A large percentage of individuals seeking a combined orthodontic/orthognathic surgery intervention have skeletal Class III malocclusions.1 This sagittal discrepancy is characterized by maxillary deficiency, mandibular excess or a combination of both.1,2 Changes in vertical facial growth can further contribute to the complexity of these cases.3,4,5,6,7
There are several treatment options for Class III malocclusions.
Dentofacial orthopedic appliances8,9,10and devices for protraction with bone anchorage11,12can improve the growth pattern in children with a genetic predisposition for this problem.
Purely orthodontic dentoalveolar compensation can be attempted to camouflage the skeletal discrepancy in adults when an aesthetically acceptable profile accompanies a mild-to-moderate skeletal Class III malocclusion.13-16
Excessive retroclination of the lower incisors during camouflage treatments can lead to an exaggerated buccal prominence of their roots and gingival recession.14 In such cases, a combined surgical orthodontic treatment, rather than camouflage, would be the correct approach.14 Additional guidelines for surgical orthodontic treatment in adult patients are ANB and lower incisor-mandibular plane angles smaller than -4o and 83o, respectively.17 Other important factors that distinguish surgical from non-surgical patients are the ratio between maxillary and mandibular length, the gonial angle, the sella-nasion distance and the Wits appraisal.16,17,18 19
The main objectives of orthognathic surgery are the development of a functional and stable occlusion and an improvement in facial aesthetics.15, 20,21,22,23,24,25In this type of treatment, a pre-surgical orthodontics phase is usually followed by the surgical correction of the skeletal discrepancy. Then, a post-surgical orthodontic period is required to finish and detail the occlusion.26
Dento-alveolar compensations in the form of upper incisor proclination and lower incisor retroclination help to maintain function and camouflage an existing Class III skeletal discrepancy.4,15,27,28In patients with larger anteroposterior discrepancies and increased mandibular posterior rotation, the compensatory lower incisor retroclination is increased.13,28
Additionally, in hyperdivergent patients, the lower incisors erupt in a way that maintains the overbite, and the alveolar bone becomes longer and thinner in the labio-lingual direction.
These features may increase the risk of periodontal problems in the anteroinferior region.27,29,30Pre-surgical orthodontics eliminates these compensations by creating or increasing a reverse overjet, which allows a surgical mandibular setback and/or maxillary advancement. As a result, the direction of the incisor movement is opposite to that required by a non-surgical, compensatory treatment plan. Therefore, comparing to the baseline, the patient’s malocclusion and profile are generally worse immediately before surgery, and this can only be avoided if an early surgical approach is used.15,31,32
Depending on the magnitude of the initial sagittal discrepancy and the degree of incisor compensation observed, an orthodontic treatment plan is established. This treatment may require the extraction of upper first premolars, alone or in combination with the lower second premolars.
The aim of this retrospective cephalometric study was to evaluate the changes produced by pre-surgical orthodontic treatment on dental and skeletal measurements of the lower third of the face, in patients with skeletal Class III malocclusions requiring orthognathic surgery, using different extraction protocols. The null hypothesis tested was that, after the pre-surgical orthodontic phase, no differences would be found in cephalometric measurements between the extractions (for orthodontic and non-orthodontic reasons) and the no-extractions groups.
Material and methods
The sample for this study consisted of adult orthodontic patients with skeletal Class III malocclusions requiring orthognathic surgery. The inclusion criteria were European origin, no previous orthodontic or orthopedic treatments, good quality cephalometric x-rays, and treatment performed by the same specialist in orthodontics. After approval by the Ethics Committee of the School of Dentistry of the University of Lisbon, a sample of 18 males and 22 females was gathered, with
informed consent. Individuals with congenital anomalies and severe facial asymmetries were excluded from the study.
The original sample was divided into three groups: Group N, including no extractions (n =13); Group E, including upper first premolars extracted for orthodontic treatment purposes (n =12); and Group E-NO, including previous extractions for non-orthodontic reasons (n =15).
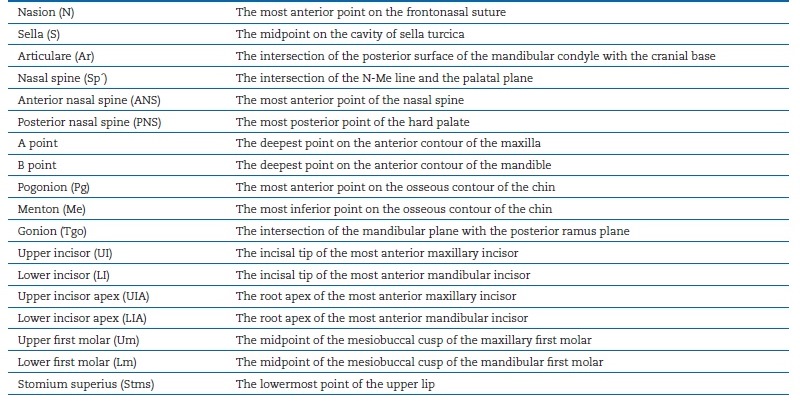
Lateral cephalograms were taken before (T1) and after (T2) the pre-surgical orthodontic treatment phase with the aid of a cephalostat and with the Frankfurt horizontal plane parallel to the floor. The Adobe Photoshop CS5 (Adobe Inc.® San José, California) program was used to superimpose the T2 cephalogra on the T1 one, according to the structural method of Björk. The horizontal reference plane (x) was constructed 7º above the sella-nasion line, with the vertex at nasion.33 A line perpendicular to the horizontal plane at nasion was used as the vertical reference plane (y). All linear cephalometric variables were measured either parallel or perpendicular to the x plane, using the cephalometric program Nemoceph (Nemotec ®, Madrid, Spain). The cephalometric landmarks used are described in Table 1. The palatal plane (ANS-PNS), the mandibular plane (Tgo-Me), the long axis of the upper incisor UI1 (UIUIA) and the long axis of the lower incisor LI1 (LI-LIA) were also traced in the analysis.
Cephalometric measurements were chosen to represent skeletal and dental variables, which could be changed by the pre-surgical orthodontic treatment. For skeletal changes, the SNA angle, total facial height (TFH, N-Me distance), inferior facial height (IFH, Sp´-Me distance), maxillary prominence (point A to y distance), mandibular prominence (point B to y distance), chin prominence (Pg to y plane) and the MP-x angle (Tgo-Me to x plane) were calculated. For dental changes, the
following measurements were evaluated: upper incisor exposure (UI-Stms distance), overjet, overbite, UI-y distance, LI-y distance, UI-PP distance, LI-MP distance, UI1-x angle, LI1-x angle, UI1-PP angle, LI1-MP angle, Um-y distance, Lm-y distance, Um-PP distance, and Lm-MP distance.
One researcher traced all the radiographs and was blinded for patients’ identity, to avoid bias. Ten randomly chosen cases were re-traced within a month interval, by the same investigator.
Method error was evaluated with paired t-tests and the Dahlberg’s equation: √Σd2/2n, where d is the difference between the calculated values between the first and the second tracings.34
Statistical analysis was done with SPSS® version 20.0 for Macintosh (IBM Company, Armonk, NY, USA). Descriptive statistics (mean and standard deviation) were calculated at T1 and T2 for each cephalometric variable. The Shapiro-Wilk test was performed to evaluate normality in the sample distribution.
A t-test for independent samples was used to determine the influence of the orthodontic treatment on the cephalometric variables within each group. Differences between the groups before treatment and differences in the changes produced by the orthodontic treatment in the three groups were evaluated using an ANOVA analysis. Post-hoc testing was done with the Bonferroni method. The level of statistical significance was fixed at 5%.
For the method error, the paired t-test revealed no significant differences between the first and the second measurements (p>0.05). No systematic deviations were found, and the values obtained from the Dahlberg equation were generally small (<1°/1mm). Therefore, there were no significant random errors.
Results
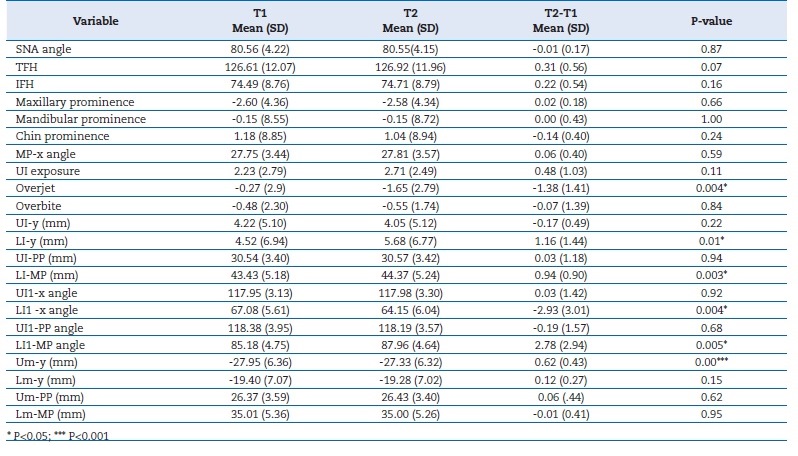
According to the results of the Shapiro-Wilk test, all variables in the study showed normal distribution. The descriptive statistics (mean and standard deviation) before the orthodontic treatment (T1) are presented in Table 2.
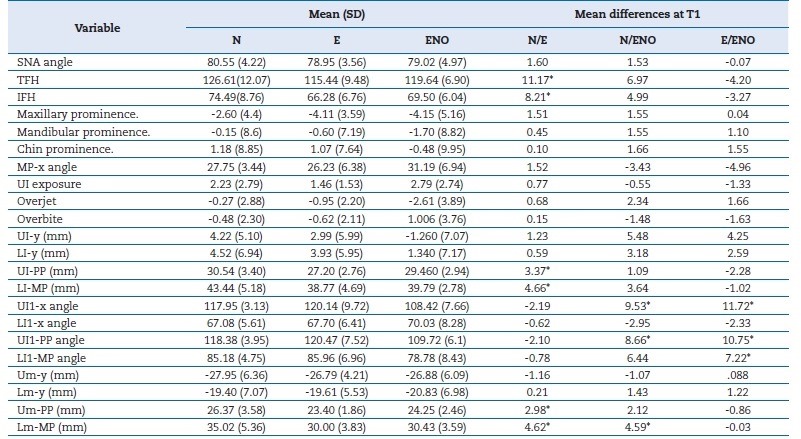
Table 2 Descriptive statistics (mean and standard deviation) and mean differences between groups in T1, for all the variables
*P<0.05
The differences between Groups N, E and E-NO before the pre-surgical orthodontic treatment (T1) are exposed in Table 2. In comparison with Group N, Group E was characterized by a decrease in TFH and IFH. The distances UI-PP, Um-PP, LI-MP and Lm-MP were also reduced. The distance Lm-MP was smaller in Group E-NO than in Group N. Upper incisor inclination in relation to both the palatal plane and the horizontal plane was reduced in Group E-NO in comparison with the other two
groups. The lower incisor retroclination was significantly (p<0.05) greater in Group E-NO than in Group E.
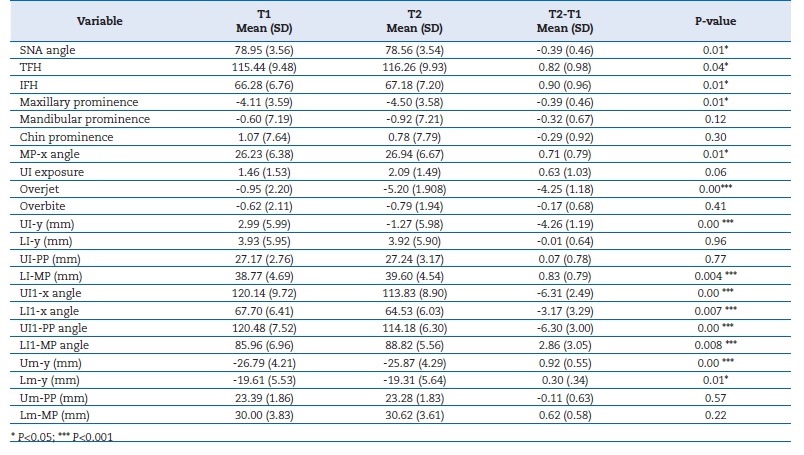
Changes produced by the orthodontic treatment are presented in Table 3 for Group N, Table IV for Group E and Table V for Group E-NO. In Group N, the overjet became more negative due to lower incisor proclination and protraction, and the distance between this incisor and the mandibular plane increased. The upper molars moved forward in Group N.
In Group E, the SNA angle decreased, and point A retraction was observed. Posterior mandibular rotation caused an increase in TFH and IFH and in the MP-x angle (Table 4). The overjet became more negative due to the elimination of dental compensations: the upper incisors were retracted and retroclined, and the lower incisors were proclined and extruded.
Both upper and lower molars moved forward in Group E. An increase in TFH and IFH and the MP-x angle were observed in Group E-NO (Table 5). The overjet became more negative and the overbite decreased with lower incisors proclination and protraction, and both upper and lower molars mesialized in Group E-NO.
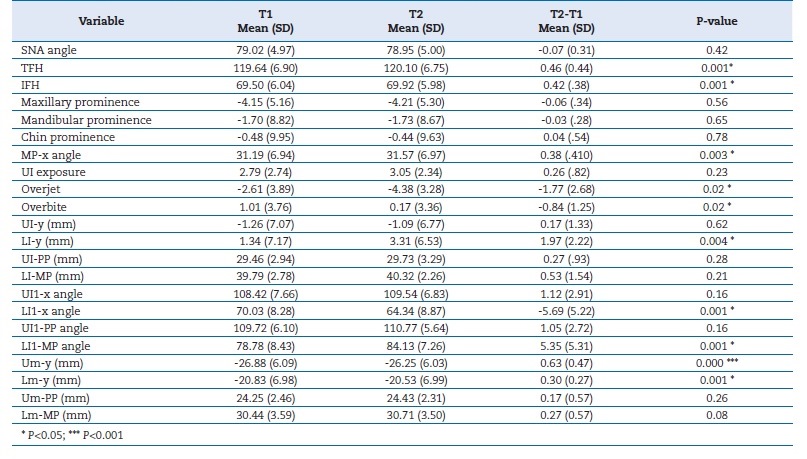
Table 5 Changes in Group E-NO (extractions for non-orthodontic reasons) caused by the pre-surgical orthodontic treatment
The comparisons between groups during the pre-surgical orthodontic treatment are presented in Table 6. There was a larger decrease in the SNA angle and a greater retraction of point A in Group E when compared to Group N. Mandibular posterior rotation was also greater in Group E with a higher increase in the IFH and the MP-x angle. Overjet became more negative in Group E than in Group N, due to a greater retraction and retroclination of the upper incisors.
When comparing Group E to Group E-NO, a significant (p<0.05) decrease in the SNA angle and a larger retraction of point A were observed in the first. Overjet also became more negative, primarily due to a larger retraction and retroclination of the upper incisors. In Group E-NO, greater lower incisor advancement was observed in relation to the vertical plane.
There were no significant (p>0.05) differences in the changes observed between Groups N and E-NO (Table 6).
Discussion
Pre-surgical orthodontic treatment involves leveling and aligning of the dental arches, transverse coordination, closure of extraction spaces, and elimination of dental compensations.26 Although the orthodontic treatment might involve extractions, some Class III surgical patients already have missing teeth for non-orthodontic reasons. Since this could influence the cephalometric variables measured in the present study, the patients were divided into three groups (N, E and E-NO).
Before treatment, the magnitude of the sagittal discrepancy was similar in all groups. The increased upper incisor proclination initially observed in Group E may have contributed to the decision to extract teeth in these cases. In Group E-NO, the normal upper incisor inclination could be explained by the previous absence of posterior teeth. This arch length collapse could also have been responsible for the greater retroclination observed in the lower incisors of this group. However, some degree of lower incisor retroclination was present in all groups before treatment.
During the pre-surgical orthodontic treatment, all three groups exhibited anchorage loss with mesialization of the upper first molars. In Groups E and E-NO, lower molar advancement also occurred, possibly due to closure of the extraction spaces. Although Group E initially demonstrated greater upper incisor proclination, the treatment caused significant upper incisor retraction and retroclination only in this group, resulting in an overjet more negative than in the other two groups.
Alveolar bone resorption on the labial aspect of the retracted incisors caused a significant point A retraction and a reduction in the SNA angle.
According to other authors, orthodontic treatment planning without extractions in the upper arch may limit upper incisor retraction and may be responsible for the persisting post-treatment incisor proclination.15,35 This situation was verified in Group N in the present study, where the upper incisors remained proclined. In Group E-NO, these teeth maintained a normal inclination even before surgery. Generally, satisfactory results depend on an adequate correction of upper incisor proclination as successful decompensation permits greater surgical movement.35,36
The lower incisors proclined in all groups and advanced in Groups N and E-NO. The success in lower incisor decompensation was verified by other authors.36However, the greater initial lower incisor retroclination in Group E-NO, caused by the absence of several posterior teeth, limited the amount of proclination achieved orthodontically and, thus these teeth were still excessively retroclined post-treatment comparing to the norm.38This association between unsuccessful lower incisor decompensation and extractions in the lower arch has been previously documented.35 Persisting lower incisor retroclination can limit correction and lead to reduced ANB and excessive SNB angles even after treatment.35
Although decompensation has been described to be less successful in hyperdivergent and severe anteroposterior discrepancies,37 the groups were similar initially. Factors that contribute to insufficient lower incisor decompensation include lower arch extractions, severe initial lower incisor retroclination, lack of patient cooperation in the use of Class II elastics, and insufficient alveolar bone thickness to permit incisor advancement.35
One of the limitations of this investigation was the small sample size in each group since the 40 patients were subdivided into three groups. Also, Group E-NO was heterogeneous and included patients that had three or more missing teeth anterior to the upper and lower first molars.
Future studies on the long-term impact of removing dental compensations on surgical cases with and without extractions are needed. Finally, the effects of pre-surgical incisor decompensation on the soft tissues, which, although temporary, can have a strong impact on facial aesthetics, should be investigated.
Conclusions
1) In Group E, there was a decrease in the SNA angle due to retraction of point A.
2) Mandibular clockwise rotation in Groups E and E-NO led to an increase in total and inferior facial heights.
3) Upper incisors were significantly retracted and retroclined only in Group E, where extractions facilitated incisor decompensation.
4) The lower incisor was proclined in all three groups and protracted in Groups N and E-NO. Due to the large degree of initial retroclination, the lower incisors remained retroclined in Group E-NO after treatment.
5) The upper first molar advanced in all the three groups.