Introduction
Evidence-based practice is an approach that encourages the development and/or use of results in clinical practice. Due to the immensity and complexity of evidence produced in the health area, there is a need to create literature review methods that systematize the clinically relevant findings so that this information is more easily accessible and constitutes effective support to the process of decision-making of health professionals, managers, and politicians (Kuiper, O’Donnell, Pesut & Turrise, 2017). In this context, mindful of the skills of nurse-midwives in monitoring low-risk pregnancy (European Parliament and Council, 2005), it is known that currently, in the Portuguese context, these pregnant women, whom a nurse-midwife could accompany, are accompanied by family doctors, guided by a pre-defined program by the General Directorate of Health (Direção-Geral da Saúde, 2016). Despite the bureaucratic and formal issue of organizing the provision of maternal health care in Portugal, it is important to understand whether this organization will not result in an under-utilization of these professionals' skills, with implications for the accessibility and quality of care provided to these women/couples. The profitability of the nurse-midwives’ skills would free up family doctors for other care activities for which only they have the skills to develop. The results obtained from the investigation can help managers and politicians in the decision-making process for a more efficient allocation of human resources available in our health services and for health professionals to have adequate and up-to-date evidence on the information to be provided to pregnant women to make an informed and conscious decision regarding the follow-up of their pregnancy. Therefore, considering the background, the objective of this study is to identify the benefits of monitoring pregnancy by nurse-midwives to ensure robust scientific evidence of the benefits of uncomplicated pregnancy follow-up by nurse-midwives, achieving higher quality and timely health care.
1. Theoretical framework
The nurse-midwife corresponds to the designation in European legislation with the term "Midwife" (Ordem dos Enfermeiros, 2010). The word midwife derives from the word childbirth which comes from the Latin Parere and means “to be born”. Commonly known as the woman who assists at births, we now know that being a midwife is more than assisting at births. Thus, through European Directive 36/2005/CE, the specific competencies of the nurse-midwife were defined, including taking care of the woman in the family and the community in family planning and during the preconception period, the prenatal period, during the work of childbirth, and the postnatal period and all other periods of sexual and reproductive life that women go through during the life cycle. In the aforementioned legislation, we also find the responsibilities assumed by nurse-midwife in their professional practice. They assume autonomous interventions in all low-risk situations, in which physiological processes and normal life processes are involved in the woman's reproductive cycle. In medium and high-risk situations, in which pathological and dysfunctional processes occur in the reproductive cycle, they work collaboratively with other health care providers (European Parliament and Council, 2005). In woman-centered care, the nurse-midwife assumes the role of its advocate, allowing her to make her own decisions, supporting her in her informed choices, encouraging her autonomy, and offering diverse impartial information that helps in her decisions, covering her beliefs and values and that is non-judgmental (Ordem dos Enfermeiros, 2015). The role of midwives in countries such as Sweden, for example, has shown a positive birth experience and fewer medicalized births, increasing health promotion by following up women of childbearing age from an earlier age (Hildingsson, Karlströmb & Larsson, 2021).
Traditionally, in Portugal, until 1980, labor was a low-resource event that took place at home. After the revolution in 1974, the restructuring process began, resulting in a healthcare system based on the British National Health Service (NHS), supported by the construction of a network of hospitals. This restructuring resulted in the monitoring of pregnant women and their respective labor led by obstetricians, which saw a drastic reduction in perinatal mortality (White & Queirós, 2018). Currently, the ratio of doctors per 100 thousand inhabitants is 555 (Pordata, 2021), which is above the European average, and that of nurses is below the European average (Organização para a Cooperação e Desenvolvimento Económico, 2019). This ratio of doctors/nurses has implications for health care. While in other countries, maternity centers led by midwives have evolved, both inside and outside hospitals with positive maternal and neonatal outcomes, in Portugal, these centers do not exist (White & Queirós, 2018).
Although in Portugal the autonomous surveillance of normal pregnancy is carried out by family doctors and obstetricians (Assembleia da República, 2012), in the last two decades there has been an increase in professionals specialized in Maternal and Obstetric Health Nursing, who support childbirth in hospitals and more childbirth preparation programs (Carneiro, 2004). The lack of accessibility to nurse-midwives’ consultations and how health services are organized, without any reimbursement, for example, lead to pregnant women being followed by obstetricians (White & Queirós, 2018). As a result, the pregnant woman's desire that the doctor present at the time of delivery is the same one who accompanied her during the pregnancy resulted in a phenomenon "scheduling" of the day of delivery, increasing the rates of cesarean sections (White & Queirós, 2018) among other unforeseen interventions. In Portugal, as well in many other countries all over the world, a woman with a low-risk pregnancy, understood as one in which normal physiological processes and life processes are included in the woman's reproductive cycle, is usually accompanied by her family doctor, except when the pregnant couple opts for another type of follow-up, such as a private doctor.
2. Methods
To carry out this study, a secondary investigation was chosen through an integrative literature review (Sousa, Marques-Vieira, Severino & Antunes, 2017), which would allow mapping the current evidence to answer the following research question: What benefits can be obtained from the follow-up of pregnancy by nurse-midwives compared to the same follow-up carried out by doctors?
Once the research focus of attention was identified, the starting question was formulated, for which the acronym PICO was used, which defines, according to Galvão & Pereira (2014), the population (pregnant/parturient); the intervention or exposure (follow-up by nurse-midwife); comparison (follow-up by a physician) and the outcome (benefits). Subsequently, an initial search was carried out in the main health sciences descriptors - Medical Subject Headings, which allowed defining the terms used in the research, which were combined with the Boolean operators OR and AND. The research was conducted between January and August 2021, in three distinct databases: PubMed, CINAHL and Scielo, which were freely accessible within the institution where the authors work and were considered the most accurated for answering the research objectives, using the following Boolean phrase: ((("prenatal care") OR ("maternity care")) AND (("midwifery) OR ("nurse-midwives")) AND (("childbirth") OR ("parturition"))). Search strategy for Pubmed was performed between July 20th and August 8th 2021, with 86 results according to: (((“prenatal care”[Title/Abstract]) OR “maternity care” [Title/Abstract]) AND (midwifery[Title/Abstract] OR “nurse-midwives”[Title/Abstract]) AND (childbirth[Title/Abstract]) OR parturition[Title/Abstract]))) [MeSH Terms] Filters: English; Portuguese; Spanish; Publication Date from 2015/01/01 to 2021/07/31.
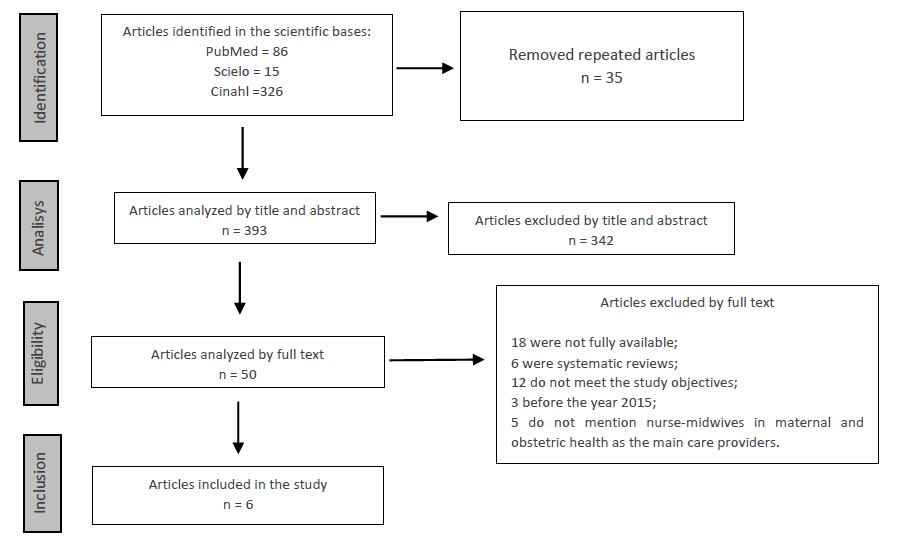
For this research, the following inclusion criteria were defined: a) primary studies, b) studies published between 2015 and 2021, thus seeking to translate the most recent scientific evidence, c) articles published in English, Portuguese or Spanish; and d) available full text. The different phases of the research are shown in the PRISMA diagram (Page et al., 2021), shown in figure 1.
The first search was limited to the last five years; however, due to the reduced number of papers retrieved, two more years were added to the time limit search to strengthen results. For data extraction, a matrix was developed to collect the following information: year and authors, country where the study was conducted, objectives and study design, and results. The search and selection of the articles were made by two reviewers independently according to the inclusion criteria and research question.
Once the selection of the articles was completed, the assessment of the methodological quality of each of them was carried out by three researchers, using the instruments proposed by the Critical Appraisal Skills Program (CASP) (Long, French & Brooks, 2020), which present 12 questions, which allow the evaluation and interpretation of the evidence, focusing on three domains: validity, results, and relevance to clinical practice. Only articles complying with at least nine (75%) items of the CASP tool would be included. When there was no unanimous consensus on the quality evaluation on any of the items of the evaluation instrument used, it was decided to classify them as "not achieved". In the assessment of methodological quality, all articles presented at least nine affirmative answers for the set of 12 questions under evaluation, concluding that they had a methodological quality to be included in the review. Quantitative analysis of the results was planned, and in case this was not possible, a synthesis and qualitative appreciation were determined.
3. Results
All retrieved articles were considered to have the adequate methodological quality to be included in the review, as they met at least 75% of the CASP items. The methodological procedures allowed us to identify six studies for analysis. Of the included studies, two were cohort studies (E1, E2), three randomized controlled clinical trials (E3, E4, E5) and one using the modified grounded theory methodology (E6). Of the six studies analyzed: two were carried out in 2018 (E1, E2); one in 2017 (E3), one in 2016 (E4), and two in 2015 (E5, E6). The locations where the studies were carried out cover two countries: five studies in Australia (E2, E3, E4, E5, E6) and a study in the United States of America (E1). Concerning study participants: three studies defined women with low-risk pregnancies as inclusion criteria (E1, E4, E5), one study used women who were pregnant when there was a sudden flood in the city where they lived (E2), one study used pregnant women afraid of childbirth (E3), and the final one (E6) used pregnant women who chose to receive maternal care from a private nurse-midwife. After choosing the six articles, a table was created with a summary of the results of those articles (Table 1). We excluded studies with poor reporting and/or whose CASP methodological assessment indicated a high risk of bias to avoid potential biases.
Table 1 Summary of selected articles.
| Authors | Year | Objectives | Study design | Participants | Results |
|---|---|---|---|---|---|
| E1. Weisband, Y., Klebanoff, M., Gallo, M., Shoben, A. & Norris, A. | 2018 | To compare birth interventions and maternal and neonatal outcomes among women with low-risk pregnancies who receive antenatal care from a nurse-midwife and antenatal care by a physician. | Retrospective cohort study. | A total of 8779 low-risk women who gave birth to a singleton infant between January 2012 and December 2015, who had attended at least one prenatal care visit either a physician or a midwife prior to 20 weeks’ gestation. | The number of women who experienced induction of labor, episiotomies, or epidurals was significantly lower among pregnant women who received antenatal care from a nurse-midwife. A significantly smaller difference in women who had cesarean sections or had premature births in pregnant women accompanied by a nurse-midwife in antenatal care. |
| E2. Simcock, G., Kildea, S., Kruske, S., Laplante, D., Elgbeili, G. & King, S. | 2018 | To assess whether the monitoring of the pregnant woman by a nurse-midwife affects the baby's neurological development at six months, in the context of a natural disaster. | cohort study | The study included 115 women that received one of two models of maternity care: midwifery group practice or standard hospital maternity care. | Even during a natural disaster, babies of mothers whom a nurse-midwife accompanied scored better on the age and stage Questionnaire (ASQ-3) in two of the five domains (fine motor skills and problem-solving). |
| E3. Toohill, J., Callander, E., Gamble, J., Creedy, D. & Fenwick, J. | 2017 | To determining the cost-effectiveness of a psycho-education led by a nurse-midwife for pregnant women afraid of childbirth. | Randomized controlled clinical trial | 339 pregnant women were screened for childbirth fear. | With minimal additional costs to the healthcare system, pregnant women can receive personalized care from a nurse-midwife that improves emotional health, confidence and increases the rate of spontaneous vaginal births. |
| E4. Forster, D., McLachlan, H., Davey, M., Biro, M., Farrell, T., Gold, L., Flood, M., Shafiei, T. & Waldenstrom, U. | 2016 | To investigate the effectiveness of care delivery led by a nurse-midwife in assessing the pregnant woman's satisfaction in antenatal, intrapartum, and postpartum care in the hospital or at home. | Two-arm randomized controlled clinical trial | 2314 pregnant women at low risk of complications were randomized to caseload midwifery or standard care. | For pregnant women with a low risk of medical complications, follow-up led by a nurse-midwife increases women's satisfaction in antenatal, intrapartum, and postnatal care. |
| E5. McLachlan, H., Forster, D., Davey, M., Farrell, T., Flood, M., Shafiei, T. & Waldenstrom, U. | 2015 | To determine the effect of monitoring the pregnant woman led by a nurse-midwife on the woman's experience in childbirth. | Randomized controlled clinical trial | A total of 2314 low-risk pregnant women. | Women in the intervention group had better results in the following aspects: positive experience of childbirth in general, birth control, coping physically and emotionally, feeling proud of themselves, feeling the freedom to express their pain. |
| E6. Davison, C., Hauck, Y., Bayes, S., Kuliukas, L. & Wood, J. | 2015 | To describe the pregnant women's reasons for choosing to be accompanied during pregnancy by a nurse-midwife. | Modified Grounded Theory | The sample comprised 14 women who had received maternity care from a privately practicing midwife within the previous five years. | Pregnant women value working together with their nurse-midwife to share a common goal of natural birth, studying the different pregnancy monitoring options preferring a personalized model to the pregnant woman rather than focusing on medical constraints. |
4. Discussion
The results presented were subdivided by the advantages found to expose the collected data, linking them between the different articles for better systematization.
Lower cesarean rates / Increased spontaneous vaginal deliveries
Cesarean sections, despite being sometimes necessary and life-saving surgeries, when performed without medical justification, can put the woman and baby at risk, bringing health problems in the short and long term. The cesarean rate has been increasing worldwide without showing significant benefits for the health of women or their babies (World Health Organization, 2018). Recognizing that it is an urgent problem, the World Health Organization (WHO) in 2018 launched new guidelines for non-clinical interventions to reduce the number of unnecessary cesarean sections. Key recommendations include educational programs for women and partners to make an informed decision based on the type of birth to be performed, and these programs are made up of a multidisciplinary team led by midwives. In studies E1 and E3 the data suggest that pregnant women, when accompanied by nurse-midwife, are less likely to have a cesarean delivery (34% lower risk of having a cesarean birth (E1) and 2.34 times the odds of having a vaginal birth (E3)). A study by Rosenstein, Nijagal, Nakagawa, Gregorich, & Kuppermann (2015) followed a community hospital for nine years in which women coming from private insurance with a private doctor switched to a 24-hour midwifery follow-up model, with cesarean rates between nulliparas, multiparas, full-term infants, and vaginal delivery after cesarean, purchased before and after the change of follow-up model. The results of this study indicate that changing follow-up is associated with decreased rates of cesarean deliveries and increased rates of vaginal births after cesarean delivery. A study carried out by Gama et al. (2016) in Brazil compared hospitals that used the physician-led follow-up model and nurse-led follow-up models in performing vaginal deliveries. The results of this study indicate that the participation of nurses in antenatal and intrapartum care has a positive impact, including reducing cesarean rates. In the same line, in a study carried out by Valadan et al. (2015), quality of life was similar in both groups of vaginal delivery and Cesarean section, namely which focused on physical, psychological, social, and environmental aspects as well as individual’s general view of life and personal health. Therefore, authorities in charge of health programs can have a leading role in changing people's delivery concept and developing a positive attitude towards vaginal delivery. This could be achieved through effective public training schedules.
Reduction in premature births
It was also identified a relationship between the monitoring of pregnant women by nurse-midwives and the decrease in the number of preterm births (E1) (5.3% compared to 11.4% with similarly low-risk women who received prenatal care from a physician). A study by Allen, Kildea & Stapleton (2016), using data from births between 2008 and 2012 and interviews carried out with women who received follow-up care by nurse-midwives and the respective nurses who carried out a follow-up, indicates that the follow-up by nurse-midwives influences pre-births-term for promoting earlier monitoring of pregnancy, effective prenatal care, reduced use of tobacco and substances, optimal gestational weight gain, better emotional health for pregnant women, and fewer untreated urinary tract infections. The WHO, faced with the problem of increasing preterm birth rates, launched guidelines on how to act to reduce these rates. Among these guidelines comes the monitoring of pregnant women led by a midwife, which has been shown to reduce preterm birth rates by up to 24% (World Health Organization, 2018).
Reduction of interventions performed during childbirth
Interventions performed during the time of delivery such as episiotomies, use of epidural analgesia, induction, or increase in labor are less likely to occur when the pregnant woman was accompanied by nurse-midwives (E1, E5): 13% lower risk of having their labor augmented, 33% lower risk of having their labor induced, and 31% lower risk of having epidural analgesia during labor, and significantly associated with reduced odds of having an episiotomy compared with similarly low-risk women who received prenatal care from a physician. There is evidence that midwife-led monitoring of pregnant women is associated with low rates of birth interventions among women with low-risk pregnancies (de Jonge et al., 2017). McLachlan et al. (2012) used women with low-risk pregnancies whose pregnancy monitoring was led by a midwife. This study suggests that monitoring the pregnant woman led by a midwife is related to a reduction in analgesia during childbirth and a reduction in episiotomies. This study is consistent with the systematic review carried out by the Cochrane Library (Sandall, Soltani, Gates, Shennan & Devane, 2016) that compares the follow-up carried out by nurse-midwives to other types of follow-up for pregnant women and where one of the main results is the decrease in instrumental deliveries, use of epidurals, and need to perform episiotomies. A recent literature review proved that in pregnant women followed by the midwife model, there was a significant correlation in the reduction of medical interventions, including surgical deliveries, epidurals, performing either amniotomy or episiotomy and a more significant number of vaginal deliveries (Alves, Mendes, Azevedo & Correia, 2019).
Better pregnant emotional health
All studies have in common (E1-E6) that a healthy pregnant woman, who feels listened to and valued, is much more likely to have a more comfortable birth without having to resort to interventions during this. When accompanied by nurse-midwives, pregnant women report receiving personalized care, adapted to their problems and fears (E3, E5, E6). This characteristic means that pregnant women are in pain control, obtaining a more positive experience of the moment of delivery (E4, E5). Fear of the moment of delivery is one of the factors that most influence the well-being of pregnant women and one of the main reasons why the rate of cesarean sections per request has been increasing (Fenwick et al., 2015). A study by Hildingsson, Rubertsson, Karlström & Haines (2018) analyzed the effectiveness of monitoring pregnant women by midwives dedicated only to monitoring pregnant women in reducing the fear of childbirth. These researchers questioned pregnant women mid-way through pregnancy, late in pregnancy, and two months postpartum, using scales to assess fear of childbirth pain. After collecting these data, questionnaires were sent to assess the degree of satisfaction of pregnant women with the service provided by midwives. The results show that 8 out of 10 women received all prenatal and intrapartum care by a midwife they already knew, with the majority having a vaginal birth without the need to resort to analgesic drugs. The degree of satisfaction was high, and most women reported that the fear of childbirth disappeared or decreased with monitoring by midwives. Fenwick et al. in 2015 analyzed the effects of psychological education by midwives in pregnant women afraid of childbirth on their postpartum psychological well-being. The results of this study suggest that women who received follow-up by midwives compared to pregnant women who received traditional family doctor follow-up have lower rates of C-sections and emergency C-sections and fewer flashbacks at the time of delivery, indicating that the support received by the midwife helped in decreasing the development of trauma associated with childbirth.
In conclusion, the analyzed studies suggest that the follow-up of pregnant women by nurse-midwives encompasses the woman in a holistic perspective, demonstrating concern beyond the physical aspect, ensuring that pregnant women maintain physical and psychological well-being to face a new phase in their lives. It may also improve breastfeeding rates and support the identification and prevention of postnatal depression. Interventions that offer continuity of support beyond birth may therefore improve longer-term outcomes (Symon, 2016). Alves, Mendes, Azevedo & Correia (2019) demonstrated that pregnancy followed by the midwife model results in three times more satisfaction with the care provided and twice more with care during labor and delivery. Pregnant women felt greater control over the labor and, with greater emotional and physical coping and self-pride, were less anxious, more at ease to express their feelings, declaring a better birth experience.
Conclusion
This study was able to identify the most current evidence, suggesting substantial benefits for low-risk pregnancies when followed by nurse-midwives. The benefits were a reduction in cesarean rates, an increase in spontaneous vaginal deliveries, a reduction in preterm births, and the reduction of interventions performed during childbirth, such as episiotomy, epidural analgesia, induction, and better emotional health of the pregnant woman. Despite the limited number of studies retrieved, we believe that we were able to respond to the initially proposed objective. To note that outcomes and outcome measurement methods were different across studies.
The main limitations of this review are the search limitation to three languages and only three databases, which may have resulted in missing evidence, and the reduced number of studies retrieved and included for review, which prevents the generalization of the results obtained. Another recognized limitation is that the participants included in this review are low and medium-risk pregnant women, which translates into heterogeneity of the study population. More evidence on the benefits of a woman with a physiological pregnancy followed by nurse-midwives must be developed to validate the results suggested in this study.
The results of this literature review may be useful for health professionals to have adequate and up-to-date evidence on the information to be provided to pregnant women to make an informed and conscious decision regarding the follow-up of their pregnancy.
Revision articles
E1: Weisband, Y., Klebanoff, M., Gallo, M., Shoben, A., & Norris, A. (2018). Birth Outcomes of Women Using a Midwife versus Women Using a Physician for Prenatal Care. J Midwifery Womens Health, 63(4), 399-409. https://doi.org/10.1111/jmwh.12750
E2: Simcock, G., Kildea, S., Kruske, S., Laplante, D., Elgbeili, G., & King, S. (2018). Disaster in pregnancy: midwifery continuity positively impacts infant neurodevelopment, QF2011 study.BMC Pregnancy Childbirth, 18, 309. https://doi.org/10.1186/s12884-018-1944-5
E3: Toohill, J., Callander, E., Gamble, J., Creedy, D., & Fenwick, J. (2017). A cost effectiveness analysis of midwife psycho-education for fearful pregnant women - a health system perspective for the antenatal period.BMC Pregnancy and Childbirth, 17(1). https://doi.org/10.1186/s12884-017-1404-7
E4: Forster, D., McLachlan, H., Davey, M., Biro, M., Farrell, T., Gold, L., Flood, M., Shafiei, T., & Waldenström, U. (2016). Continuity of care by a primary midwife (caseload midwifery) increases women’s satisfaction with antenatal, intrapartum and postpartum care: results from the COSMOS randomized controlled trial.BMC Pregnancy and Childbirth, 16, 28. https://doi.org/10.1186/s12884-016-0798-y
E5: McLachlan, H., Forster, D., Davey, M., Farrell, T., Flood, M., Shafiei, T., & Waldenström, U. (2015). The effect of primary midwife-led care on women's experience of childbirth: results from the COSMOS randomized controlled trial.BJOG: An International Journal of Obstetrics & Gynaecology, 123(3), 465-74. https://doi.org/10.1111/1471-0528.13713
E6: Davison, C., Hauck, Y., Bayes, S., Kuliukas, L., & Wood, J. (2015). The relationship is everything: women׳s reasons for choosing a privately practicing midwife in Western Australia.Midwifery, 31(8), 772-8. https://doi.org/10.1016/j.midw.2015.04.012