Social anxiety disorder (SAD) refers to intense, persistent, and disproportionate fear and/or anxiety when facing social exposure and possible evaluation by others, namely in social interaction (e.g., having a conversation, meeting unfamiliar people), observation (e.g., while eating or drinking) and performance (e.g., doing a presentation or speaking in public) situations (American Psychiatric Association, 2013). Such fears have been associated with various actions, namely avoidance and safety behaviors. These actions intend to protect the self from feared social outcomes that are seen as probable, threatening, and catastrophic (Piccirillo et al., 2016).
SAD has its more frequent onset during adolescent years, with estimated prevalence rates varying between 8.6% (Burstein et al., 2011) and 9.1% (Merikangas et al., 2010) in the USA. A recent study in Portugal indicates similar prevalence rates (i.e., 9.4% in a school-based sample of adolescents; Alves, et al., 2022). It usually follows a chronic course if left untreated (Keller, 2006), particularly for those adolescents who perform worse in social events (Miers et al., 2013). SAD entails self-perceived meaningful impairment in several domains of the adolescents’ everyday life, namely higher levels of anxiety and avoidance when interacting with peers or potential romantic partners, as well as when called to take part in academic activities (Rao et al., 2007). Also, adolescents with SAD perceive themselves to have poorer social skills; such poorer social performance is corroborated by observing others (Inderbitzen-Nolan et al., 2007; Rao et al., 2007), including their peers (Miers et al., 2010), in comparison with non-socially anxious adolescents. Avoidance and safety seeking behaviors may be partly the reason why adolescents with SAD experience poorer social outcomes (McNeil et al., 2010).
Avoidance behaviors have a substantial role in maintaining social anxiety (McManus et al., 2008) because they are negatively reinforced, by allowing a removal, prevention, or delay in the exposure to feared social situations and the discomfort they elicit (Piccirillo et al., 2016). When avoidance is not possible, socially anxious individuals frequently resort to safety behaviors (Halldorsson & Creswell, 2017; McManus et al., 2008) to manage the impression they are making on others (Plasencia et al., 2011). These safety behaviors may assume different forms. They may focus on trying to go unnoticed thus inadvertently bringing about feared consequences (e.g., social disconnection from others). They may also take the form of striving for an optimal social performance, which, if achieved, is attributed solely to the practice of safety behaviors (Piccirillo et al., 2016). In both cases, social anxiety and the actions used to cope with it are sustained.
Thus, avoidance and safety behaviors appear as relevant intervention targets to consider with those suffering from SAD (McManus et al., 2008; McNeil et al., 2010). Such a behavioral approach to SAD should include behavior exposure and training of skills that may enhance the positive reinforcement obtained from exposing oneself to feared social stimuli (McNeil et al., 2010). In fact, the inclusion of social skills training has been found to heighten benefits following cognitive-behavioral treatment for SAD (Scaini et al., 2016). As such, some intervention approaches for SAD combine cognitive strategies [e.g., realistic thinking (Warner et al., 2007) or cognitive challenging (Spence et al., 2000)] with exposure and social skills training. The Social Effectiveness Therapy (SET; Beidel et al., 2014), however, focuses solely on exposure and social skills training, which may more directly address the negative interactions in which adolescents with SAD get involved (Blöte & Westenberg, 2007). Specifically, the SET includes group sessions that train the individual in how to act in diverse social events (e.g., take the initiative, perform in public, maintain conversations) and individual sessions where they are exposed to their worst social fear until anxiety levels subside (Beidel et al., 2014). Given that social skills deficits related to social anxiety seem to be present specifically for children and adolescents (Levitan & Nardi, 2009), an approach that most directly tackles these difficulties seems particularly relevant for adolescent SAD.
Though initially designed for adults, the SET has a version conceived for children and adolescent (i.e., SET-C; Beidel et al., 2007), which has been successfully applied to this population (Mesa et al., 2014) and has led to lessened self-reported social anxiety (Beidel et al., 2007; Olivares et al., 2002) and avoidance (Beidel et al., 2007). These therapeutic changes are superior to a pharmacological treatment (Beidel et al., 2007) and similar to the standard cognitive-behavioral group treatment (Olivares et al., 2002). Still, it is a very intensive intervention (at least 24 sessions over a 12-week period), and hence possibly less applicable or appealing to non-treatment seeking samples (i.e., adolescents taken from schools who are diagnosed with SAD), of which, nevertheless, over 65.7% would be available to receive treatment if offered (Alves et al., 2022). Shorter interventions may be more appealing to adolescents with SAD, who, similarly to adults with SAD, might be reluctant to seek treatment (Griffiths, 2013).
Therapeutic gains on SAD symptoms have been observed for cognitive-behavioral intervention as short as 4 sessions (Gallagher et al., 2004), but the specific changes arising from a short stand-alone behavior approach to SAD have not, to our knowledge, been addressed before. This paper intends to explore the change in self-reported social anxiety, avoidance, and practice of safety behaviors, following a brief group behavioral therapy approach (see the Intervention Approach section below) based on the SET-C, in comparison with a waiting-list control group and using a pre- to post-intervention design. This shorter and more focused intervention approach may be an appealing, developmentally relevant, and cost-effective way of addressing adolescent SAD. We expect that adolescents taking part in the intervention will self-report diminished social anxiety, avoidance, and practice of safety behaviors from pre- to post-intervention, like previous findings based on interventions focusing on exposure and social skills training (i.e., SET-C, Beidel et al., 2007). We also expect that change to be more noticeable for the intervention than the waiting-list group. As a secondary goal, considering the role that avoidance and safety behaviors are proposed (McNeil et al., 2010) and were found to have (McManus et al., 2008) in maintaining social anxiety, this work will also explore if post-social anxiety might be predicted by change in avoidance and/or practice of safety behaviors, in addition to pre-intervention social anxiety.
Method
Participants
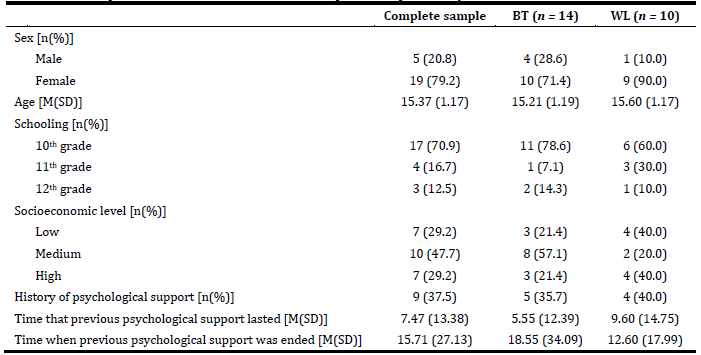
Participants were 24 adolescents with a primary diagnosis of SAD, aged 14 to 18 years old (see Table 1). They were randomly allocated into a Behavioral Therapy condition (BT; n = 14) or to a Waitlist condition (WL; n =10). Their sociodemographic characteristics were then compared. Participants in the BI and WL were equally prevalent by sex (ꭓ2(1) = 1.22, p = .27), schooling (ꭓ2(3) = 4.36, p = .23), socioeconomic level (ꭓ2(2) = 3.31, p = .19), and having previously received psychological support for their difficulties (ꭓ2(1) = 0.46, p = .83). They also had similar mean ages (z = -0.93, p = .40). Also, those who had a history of psychological support, had had it for a similar number of months (z = -0.21, p = .86) and that experience had been finished for a similar number of months (z = -0.67, p = .61).
Instruments
Recruitment measures. The Social Anxiety Scale for Adolescents (La Greca & Lopez, 1998; Portuguese version by Cunha et al., 2004) was used to screen for students that might present high levels of social anxiety. It is a self-report questionnaire consisting of 22 items answered using a 5-point Likert scale ranging from “1 - not at all” to “5 - all the time”. Each participant’s response to 18 of those items can be interpreted using a total measure and/or three subscales (i.e., fear of negative evaluation from others, discomfort or avoidance in new social situations, and generalized social discomfort and avoidance in peer interaction); 4 items are neutral and not considered when interpreting results. Its original (La Greca & Lopez, 1998) and Portuguese (Cunha et al., 2004) versions have shown good internal consistency. For the current study, using the Portuguese version of the instrument and considering data provided by Cunha et al. (2004), students scoring one standard deviation above the mean on this instrument’s total score were called for individual assessment to verify compliance with the inclusion and exclusion criteria (see the Sampling subsection below).
The M.I.N.I-KID - Mini International Neuropsychiatric Interview for Children and Adolescents (Sheehan et al., 1998; Portuguese version Rijo et al., 2016) is a structured clinical interview that assesses mental disorders commonly found in childhood and adolescence based on the diagnostic criteria defined in Diagnostic and Statistical Manual of Mental Disorders - DSM. Its Portuguese version was applied individually in space made available by the school by trained psychology Master graduates to assess for the primary diagnosis of social anxiety disorder, and for the absence of psychotic symptoms or current counseling for social anxiety.
Outcome measures. The Social Anxiety and Avoidance Scale for Adolescents (Cunha et al., 2008) was originally developed in Portuguese and studied with Portuguese adolescents to assess social anxiety and avoidance of feared social events. It is a self-report questionnaire that includes 34 items listing social situations specifically relevant to adolescents. Each item is answered twice, one for anxiety using a Likert-type response scale ranging from ‘1 = none’ to ‘5 = very much’, and another for avoidance using a Likert-type response scale varying from ‘1 = never’ to ‘5 = almost always’. Previous studies have ascertained this instrument’s psychometric quality, namely internal consistency and test-retest reliability, construct validity in relation to anxiety and depression, and discriminant validity of SAD in comparison with other anxiety disorders and normal controls (Cunha et al., 2008). Its internal structure has also received ample evidence as organized in six measures that are non-coincident for the anxiety and avoidance constructs (Cunha et al., 2008; Vagos et al., 2014). Given the similarity of our samples’ age to the work of Vagos et al (2014), measures were computed according to those authors’ recommendations. The measures are, according to Vagos et al. (2014): Interaction in New Social Situations including 4 items for anxiety (i.e., scores range from 4 to 20) and 3 items for avoidance (i.e., scores range from 3 to 15); Interaction with the Opposite Sex including 5 items for anxiety and avoidance (i.e., scores range from 7 to 15); Performance in Formal Social Situations including 4 items for anxiety (i.e., scores range from 4 to 20) and 5 items for avoidance (i.e., scores range from 5 to 25); Assertive Interaction including 6 items for anxiety and for avoidance (i.e., scores range from 4 to 20); Observation by Others including 7 items for anxiety (i.e., scores range from 7 to 35) and 4 items for avoidance (i.e., scores range from 4 to 20); and Eating and Drinking in Public including 2 items for anxiety (i.e., scores range from 2 to 10) and 3 items for avoidance (i.e., scores range from 3 to 15). Its original Portuguese version was used in the current study.
The Assertive Interaction measure was not used in the data analyses, due to it having achieved unacceptable internal consistency values. For the other measures, at least acceptable internal consistency values were found at pre- and post-intervention using the current sample: α ≥.68 for anxiety and α ≥.83 for avoidance of Interaction in New Social Situations; α ≥ .83 for anxiety and α ≥ .52 for avoidance of Interaction with the Opposite Sex; α ≥ .83 for anxiety and α ≥ .53 for avoidance of Performance of Formal Social Situations, α ≥ .57 for anxiety and α ≥ .67 for avoidance of Observation by Others, and α ≥ .70 for anxiety and α ≥ .67 for avoidance of Eating and Drinking in Public.
The Safety Behaviors in Social Situations for Adolescents (Silva et al., 2011) was originally developed in Portuguese and studied with Portuguese adolescents to assess the frequency with which safety behaviors were practiced in feared social events. It is a self-report questionnaire including 17 items that are answered using a Likert-type response scale varying from ‘1 = never’ to ‘4 = almost always’. Its internal structure is organized into a single factor with possible values ranging from 17 to 68. Its scores have presented good internal consistency and temporal stability. They have also proved to be sensitive to discriminating between adolescents presenting with SAD and non-anxious adolescents and between pre- to post-treatment differences (Silva et al., 2011). Its original Portuguese version was used in the current study and achieved at least good internal consistency for all assessment moments within the current sample (i.e., α ≥ .76)
Procedure
Sampling. Four schools in the north and center regions of Portugal were selected, based on geographical convenience (i.e., proximity to the host institution) and on providing secondary level teaching. They collaborated in recruiting participants for this research during the school year of 2016/17, after the study was approved by the General Directorate of Education and the Ethics Committee of the host institution. Schools further attained written informed consent from parents/ legal guardians of students, which explicitly stated the stages and procedures of the study, the confidentiality of individual data, and the potential risks for participants in the intervention (i.e., discomfort when facing feared social events) that would be appropriately addressed by a trained psychologist. Parents/ legal guardians also had access to the contact information of the responsible researcher if they wanted to clarify any doubts. Students who had parental/ legal consent were further asked for verbal assent to take part of this research. Only those who assented were integrated into the specific recruitment procedures described below. Inclusion criteria were being a student enrolled in the 10th or 11th grade at the time of screening and then having a primary diagnosis of SAD established via clinical interview. 12th graders are part of this sample because they changed school year between the screening and the intervention. Exclusion criteria were being enrolled in the special needs school system, currently receiving counselling for social anxiety, and/or presenting with psychotic symptoms at the time of enrollment.
Recruitment considered the following stages. Firstly, the 257 students attending the 10th and 11th grades who had parental consent and assented to participate were screened for social fears using the Social Anxiety Scale for Adolescents (Cunha et al., 2004). They were also asked to fill in a sociodemographic questionnaire developed by the research team at this time. Information taken from this questionnaire was used to characterize the sample. Secondly, 52 students scoring one standard deviation above the mean on that scale according to national normative data (Cunha et al., 2004) were called for individual assessment using the MINI-KID (Rijo et al., 2016). Finally, 24 participants who received a primary diagnosis of SAD in that interview were invited to take part in the study, if also complying with the other inclusion and exclusion criteria stated above. Right after the interview, these participants were asked to fill in the outcome self-report protocol in written format. This corresponded to the pre-intervention assessment which took place roughly one week before intervention started. Participants were then randomly allocated to either BT or to WL. Three BT groups were conducted with 3 to 5 participants per group in space made available by the school and were led by one doctor in psychology and one psychologist in training. All participants from the BT and the WL were asked to fill in the same post-intervention protocol. The post-intervention happened roughly eight weeks after pre-intervention (i.e., six weeks of intervention happened between assessment moments), at a pre-arranged time and place in the school, in the presence of the evaluator. After post-intervention assessment, participants in the WL were invited to take part in BT; three refused to do so.
Intervention Approach. The current BT-SAD intervention was based on the SET approach to SAD, and so focused on social skills training and exposure. Unlike the SET, exposure was carried out in group sessions, with group members performing specific roles to represent each other’s fears. Specific behavioral intervention strategies were used to facilitate exposure, namely diaphragmatic breathing, progressive muscle relaxation, self-positive reinforcement, and counterconditioning in relation to the antecedents of feared social events. Additional information on the intervention, including each sessions’ dynamics, will be provided by the corresponding author upon reasonable request.
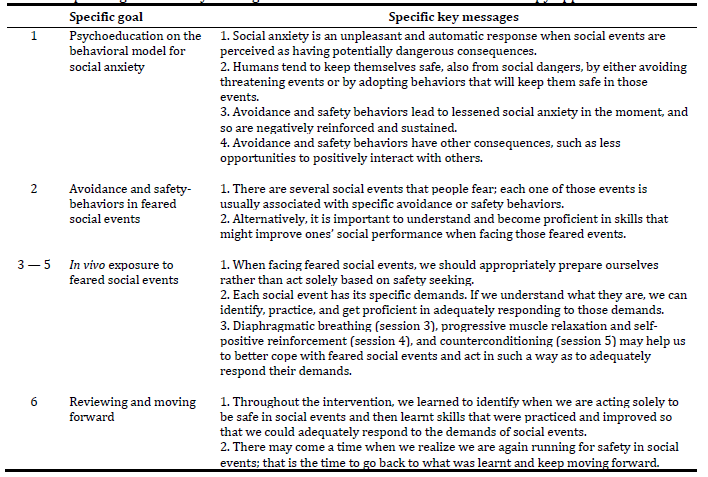
BT-SAD consisted of six weekly sessions delivered in person, each lasting approximately one hour. Each session consisted of two dynamics that were designed to accomplish specific goals and convey specific key messages (see Table 2). Sessions covered the following themes: psychoeducation of social anxiety as a fear response that is reinforced/ maintained by the practice of avoidance and safety behaviors (session 1); developing a fear hierarchy and discussing the avoidance and safety behaviors usually practiced in each feared situation (session 2); practice of social skills and adjustment of the practice of safety behaviors and then promotion of in vivo exposure to feared situations (sessions 3, 4 and 5); and finally reviewing contents, competences and how to continuously apply them (session 6). Sessions 3 through 5 included training in skills related to symptom management when performing behavior exposure (i.e., diaphragmatic breathing, progressive muscle relaxation, positive self-reinforcement) and in social skills training. The later was tailored to the specific demands of the events feared by members of each group. Trained social skills included: starting and maintaining conversations with others; expressing disagreement with another person’s opinion or with the way one is being treated by others; dealing with criticism from others; apologizing and/or asking for help; performing in front of others; and giving and receiving praise from others.
Data Analyses. Descriptive analyses were used for describing our sample, in total and differentiated by groups. Concerning gender, schooling, socioeconomic level and history of psychological support, the number of participants and its corresponding percentage was presented. Mean and standard deviation was presented for age, and time that previous psychological support lasted and when it ended. Furthermore, groups were compared across these variables: chi-square analyzes were conducted to ascertain for the (dis)similar distribution of participants by group based on sex, socioeconomic level, and having previously received psychological support for their difficulties, whereas Mann-Whitney analyzes were carried out to compare means for age, time that previous psychological support lasted and when it ended across groups.
Preliminary results are presented that explored how pre- and post-intervention scores for the outcome measures (i.e., anxiety, avoidance, and practice of safety behaviors) were associated with age and timing of psychological support. Preliminary results also refer to analyses of differences on those variables based on sex, schooling, socioeconomic level, and history of psychological support. Most measures followed a normal distribution, with three exceptions [i.e., social anxiety felt when interacting in new social events at the pre-intervention stage (W= .91, p = .03); post-intervention eating and drinking in public at (W = .86, p = .01) and the pre-intervention practice of safety behaviors (W = .89, p = .02)]. Still, given our sample size, non-parametric tests were used for these preliminary analyses. Specifically, the Mann-Whitney test was used for comparing outcome measures by gender and having or not having had previous psychological support and the Kruskall-Wallis test was used when comparing outcome measures by schooling and socioeconomic level. Spearman correlation analyses were carried out to assess the association between the outcome measures on the one hand, and age and timing of psychological support, on the other.
Mixed ANOVAs were used to evaluate change following BT: they allow comparison between CT and WL (i.e., between-subject effect) from pre- to post-intervention (within-subject effect) and the way these overtime changes may vary by group (i.e., interaction effect), and have no non-parametric equivalent. The Greenhouse-Geiser correction was applied whenever the sphericity assumption was refuted; and the Levene test showed homogeneity of variance for all measures. This method is necessary to accomplish the goals of the current research, and has been previously used to study changes following a brief cognitive-behavioral approach to SAD with a similar sample size (Gallagher et al., 2004). A priori analyses using the Gpower software show that, for a sample of 24 participants and power analyses set at .08, only large effect sizes would be found (i.e., > .40).
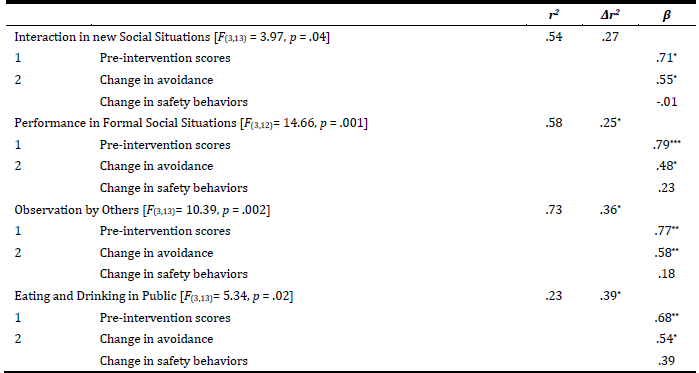
Hierarchical regression analyses were used to investigate variables predicting post-intervention social anxiety. Pre-intervention social anxiety was entered as a predictor in the first step, and the change in avoidance and in the practice of safety behaviors from pre- to post-intervention were entered as predictors in the second. A priori analysis using the Gpower software show that, for a sample of 14 participants using three predictors and power analyses set at .80, only large effect sizes would be found (i.e., > .35).
Because participants were asked to fill in the self-report protocol in written format when an evaluator was present, the evaluator was able to check for missing responses and request them to be filled in by the participant; hence, we had no missing values. All analyses were carried out using the IBM SPSS Statistics 26.
Results
Pre- and post-intervention outcomes by sociodemographic variables
No significant differences were found for any outcome measure between boys and girls, between students from different school years, and between participants who had or did not have a history of receiving psychological support. Similarly, outcome measures did not correlate significantly with age or duration of previous psychological support.
Significant differences were found between participants coming from diverse socioeconomic levels at the pre-intervention stage for anxiety when eating and drinking in public [H(2) = 7.33, p = .03] and avoidance of interacting in new social situations [H(2) = 6.85, p = .03]. Likewise, significant differences were found post-intervention based on socioeconomic level for anxiety when eating and drinking in public [H(2) = 9.27, p = .01]; anxiety when being observed by others [H(2) = 12.35, p = .002]; avoidance of eating and drinking in public [H(2) = 10.42, p = .005]; avoidance of interacting in new social situations [H(2) = 6.42, p = .04]; and avoidance of being observed by others [H(2) = 15.91, p < .001]. Participants from the medium socioeconomic level had the lowest scores, followed by those from the high level and finally participants from the low level.
Change in outcome measures from pre- to post-intervention assessment
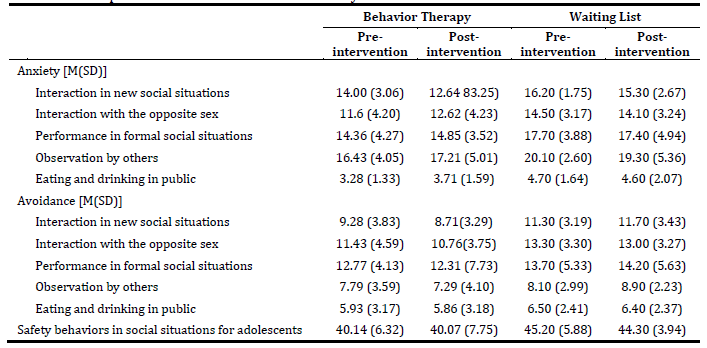
Descriptive results for all outcome measures at pre- and post-intervention are presented in Table 3. For anxiety, significant group mean level differences were found only for interacting in new social situations [F(1,22) = 4.14, p = .05, ƞ2 = .16 for assessment moment and F(1,22) = 5.57, p = .03, ƞ2 = .20 for condition]. Participants had similar mean scores at the pre-intervention stage (p = .05) but differed at the post-intervention (p = .04). Mean scores decreased from pre- to post-intervention for both groups (see Table 3). A similar result was found for avoidance of interacting in new social situations; though only the condition effect was close to statistical significance [F(1,22) = 2.53, p = .07, ƞ2 = .14). Post-hoc comparisons place that between-group difference at post-intervention (p = .04) but not at the pre-intervention stage (p = .19).
Predictors of post-intervention social anxiety scores
Pre-intervention social anxiety was a significant predictor of the variance of post-intervention social anxiety. Additionally, change in avoidance scores and in practice of safety behaviors significantly contributed to increasing that variance for performing in formal social situations, being observed by others, and eating and drinking in public. Specifically, pre-intervention scores and change in avoidance of those situations were significant predictors of the variance of post-intervention scores; change in practice of safety behaviors was not. For anxiety felt when interacting in new social situations, the contribution of change in avoidance or safety behaviors to explaining variance in post-intervention social anxiety was not statistically significant, although the model including all predictors was (Table 4).
Discussion
The current study intended to explore change outcomes from pre- to post- intervention grounded on a brief behavioral approach to SAD in adolescence. This approach is based on the premise that avoidance and safety behaviors are maintaining factors for SAD (McManus et al., 2008; Piccirillo et al., 2016). Accordingly, combining behavior exposure with skills training has proved to be beneficial when treating children and adolescents presenting with SAD, despite being a long process (Beidel et al., 2007; Scaini et al., 2016). The benefits of a brief BT intervention had not been explored before, nor had the benefits of previous actions combining exposure with skills training been explored concerning diverse feared social events, rather than general anxiety, avoidance, and social skills.
Current results show that changes following this brief group behavioral therapy approach to adolescent SAD were limited to how one feels and approaches interaction in new social situations. The current intervention approach focused on training skills pertaining to everyday interactions (as opposed to, for example, interacting specifically with the opposite sex or with figures of authority), following previous similar initiatives (i.e., Beidel et al., 2007; Warner et al., 2007). We may suppose that this practice resulted in experiencing more positive reinforcement and less negative consequences when interacting in new social events thus associating with this circumscribed result. These positive experiences, which may have allowed recalibrating the estimates of the probability of social consequences (Craske et al., 2014), may be explicative of change from pre- to post-program, rather than change in avoidance or the practice of safety behaviors, which did not significantly add to the explanation of the variance of post-intervention anxiety in new social events. Still, as is, current findings indicate that the current intervention approach may be beneficial only with very specific difficulties within social anxiety.
As for social contexts pertaining specifically to formal performance and observation by others (when writing, when riding a bus, or when eating and drinking in public), change in avoidance, but not in the practice of safety behaviors, contributed to explain the variance of post-intervention scores in social anxiety, in addition to pre-intervention social anxiety. Other change mechanisms (e.g., habituation, inhibitory learning; Craske et al., 2014) may have been in place in these situations that were not anticipated via skills training. Alternatively, the fact that change in practice of safety seeking behaviors did not predict post-intervention scores is in line with the previously divulged idea that suppressing all safety behaviors may not be beneficial to cope with social anxiety (Helbig-Lang & Petermann, 2010; Plasencia et al., 2011). It is also in keeping with previous works that did not find evidence of different effects of exposure with and without suppression of safety-seeking behaviors (Meulders et al., 2016).
Current findings point to the relevance of changing avoidance - but not safety behaviors - when intervening in adolescent SAD, as only changing avoidance significantly accounted for the variance of post-intervention social anxiety. Avoidance is proposed to be kept in a self-reinforcing cycle (McManus et al., 2008) that prohibits all forms of positive consequences from being obtained from social events (McNeil et al., 2010). Thus, breaking that cycle and helping adolescents obtain positive social outcomes may have had a substantial impact on our participants’ anxiety. That, in addition to more specific social skills training, should be considered in future works as a way of generalizing change outcomes obtained with behavioral approaches to SAD.
Current findings must be interpreted within some limitations. One of them is that we relied on a small non-treatment seeking sample constituted primarily of 10th graders, which warrants caution in the generalization of the findings. Still, it was a rigorously selected clinical sample, and its size is comparable to that previously used to explore therapeutic change following new intervention approaches (e.g., Masia et al., 2001). Our sample size also implies that only large effect sizes would be found; so, less obvious changes, which might be useful in interpreting change outcomes, may have gone unnoticed. Though only a minority of our sample had previously received psychological support, this might have impacted change outcomes, but our sample size prevented us from assessing that. As for the intervention, we conducted a very brief one, shorter even than the usual practice when exposure alone is implemented (i.e., 8 sessions; Anderson et al., 2017), which tailored skills training to participants’ reported fear hierarchies and so focused on interactive social skills. Adding sessions might be essential to achieve more evident and generalized gains. Likewise, considering non-interacting skills training (e.g., public speaking) might help to generalize the tentative gains that were currently achieved to other social contexts (e.g., assertive interactions or performance in formal social events). Also, comparing the current group intervention with an individual format as proposed by Beidel et al. (2007) may provide evidence on the relevance of peers to behavioral exposure and social feedback. Finally, no follow-up and only self-report data was obtained. Follow-up analyses would be important to ascertain if these actions are relevant in changing the chronic natural course of social anxiety (Keller, 2006). Furthermore, it is important to understand if change following the intervention would contrast with the poorer social skills that others perceive socially anxious adolescents have (Inderbitzen-Nolan et al., 2007).
Behavior therapy has recently been neglected as a way to change adolescent SAD, despite it having provided significant results in the past for children and adolescents (Beidel et al., 2007; Olivares et al., 2002). The current exploratory work ascertained that a brief form of it may be important to adolescents specifically presenting core fears relating to interaction. Even if addressing specific core fears (i.e., interaction, observation, or performance) to better tailor intervention regarding adolescent social anxiety, is a reasonable endeavor (Kodal et al., 2017), it should be noted that other implications of the current intervention may have gone unnoticed given our sample size. Current findings, moreover, stress the importance of engaging with social events (i.e., not avoiding them), mirroring contemporary therapeutic approaches that stress valued action practiced in an attitude of ,acceptance of negative internal experiences, as a path toward well-being (i.e., Acceptance and Commitment Therapy), also in adolescents (Halliburton & Cooper, 2015). Current results, though modest, may stimulate scientific curiosity about future investigations into contextual and behavioral interventions, using larger samples and a more robust methodology, namely addressing the therapeutic effect and cost-effectiveness of behavioral approaches to SAD in adolescence.
CRediT authorship contribution statement
Mariluz Barata: Data curation; Methodology; Resources; Validation; Visualization; Writing - Original draft; Ana Ferreira: Data curation; Methodology; Resources; Validation; Visualization; Writing - Original draft; Paula Vagos: Conceptualization; Formal analysis; Funding acquisition; Methodology; Project administration; Writing - Original Draft; Writing - Review & Editing