Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Motricidade
Print version ISSN 1646-107X
Motri. vol.15 no.2-3 Ribeira de Pena Sept. 2019
https://doi.org/10.6063/motricidade.17662
ORIGINAL ARTICLE
Pain perception and thermographic analysis in patients with chronic lower back pain submitted to osteopathic treatment
Silvânia O Leal1, Eduardo B Neves2,3*, Danielli B Mello1,4, Marcelo Q Filgueiras5,6, Estélio M Dantas1,7
1 Nursing and Biosciences Program (PpgEnfBio), Federal University of Rio de Janeiro State (UNIRIO), Rio de Janeiro, Brazil
2 Brazilian Army Research Institute of Physical Fitness (IPCFEx), Rio de Janeiro, RJ, Brazil
3 Biomedical Engineering Program, Federal Technological University of Paraná (UTFPR), Curitiba, Paraná, Brazil
4 Physical Education College of the Brazilian Army (EsEFEx), Rio de Janeiro, Brazil
5 the Interdisciplinary Center of Laboratory Animal Studies (NIDEAL) of the Federal University of Juiz de Fora, Brazil
6 Rehabilitation Center of João Penido Regional Hospital (FHEMIG)
7 Health and the Environment Program (PSA) of Tiradentes University (UNIT) Aracaju, Sergipe state, Brazil
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Lower back pain (LBP), one of the main causes of pain, employee absenteeism and disabilities, exhibits a multifactorial and degenerative etiology, with different characteristics. Objective: a) analyze the acute effect of osteopathic treatment on the temperature of three dermatomes of patients with chronic lumbago; and b) assess the subjective pain perception of patients before and after an osteopathic session. Materials and methods: Quasi-experimental cross-sectional study of 14 individuals treated at a physical therapy clinic in Brasilia, Brazil. Data collection included physical therapy, pain scale (VAS), thermographic, and anthropometric assessment. Treatment consisted of a single osteopathic session. Results and conclusions: leg and foot temperature declined (∆% = 2.91 and 4.76%, respectively, p = 0005) in the innervations of 2 regions of interest (ROIs) of the L4 lower limb dermatome and pain levels decreased (∆% = 65.98 and 59.92%, p = 0.005) in the men and women, respectively. In addition, a strong correlation was observed between the maximum (r=0.742 and p-value = 0.002) and mean temperature variations of the lumbar region (r=0.733 and p-value = 0.003), according to the VAS. It was concluded that acute osteopathic treatment was efficient in varying the temperature at reference points of the dermatome analyzed and lowering pain perception, suggesting the effectiveness of the proposed treatment.
Keywords: lower back pain, osteopathy, manual therapy, infrared imaging, thermography.
Introduction
Lower back pain (LBP) is one of the primary sources of pain, discomfort, and disability. LBP has repercussions, with localized or general, referred or local, acute or chronic characteristics (Dibai-Filho & de Jesus Guirro, 2015), and is among the problems that most affect the economically active population, in addition to being a major cause of temporary employee absenteeism in Brazil (Jeremias, 2013).
Exhibiting a multifactorial etiology, LBP may occur due to the natural degenerative (aging) process(Rios, Leite, Pereira, Sousa, & Safons, 2015), or be of congenital, inflammatory, infectious, tumoral, mechanical (due to intense physical, trauma or work-related activity) or postural origin (Lizier;, Peres;, & Sakata, 2012; Sedrez & Candotti, 2013). It can also be associated with visceral disorders that may cause viscerosomatic reflexes, in which the viscera lose the ability to slide, changing their functioning and affecting the physical structure. The opposite can also occur, that is, restricted movement of the physical structure can compromise visceral functioning(Degenhardt, Johnson, Brooks, & Norman, 2018; Jerome, 2017).
Osteopathic treatments are one of the therapeutic resources available to treat LBP and trigger numerous corrective and modulating events that encompass not only bone, muscle, and nerve, but primarily the visceral and fascial structures, which contributes to biochemical, sensitive, neurological and motor responses that favor body balance and rebalance(Degenhardt et al., 2018).
With a view to helping diagnose patients complaining of chronic referred pain in neuromusculoskeletal activities, infrared (IR) imaging became an important non-invasive instrument, providing data on skin temperature and the influence of microcirculatory heat conduction from the deepest to the surface tissues, changes that are controlled by the neurovegetative system (Lima, Brioschi, Teixeira, & Neves, 2015; Neves, Vilaça-Alves, Nogueira, & Reis, 2015).
It is known that temperature variations correspond to changes in dermal layer circulation, which is controlled by the sympathetic neurovegetative system. It is also known that somato-somatic and visceral-cutaneous reflexes are triggered by pain due to myofascial dysfunction or visceral inflammation (Lasanen et al., 2018).
Thus, the aim of the present study was twofold: a) analyze the acute effect of osteopathic treatment on the temperature of three dermatomes in patients with chronic lumbago; and b) assess the patients` subjective perception before and after the osteopathic session.
Method
This was a quasi-experimental cross-sectional study.
Participants
The sample was selected according to the following inclusion criteria: individuals of both sexes, aged between 21 and 50 years, diagnosed with chronic lumbago at least six months before, who had not undergone any physical therapy, exhibited no malignant tumor, infectious or rheumatic disease (rheumatoid arthritis or ankylosing spondylitis), had submitted to magnetic resonance imaging (MRI) in the ten days before treatment, and had not undergone spinal surgery.
Exclusion criteria: individuals who regularly used pain medication or refused to give their informed consent.
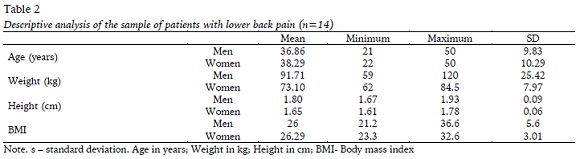
The sample consisted of 14 individuals treated at a physical therapy clinic in Brasilia: seven men (aged 36.86±9.83 years) and seven women (38.29±10.29 years) with 10±3.4 months and 11±67 months of chronic lower back pain, respectively.
All the participants were advised of the study aims and gave their informed consent, and the research complied with the human being guidelines of Resolution 466/12 of the National Health Council (CNS). The study was approved by the Research Ethics Committee of the Federal University of Rio de Janeiro state (UNIRIO), under protocol number CAAE: 93050218.0.0000.5285
Measures
At the first meeting, any doubts expressed by the subjects were clarified, as well as inclusion criteria, assessment instruments, and the care required for thermographic assessment, in addition to the time needed for the first session (assessment and treatment).
The individuals were assessed for three weeks. Each participant was submitted to a single 120-minute physical therapy session, where they underwent a series of assessments (medical history, VAS, and thermography) and the osteopathic treatment protocol.
Procedures
The First, clinical-functional assessment (anthropometric data, medical history, and physical examination consisting of inspection, palpation, muscle conditions, and mobility), evaluation of complementary examinations, VAS, and thermographic assessment were carried out.
Diagnostic assessment (medical history) included identification (name, age, sex, ethnicity, marital status, birthplace, nationality, address, profession, and occupation); primary complaint (PC); current disease history (CDH); progressive pathology history (PPH); patient`s medical history; family history (FH); personal history (physiological); social history and the visual analog scale (VAS).
A Filizola® weight balance (Brazil) (150kg and 100g resolution) and a Sanny® stadiometer (Brazil) were used for anthropometric assessments. The International Society for the Advancement of Kinanthropometry (Marfell-Jones, Olds, Stewart, & Carter, 2006) protocols were applied.
Lower back pain was quantified using the VAS, where participants were shown a ruler numbered 1 to 10 with faces demonstrating three pain intensities: a) Mild (0 to 2) b) Moderate (3 to 5 less intense and 5 to 7 more intense) and c) Intense (8 to 10). Subjects were asked to bend their torso and rate their pain intensity. This assessment was carried out by the same evaluator, before and after the treatment protocol. According to Brito et al. (2015), a decline of two points is considered a good improvement.
Palpation was conducted with patients standing and lying down, investigating the type of pain and symptoms correlated with the medical history and physical assessment (articular, ligament, myofascial, neural, vascular, and local).
A radiologist assessed the MRIs in order to supplement and confirm the information collected at the initial anamnesis and palpation.
Infrared (IR) imaging was analyzed to identify the differences in temperature in the skin tissue to correlate this information with the pain sites reported and dermatomes in the lumbar region, on the day of the first intervention.
For IR imaging, the individuals were previously instructed not to engage in physical exercise, consume hot or cold beverages, expose themselves to the sun for three days, shave on the examination day, or use make-up, sunscreen or moisturizing cream (Salamunes, Stadnik, & Neves, 2017).
Infrared imaging was performed in a dimly-lit air-conditioned room, 15 minutes before and after the treatment protocol (single session). Subjects were acclimated for 15 minutes, at a temperature of 23ºC, standing (Mendes et al., 2015; E B Neves et al., 2015). Immediately afterward, thermographic analysis of the L4 lumbar spine and L4 dermatome region (hallux and medial part of the knee) was carried out; subjects were then submitted to an osteopathic session, as previously described, followed once again by acclimatization (15 minutes), further thermographic analyses and VAS.
For thermographic recordings, the camera was placed on a tripod 1.20 m between the patient and evaluator, with the camera in the horizontal position to capture images in the lumbar and knee regions, while for the hallux, the distance was 0.70 cm and the camera was angled at 45º. The camera was regulated at the height of the lumbar region and knees of the patients, who were in the orthostatic position. The men and women were instructed to wear swimming trunks and a bikini, respectively, in order to expose the region under analysis (Neves, Salamunes, de Oliveira, & Stadnik, 2017).
The images were recorded on a 320 X 240-pixel Fluke T1 32 thermographic camera, programmed with an emissivity of 0.98 and an ultra-contrast palette. All thermal images were analyzed using Smartview 3.1.4 software (Fluke®).
Osteopathic treatment protocol
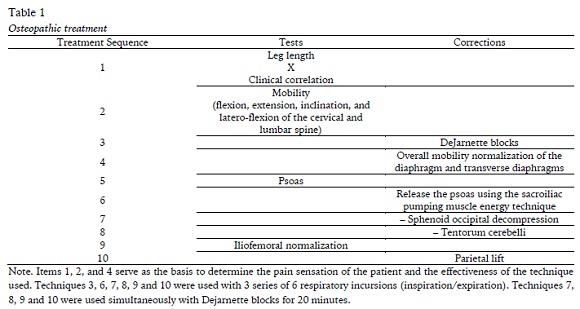
The patients were submitted to the osteopathic techniques presented in Table 1, assessed before and after a 60-minute session.
Statistical analysis
The statistical procedures consisted of descriptive analysis using means of central tendency (mean and median), and dispersion (standard deviation - s, standard error of the mean - e). Sample normality was tested by applying the Shapiro-Wilk test, and since several variables exhibited Gaussian distribution, a nonparametric approach was selected for data analysis (Wilcoxon signed-rank test).
Results
Table 2 shows the descriptive analysis of the sample. The age of the sample is compatible with the economically active population. Both groups were considered overweight, according to the body mass index classification of the WHO.
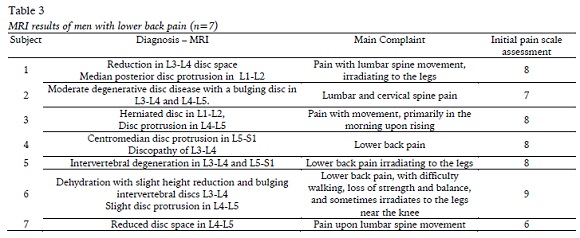
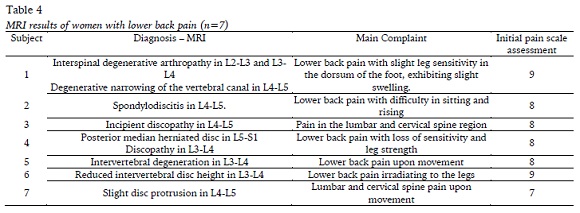
The magnetic resonance imaging (MRI) examinations of the subjects analyzed obtained the following results (Tables 3 and 4).
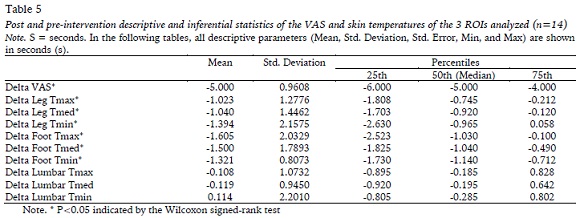
Table 5 shows VAS data, and skin temperatures of the 3 ROIs analyzed. The sample exhibited a significant drop in temperature after intervention in 2 ROIs of the dermatomes analyzed (leg and foot) and pain perception according to the VAS. No decrease in temperature was found in the lumbar region.
There was a strong correlation between the maximum (r=0.742 and p-value = 0.002) and mean temperature variation in the lumbar region (r=0.733 and p-value = 0.003) with the VAS.
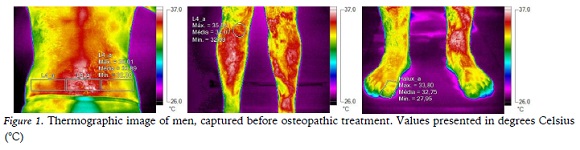
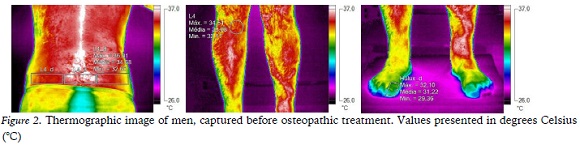
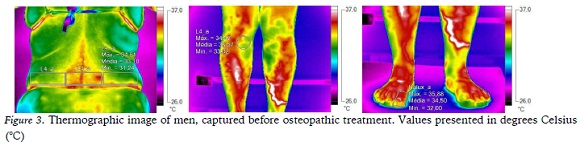
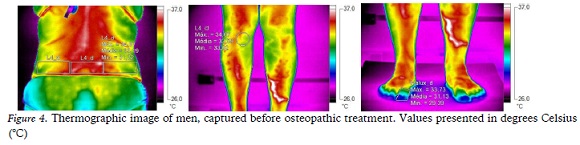
Figures 1 and 2 present the thermographic images in relation to the three ROIs used to assess innervation in the dermatome of L4 in the lumbar region, anterior medial border of the knee, and hallux. The pre and post-test measures were conducted on the right side. Figures 3 and 4 show thermographic images of women in relation to the three ROIs in the pre and post-test after the intervention.
Discussion
The study subjects were middle-class university graduates (90%), worked for 6 to 8 hours a day in middle to high-complexity jobs, and classified as overweight. This corroborates the findings of epidemiological studies by (Ponce Martínez, Villarreal-Ríos, Vargas-Daza, Martínez-González, & Galicia-Rodríguez, 2013), who found that LBP was one of the main reasons for employee absenteeism, causing a significant impact on the health system, public coffers, and society in general.
Several studies (de Moraes Vieira, Garcia, da Silva, Araújo, & Jansen, 2012; Depintor, Bracher, Cabral, & Eluf-Neto, 2016) reveal that the prevalence of chronic lower back pain may be associated with the musculoskeletal system (Saçala, Luvizotto, Oselame, & Neves, 2018), articular and neurological disorders, exhibiting distinct pain patterns and lesion severity. This can be observed in the present study, where 71% of the women analyzed reported lower back pain and surgical scars (cesareans), with facial restrictions in the abdominal region, in addition to inadequate posture at work.
The remaining 29% of women exhibited different pain intensities, but with characteristics like those of 65% of the men analyzed here, all displaying a mechanical or postural pain pattern. These findings corroborate studies (Barbosa, Vieira, & Garcia, 2018) and (Depintor et al., 2016) reporting that overweight individuals whose work involves long hours sitting down, little physical activity, and poor posture, exhibit a higher number of mechanical alterations.
The MRIs of the subjects analyzed here demonstrate mechanical changes in most of them, since 70% exhibited invertebral disc degeneration in L4-L5, with small to moderate foraminal disc protrusion; 20% interspinal degenerative arthropathy in L2-L3 and L3-L4 and degenerative narrowing of the vertebral canal in L4-L5; and 10% incipient discopathy in L1-L2 and L4-L5. Separately, these changes may not represent a painful condition, but this rarely occurs in the presence of other physical, environmental, work, or psychological factors.
As such, it was essential in the present study to cross-reference the information obtained in the different assessments, in order to understand the complexity of treating patients with chronic lower back pain, in addition to correlating these data with thermographic evaluation and not restricted solely to the subject’s main complaint, but with a total body assessment (Lima et al., 2015), mainly of the dermatome corresponding to the pain complaint.
Some studies demonstrated that temperatures 0.5°C above the reference standard indicate dysfunction and a direct correlation between pain intensity and asymmetry (Hamaguchi & Masui, 2014; Lima et al., 2015). In the present study, the mean pain perception of the assessed subjects was 8 points, classified as intense by the VAS, and the difference in temperature of the segments analyzed showed values of more than 0.5º C above the standard.
Correlation between the thermographic examination and the VAS revealed a significant variation (p=0.001) after osteopathic treatment in the dermatomes of the L4 nerve root. According to (M.L., Abramavicus, & Corrêa, 2005; Roy, Boucher, & Comtois, 2013), patients experiencing pain exhibited abnormal IR images associated with vasomotor alterations.
Nerve root dysfunctions are accompanied by changes in ipsilateral IR radiation in the corresponding dermatome, as observed by (Gemelli, de Macedo, Neves, & Ulbricht, 2012), suggesting that positive effects occurred after manipulation of sympathetic vasomotor centers, with temperature differences observed after dorsal manipulation of the center of the palms of the hand. This information supports the findings of the present study, in terms of the data obtained for the dermatomes corresponding to the L4 roots in the legs and feet.
Among the symptoms associated with chronic lower back pain are intestinal alterations (20%), sleep disorders (40%) and the presence of pain throughout the day (45%) in the subjects analyzed. According to (Padovan & Dean Azevedo, 2011), the decline in serotonin production (95% in the intestine) may be compromised by the restricted visceral mobility and motility, which could raise the levels of stress, constipation, depression and pain, and is directly associated with symptoms of lumbago.
A total of 70% of participants self-medicated with pain killers, anti-inflammatories or muscle relaxants during the most intense episodes of pain, reporting that they knew how to treat themselves since they had experienced pain for months or years. Around 60% had undergone other physical therapy treatments, such as overall postural programming, conventional hydrotherapy and physical therapy (tens and ultrasound) A total of 60 % were successful for some time and 40% abandoned treatment because no improvement was perceived. This information was reported in other studies that investigated chronic lower back pain, due to the difficult diagnosis, owing to multifactorial causes and determining the best (de Moraes Vieira et al., 2012; Depintor et al., 2016; Malta et al., 2017; Meucci, Fassa, Faria, & Fiori, 2015).
Table 5 shows no significant temperature difference in the lumbar region, as reported in the studies by (Brito et al., 2015; Roy et al., 2013), although a difference in temperature sometimes occurred, even after the acclimation period. This may be related to the distribution of skin temperature in hot or cold environments, whereby the central temperature (torso) tends to be higher (Salamunes et al., 2017). However, after intervention and acclimation and analysis of the ROIs related to the dermatomes of the L4 lumbar region, greater homogeneity was expected between the right and left sides and a decline in body temperature ipsilateral to the dermatome in question, according to the analysis (Table 2). These data show the same trend as those found by (Feng, Zhao, & Liang, 1998; Ping & You, 1993; Roy et al., 2013).
LBP is a multifactorial etiology, following earlier studies (Degenhardt et al., 2018; Dibai-Filho & de Jesus Guirro, 2015; Jerome, 2017). In the present investigation, the heterogeneity of the complaints and the different sites affected on the spine, as well as the small sample size, were limitations.
Conclusion
Infrared imaging assessment (thermography) shows the effect of acute osteopathic treatment on temperature variations at the reference points of the dermatome analyzed. Moreover, pain perception is subjective, demonstrating a difference in temperature after osteopathic treatment, suggesting the efficacy of the proposed treatment. As such, a careful assessment and systematized treatment aimed at the real needs and dysfunctions of the patient, with the help of thermography, may exhibit effective responses.
Other analyses are recommended for future studies, such as bilateral assessment of the limbs, increasing the number of osteopathic sessions, and determining the difference in temperature between sessions and changes in quality of life after a few weeks and months of treatment.
REFERENCES
Barbosa, F. M., Vieira, É. B. d. M., & Garcia, J. B. S. (2018). Beliefs and attitudes in patients with chronic low back pain. BrJP, 1(2), 116-121. DOI: 10.5935/2595-0118.20180023. [ Links ]
Brito, J. D., Schmit, E. F. D., Nóbrega, S. R., Neto, S. A., de Almeida Ferreira, J. J., de Andrade, P. R., & dos Santos, H. H. (2015). Alterações termográficas na lombalgia crônica sob tratamento fisioterapêutico: ensaio clínico controlado e randomizado. ConScientiae Saúde, 14(1), 89-98. DOI: 10.2285/ConsSaude.v14n1.5279. [ Links ]
de Moraes Vieira, É. B., Garcia, J. B. S., da Silva, A. A. M., Araújo, R. L. T. M., & Jansen, R. C. S. (2012). Prevalence, characteristics, and factors associated with chronic pain with and without neuropathic characteristics in São Luís, Brazil. Journal of Pain and Symptom Management, 44(2), 239-251. DOI: 10.1016/j.jpainsymman.2011.08.014. [ Links ]
Degenhardt, B. F., Johnson, J. C., Brooks, W. J., & Norman, L. (2018). Characterizing adverse events reported immediately after osteopathic manipulative treatment. J Am Osteopath Assoc, 118(3), 141-149. [ Links ]
Depintor, J. D. P., Bracher, E. S. B., Cabral, D. M. C., & Eluf-Neto, J. (2016). Prevalence of chronic spinal pain and identification of associated factors in a sample of the population of São Paulo, Brazil: cross-sectional study. Sao Paulo Medical Journal, 134(5), 375-384. DOI: 10.1590/1516-3180.2016.0091310516. [ Links ]
Dibai-Filho, A. V., & de Jesus Guirro, R. R. (2015). Evaluation of myofascial trigger points using infrared thermography: a critical review of the literature. Journal of manipulative and physiological therapeutics, 38(1), 86-92. DOI: 10.1016/j.jmpt.2014.10.010. [ Links ]
Feng, T., Zhao, P., & Liang, G. (1998). Diagnostic significance of topical image of infrared thermograph on the patient with lumbar intervertebral disc herniation-a comparative study on 45 patients and 65 normal control. Zhongguo Zhong xi yi jie he za zhi Zhongguo Zhongxiyi jiehe zazhi= Chinese journal of integrated traditional and Western medicine, 18(9), 527-530. [ Links ]
Gemelli, M., de Macedo, R., Neves, E., & Ulbricht, L. (2012). Effect of osteopathic maneuvers on movement of the upper limbs: a case study. Paper presented at the XXIII Congresso Brasileiro em Engenharia Biomédica, [ Links ] Porto de Galinhas-BA.
Hamaguchi, S., & Masui, J. (2014). The instrument for thermography. The Japanese journal of Anesthesiology, 63(7), 728-736. [ Links ]
Jeremias, A. T. (2013). Dor crónica lombar: modelo preditivo dos resultados da fisioterapia. (Mestrado), Instituto Politécnico de Setúbal. [ Links ] Escola Superior de Saúde.
Jerome, J. A. (2017). An osteopathic approach to chronic pain management. J Am Osteopath Assoc, 117(5), 306-314. DOI: 10.7556/jaoa.2017.056. [ Links ]
Lasanen, R., Malo, M. K., Airaksinen, O., Karhu, J., Töyräs, J., & Julkunen, P. (2018). Infrared thermography reveals effect of working posture on skin temperature in office workers. International Journal of Occupational Safety and Ergonomics, 24(3), 457-463. DOI: 10.1080/10803548.2017.1336299. [ Links ]
Lima, R. P. S., Brioschi, M. L., Teixeira, M. J., & Neves, E. B. (2015). Análise Termográfica de Corpo Inteiro: indicações para investigação de dores crônicas e diagnóstico complementar de disfunções secundárias. Pan American Journal of Medical Thermology, 2(2), 70-77. DOI: 10.18073/2358-4696/pajmt.v2n2p70-77. [ Links ]
Lizier;, D. T., Peres;, M. V., & Sakata, R. K. (2012). Exercícios para Tratamento de Lombalgia Inespecífica. Revista Brasileira Anestesiologia, 62(6), 838-847. [ Links ]
M.L., B., Abramavicus, S., & Corrêa, C. F. (2005). Valor da imagem infravermelha a avaliação da dor. Revista Dor, 6(1), 514-524.
Malta, D. C., Oliveira, M. M. d., Andrade, S. S. C. d. A., Caiaffa, W. T., Souza, M. d. F. M. d., & Bernal, R. T. I. (2017). Factors associated with chronic back pain in adults in Brazil. Revista de saude publica, 51, 9s. DOI: 10.1590/S1518-8787.2017051000052. [ Links ]
Marfell-Jones, M., Olds, T., Stewart, A., & Carter, L. (2006). International standards for anthropometric assessment Potchefstroom. South África. [ Links ]
Mendes, R., Sousa, N., Almeida, A., Vilaça-Alves, J., Reis, V. M., & Neves, E. B. (2015). Thermography: a technique for assessing the risk of developing diabetic foot disorders. Postgraduate medical journal, 91(1079), 538-538. DOI: 10.1136/postgradmedj-2015-133441. [ Links ]
Meucci, R. D., Fassa, A. G., Faria, N. M., & Fiori, N. S. (2015). Chronic low back pain among tobacco farmers in southern Brazil. International journal of occupational and environmental health, 21(1), 66-73. DOI: 10.1179/2049396714Y.0000000094. [ Links ]
Neves, E. B., Moreira, T. R., Lemos, R., Vilaça-Alves, J., Rosa, C., & Reis, V. M. (2015). Using skin temperature and muscle thickness to assess muscle response to strength training. Revista Brasileira de Medicina do Esporte, 21(5), 350-354. DOI: 10.1590/1517-869220152105151293. [ Links ]
Neves, E. B., Salamunes, A. C. C., de Oliveira, R. M., & Stadnik, A. M. W. (2017). Effect of body fat and gender on body temperature distribution. Journal of thermal biology, 70, 1-8. DOI: 10.1016/j.jtherbio.2017.10.017. [ Links ]
Neves, E. B., Vilaça-Alves, J., Nogueira, I. R. A., & Reis, V. M. (2015). Influence of subcutaneous fat layer in skin temperature. Motricidade, 11(4), 120-126. DOI: 10.6063/motricidade.5999. [ Links ]
Padovan, R. B., & Dean Azevedo, R. O. (2011). Tratamento osteopático visceral: repercussões do sistema fascial no funcionamento e na postura humana. Revista Brasileira de Osteopatia e Terapia Manual, 2(1), 18-22. [ Links ]
Ping, Z., & You, F. (1993). Correlation study on infrared thermography and nerve root signs in lumbar intervertebral disk herniation patient: a short report. Journal of manipulative and physiological therapeutics, 16(3), 150-154. [ Links ]
Ponce Martínez, M. D. C., Villarreal-Ríos, E., Vargas-Daza, E. R., Martínez-González, L., & Galicia-Rodríguez, L. (2013). Costo institucional del paciente con incapacidad temporal para el trabajo por lumbalgia mecánica. Revista de la Asociación Argentina de Ortopedia y Traumatología, 78(3), 113-119. [ Links ]
Rios, J. C. S., Leite, T. K. M., Pereira, M. d. M., Sousa, F. C., & Safons, M. P. (2015). Efeitos de um programa educacional de autocuidado de coluna em idosos com dor lombar crônica: um estudo quasi-experimental. Motricidade, 11(1), 53-63. DOI: 10.6063/motricidade.3143. [ Links ]
Roy, R. A., Boucher, J. P., & Comtois, A. S. (2013). Comparison of paraspinal cutaneous temperature measurements between subjects with and without chronic low back pain. Journal of manipulative and physiological therapeutics, 36(1), 44-50. DOI: 10.1016/j.jmpt.2012.12.002. [ Links ]
Saçala, R., Luvizotto, J. d. R., Oselame, G. B., & Neves, E. B. (2018). Disturbios Osteomusculares relacionados ao processo de trabalho no atendimento pré-hospitalar. Revista da Universidade Vale do Rio Verde, 15(2), 751-758. DOI: 10.5892/ruvrd.v15i2.3085. [ Links ]
Salamunes, A. C. C., Stadnik, A. M. W., & Neves, E. B. (2017). The effect of body fat percentage and body fat distribution on skin surface temperature with infrared thermography. Journal of thermal biology, 66, 1-9. DOI: 10.1016/j.jtherbio.2017.03.006. [ Links ]
Sedrez, J. A., & Candotti, C. T. (2013). Métodos não invasivos de avaliação postural da escoliose: Uma revisão sistemática. Motricidade, 9(4), 100-111. DOI: 10.6063/motricidade.9(4).949. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
* Av. João Luiz Alves - Urca, Rio de Janeiro - RJ, 22291-060, Brasil. Email: neveseb@gmail.com
Acknowledgments:
Eduardo B. Neves acknowledge the financial support of CNPq (Brazilian Ministry of Science and Technology) from the process number 303678/2018-6
Conflict of interests:
Nothing to declare.
Funding:
Nothing to declare.
Manuscript received at December 3th 2018; Accepted at March 30th 2019