity purposes. Nevertheless, researchers were authorized to access results of patient’s VFSS or FEES, if performed during hospital stay, which was not performed in any of the enrolled patients.
2.2 Statistical Methods
For statistical analysis IBM SPSS 25 for Windows was used. Descriptive analysis was performed for demographic and clinical data. Comparison between screening results using GUSS and the scores from NIHSS and GCS were reached using chi-squared analysis. Screening categorical data and results from clinical judgment were analyzed using qui-square test and the area under the receiver operating characteristic (ROC) curve, as a measurement of the accuracy of the test in general, was also calculated. Cohen’s kappa coefficient was used as an agreement measure. To note that internal consistency is not relevant in instruments in which items form a formative model, ie, the items together form the construct and do not need to be correlated (Mokkink at el., 2010). Therefore, the usual measures of internal consistency were not calculated.
3. Results
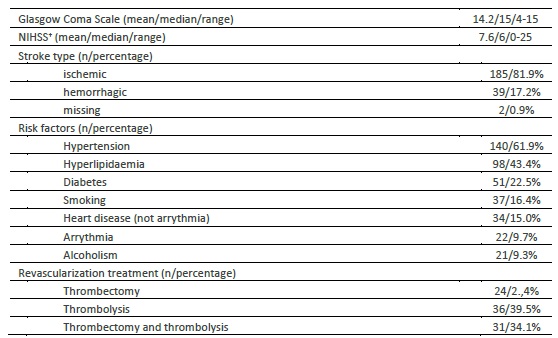
A total of 226 acute stroke patients were prospectively enrolled according to inclusion criteria and all patients, or proxy, gave written consent. The sample size results from the largest number of participants that could be enrolled during the period in which the study was authorized in each unit. The mean age of patients was 69.4±14.2 years (range 24-98) and 115 (50.9%) were male. None of the patients was submitted to VFSS or FEES during hospital stay. Most relevant patient’s clinical data are presented in Table 2. The majority of patients (n=117; 51.8%) were assessed in the first 24 hours after stroke onset and the remaining (n=109; 48,2%) up to 48 hours from stroke onset.
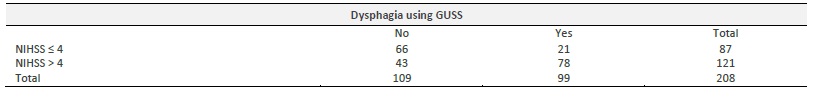
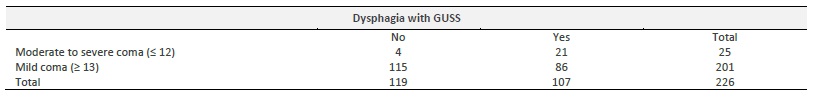
No complications occurred during the application of the GUSS and results show that 107 (47.3%) patients failed screen and therefore were identified as dysphagic. Detailing results according to dysphagia severity, 119 (52.7%) patients had a score of 20 and therefore rated as not dysphagic, four (1.7%) with mild dysphagia, 63 (27.9%) with moderate dysphagia and 40 (17.7%) with severe dysphagia. When the results obtained by the GUSS were compared with NIHSS results at a cut-off point of 4 (Henke, Foerch, & Lapa, 2017) and GCS scores, a very significant relationship was found: χ2 = 32.99; p <0.001; and χ2=15.15; p<0.001, respectively (table 3 and 4).
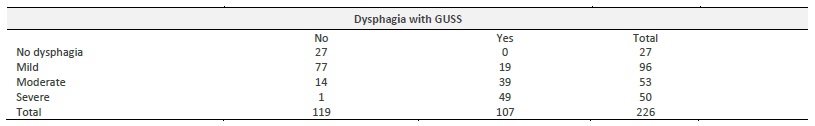
Patient’s dysphagia rating obtained by nurses’ clinical judgment was compared with screening results and a highly significant association was found (χ2=119.62; p<0.001), with 119 participants being identified as non-dysphagic by GUSS rated as no-dysphagia or mild dysphagia by stroke nurses (table 5).
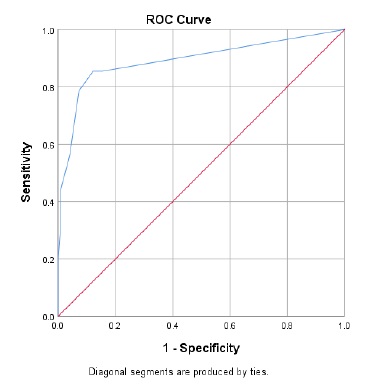
The area under the ROC curve (figure 1) was 0.892, which indicates a good predictive ability of the instrument in identifying the risk of swallowing impairment and sensitivity and specificity were respectively 85.4% and 84.6% for a cut-off point of 19 (dysphagia according to the GUSS score). For the cut-off point between 14 and 15 in the score (cut-off point for aspiration risk), an increase in specificity (92.7%) but with loss of sensitivity (78.6%) is obtained.
To determine inter-rater reliability, the application of the GUSS was repeated by a second rater within 24 hours, blinded to the result of the first assessment, to 42 (18.6%) patients. The reliability analysis test obtained excellent k values (k = 0.940).
Data available on request.
4. Discussion
Results show a high incidence of dysphagia in acute stroke patients, in line with previous results that show that it can reach up to 80% in the acute phase (Takizawa et al., 2016). Analyzing the participants with positive screening for aspiration risk (GUSS 0-14), an incidence of 45.6% was found. Despite that, the data show a lower incidence of aspiration risk compared to the one identified in the two groups included in the study by Trapl et al. (2007), which may be related to a lower mean of age of the participants, since age increases the incidence of dysphagia (Joundi et al., 2018). In the study by Trapl et al. (2007) data on the risk of dysphagia are not presented, however, in another study, an incidence of 83% was determined in all participants (Warnecke et al., 2017). In this study, people with mild neurological deficits (NIHSS ≤3) were excluded, resulting in a higher NIHSS mean score (7.6 vs 11.8), as well a higher mean age (69.4 vs 73.6) which may justify a higher incidence, thus making impractical the comparability of results.
Participants’ sociodemographic and clinical data corroborate the incidence found in the Portuguese population, with ischemic stroke having a higher incidence than hemorrhagic stroke, in a ratio of 1:4 (Direção-Geral da Saúde, 2017). Considering age and sex, these results are in line with the VALSIM study in which a higher prevalence of stroke in men (2.3% vs 1.9%) and an increase with age (Fiuza, Corte-Dias, Martins, & Belo, 2009) were found. These findings also highlight a high incidence of arterial hypertension, dyslipidemia and diabetes in the Portuguese population that are known important modifiable risk factors for stroke (Direção-Geral da Saúde, 2016; Fiuza et al., 2009).
Regarding further assessment for participants found to be at risk of dysphagia according to GUSS, none has been submitted to instrumental evaluation. Acknowledging that a screening test is not enough to diagnose dysphagia, a subsequent clinical and / or instrumental evaluation would be necessary to adequately identify dysphagic patients and establish adequate therapeutic plan, reducing the risk of pneumonia and hospital readmission (Powers et al., 2018; Virvidaki, Nasios, Kosmidou, Giannopoulos, & Milionis, 2018). Furthermore, only VFSS and/or FEES are effective to diagnose aspiration and accurately determine physiological and/or structural causes for dysphagia creating yet another obstacle to the definition of an adequate therapeutic plan (Powers et al., 2018). Costs and the lack of properly trained professional to perform VFSS and/or FEES are frequently identified as main barriers to access to instrumental assessment, however, these barriers are being questioned due to more significant costs attributed to the use of thickeners, enteral feeding, hospital readmissions for dysphagia complications and institutionalization (Cohen et al., 2016; Desai, 2019).
A statistically significant relationship was found between the positive screenings with the use of GUSS and the score >4 in the NIHSS, which reflects the association between increased neurological deficit and dysphagia, as previously acknowledge in different studies such as Henke et al., (2017), whose reference was used as a cut-off point for this study, but also by Joundi et al. (2018) in which patients with more severe stroke had a higher incidence of dysphagia.
Decreased levels of consciousness have also been associated with an increased risk of dysphagia (Joundi et al., 2018). In fact, it should be noted that the assessment of the level of consciousness is the first item to be evaluated in different screening tools for dysphagia, given the understanding that the patient must be awake, able to stand in upright position and comply simple instructions to be tested (Oliveira et al., 2019). The decrease in the level of consciousness in post-stroke patients can be caused, in a more acute phase, by extensive lesions with associated edema or, in a later phase, by delirium/disorientation, in which case the location and size of the lesion will be less important (Cohen et al., 2016).
The analysis of sensitivity and specificity measures, using clinical judgement as a reference, comparing with the results obtained for GUSS in the original study is not equitable because a different cut-off point was used. The values found for the area under the ROC curve are intermediate to the values found for the two groups in Trapl et a. (2007) study. In a systematic review with meta-analysis that sought to ascertain the validity and benefits of GUSS, pooled values of sensitivity, specificity and area under the ROC were found of 97.0%, 67.0% and 0.931, respectively (Park et al., 2020). A high sensitivity implies that the instrument has a high probability of tracking patients with dysphagia. It also adds that its use by trained professionals, such as nurses, reduces the incidence of pneumonia, decreases the length of hospital stay and the mortality rate (Park et al., 2020). The results now found, although inferior, especially for sensitivity, corroborate the good predictive ability of the GUSS to identify the risk of dysphagia. The difference in these findings can be explained by the use of clinical judgement as a reference, in contrast to the use of the results of instrumental evaluation. It is understandable that nurses in case of doubt, due to patient safety issues, mainly due to respiratory complications, chooses to classify the patient as dysphagic, following the evidence that suggests a prioritization of the respiratory complications by professionals in dysphagic patients (Cohen et al., 2016) and reinforcing a higher incidence of dysphagia using clinical assessment (Martino et al., 2005).
The results obtained for inter rater reliability were higher to those achieved in the GUSS original study (k=0.940 vs k=0.835), with an almost perfect level of agreement between raters. These results may be explained by the fact that all nurses who participated in the data collection have had intensive training prior to the administration of the GUSS. In fact, the rigorous prior training and regular monitoring of the evaluators has shown to be a valid strategy in improving the competences of the evaluators, increasing the reliability among observers (Glanzman et al., 2018). Excellent results of reliability among raters were also achieved, with a value of k=0.955 for the validation study in the Turkish population (Umay et al., 2018), corroborating the results now obtained.
Conclusion
Evidence suggests that early screening in stroke patients reduces the incidence of pneumonia and this study is the first known attempt to validate a dysphagia screening tool for acute stroke patients for the Portuguese population. These findings suggest that the Portuguese version of the GUSS is a simple and easy to use screening tool, adequate to administer at bedside by nurses that, with adequate training, shows good sensitivity and excellent reliability. These characteristics make it an important asset to assist nurses in the decision-making process to refer stroke patients to a more comprehensive assessment, therefore making it an option for nurses to use in their clinical practice. The main limitations of this study, mainly due to financial constraints, are the lack of instrumental evaluation for a more accurate calculation of criterion validity and first rater not blinded for clinical judgment results, that was sought to minimize with the second rater. Researches also acknowledge that despite no adverse events occurred during the GUSS application, data on other outcomes such as pneumonia and death were not reported. Further research must be directed to reinforce the validity and reliability of this screening tool for acute stroke patients aiming to strengthen these findings.