Introduction
The simple bone cyst (SBC), also known as traumatic, solitary, overflow, unicameral and hemorrhagic bone cyst or idiopathic bone cavity, was first described by Lucas and Blum in 1929.1-4
The World Health Organization (WHO) classifies it as part of a group of giant cell lesions and bone cysts, which also include central and peripheral giant cell granuloma, cherubism, and aneurysmatic bone cyst.5,6 It is an atypical intraosseous lesion that has no epithelial lining. Therefore, it is considered a pseudocyst.1,4,7-9 It is usually an empty cavity, although sometimes it can be filled by blood, serum, or both.1,7,8,10
The exact etiopathogenesis of SBC remains uncertain, although trauma is frequently an associated factor.8,11 The most accepted theory is that an intraosseous clot, produced by trauma, decomposes and liquefies leaving an empty cavity.1-3,7,12 However, this theory has been questioned, since most cases describe no history of trauma.3 SBC usually occurs in young patients, in the first two decades of life, with no sex preference.1,2,7 It is often found in the humerus, femur, and other long bones9 but in 1% of cases, it affects the mandible.2-4,7,10 Most cases of SBC are asymptomatic and do not cause cortical expansion. They are usually found in routine radiographies.2,3,8,9 The teeth associated with the lesion are vital and generally do not present root resorption nor displacement.2,3,8,13 It is observed as a radiolucent image, uni or multilocular, with irregular margins or well-defined cutouts.2,7,8 The lesion is usually unique. The bilateral cases are rare.14 Due to the lack of specific clinical and radiographic characteristics, it is important to establish the differential diagnosis between SBC and other bone lesions of the jaws, such as radicular cyst, keratocyst, ameloblastoma, myxoma, aneurysmatic bone cyst, lateral periodontal cyst, cherubism, focal osteoporotic bone marrow defect, intraosseous vascular malformations, and central giant cell lesions.2,7,9,10
The treatment of choice is a surgical curettage of the boné walls. This procedure produces bleeding in the cavity that leads to the organization of a clot, which will be the architecture of a new bone formation.1,7,8 In the absence of tissue for histopathological analysis, the clinical presentation at the time of surgical procedure is enough to establish the diagnosis.2,3,10,14
This study aimed to present a rare case of bilateral SBC, in a young 14-year-old male.
Case report
A 14-year-old male patient was referred to the Dentistry Course at Universidade Tuiuti do Paraná, to evaluate na asymptomatic bilateral intraosseous lesion in the mandible, which was discovered by chance during the routine follow-up with radiographs of the orthodontic treatment.
The anamnesis revealed a systemically healthy, sportsman, who played football regularly. The extra and intraoral clinical examination did not show any changes in normality, but the presence of an orthodontic appliance. The panoramic radiography showed, in the mandible body, two bilateral well-defined radiolucent areas, with irregular and sclerotic edges, and no signs of root resorption of the next teeth. On the right side, a unilocular lesion, that was extended from the canine to the second premolar was observed. On the left side, there was a significantly larger lesion, which involved the first premolar to the third molar, extending to the base of the mandible and scaling it between the dental roots (Figure 1). Computed tomography did not show expansion or rupture of the cortical bone (Figures 2, 3). The teeth associated with the lesions tested positive for sensibility. The panoramic radiography done before the installation of the orthodontic appliance, showed that the lesions were already present for at least six months. (Figure 4).
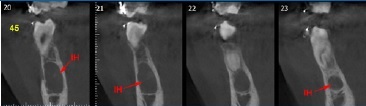
Figure 2 Sagittal section of cone-beam computed tomography (CBCT) of the mandible showing osteolytic lesion on the right side, with preservation of the boné cortex.
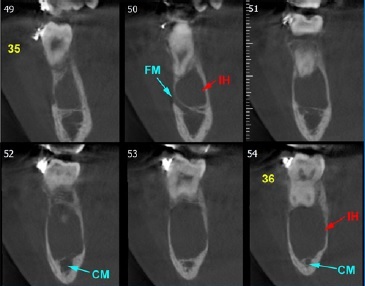
Figure 3 Sagittal section of cone-beam computed tomography (CBCT) of the mandible, showing osteolytic lesion on the left side and also showing a thinning of the bone cortex, but with no expansion or rupture of it.

Figure 4 Panoramic radiography performed before the beginning of the orthodontic treatment, showing the presence of bilateral lesions in the mandible.
Although the patient did not remember to have suffered a specific trauma in the face, he reported that this is a common happening in his daily sports practice. Based on the anamnesis and the clinical-radiographic aspect, the initial diagnostic hypothesis was that of a simple bilateral bone cyst, but the possibility of other cystic lesions or odontogenic tumors was not ruled out. Surgical exploration was suggested and na informed consent form, which also contained an authorization for the case report, was obtained from his mother. If the surgery did not reveal empty bone cavities, an excisional biopsy
on the right side and incisional biopsy on the left side, with possible installation of a drain for decompression, was planned.
Under local anesthesia, on both sides, an incision and complete detachment of the mucoperiosteal flap was performed, with local osteotomy to access the lesion. The presence of na empty bone cavity, without any apparent capsule, was observed, confirming the diagnosis of SBC (Figure 5). The curettage of the bone walls was performed, stimulating local bleeding and the formation and filling of the cavities with a blood clot (Figure 6). The mucoperiosteal flaps were repositioned and sutured with a 4.0 nylon thread. There was no soft tissue in the cavity for histologic examination.
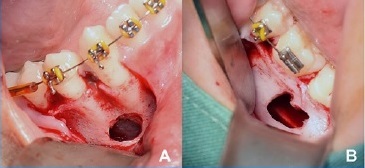
Figure 5 Transoperative view revealing empty boné cavities on both sides. A) Right side; B) Left side.
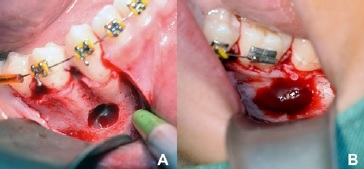
Figure 6 After a simple curettage, the complete filling with a blood clot is evident in both cavities. A) Right side; B) Left side.
The patient received the guidelines for postoperative care, the prescription of nimesulide 100mg/12 hours, for five days, and sodium dipyrone 500mg/6 hours, for three days, as a pain killer, if necessary. The stitches were removed on the seventh postoperative day, with good local healing and no pain complaints.
The radiographic follow-up was performed in the 4th, 8th and 16 th months, showing complete bone neoformation (Figures 7, 8).

Figure 7 Follow-up panoramic radiograph showing, after 4 months, the new bone formation in progress, and no signs of the recurrence of the lesions.
Discussion and conclusions
The simple bone cyst (SBC), also known as a traumatic boné cyst, is an uncommon osteolytic lesion, of benign characteristics and with no epithelial lining.2,4,9 It usually occurs unilaterally.
A case with bilateral involvement, such as the one described above, is poorly documented in the literature.9,10,14 Since the beginning of the 20th century, when it was first described, its true pathogenesis remains unknown.7,10 Trauma is supposed to be the main triggering factor. It forms an intraosseous hematoma and liquefaction of the blood clot that fails to be replaced by bone tissue. Resorption of the adjacente bone occurs through enzymes activated by the adjacente cells.1-3,7-9 Also, next to the trauma, a subperiosteal hematoma reduces the blood supply to the region causing an osteolysis process and subsequent formation of the lesion.2 However, the absence of an important traumatic injury reported by patients, makes the theory of trauma very questionable.1,7,8 More than 50% of the SBC cases have no traumatic involvement;8 in a systematic review, it was observed that only 1 in 4 cases of SBC were preceded by trauma.3 Besides, boxing athletes and other individuals who suffer frequent head and neck trauma are no longer affected by this type of injury.9
Another concept applied to the possible pathogenesis of SBC involves microtrauma of the teeth and alveolar crest.8 Some authors suggest the addition of an underlying systemic component in patients with multiple SBC, with a tendency to vascular anomalies.2,8 Others associate osteolysis caused by an altered bone metabolism.9 There is also the theory of synovial cysts arising from an error in the ossification process, where a synovial lining would occur in the affected region.2 In the theory of tumor degeneration, a pathological alteration such as fibrous dysplasia and central granuloma of giant cells would result in SBC after their liquefaction process.8,9,13
A retrospective study of 44 cases of SBC, pointed out a possible combination of these lesions with orthodontic treatment and some cases associated with florid bone cement dysplasia (DCOF).9 In this case, there is a misfunction in bone metabolismo leading to biochemical and hormonal changes resulting in osteolysis.8,9 Due to the disorganized mineralization of boné tissue, blockage of lymphatic drainage may occur, inducing the formation of the cystic space.7 The age of the majority of the patients affected by SBC coincides with those who undergo orthodontic treatment, ranging from 9 to 20 years of age.9 Possible pathogenesis is associated with tooth movement performed by orthodontic treatment, which promotes areas of tension and pressure that increase the vascularization in the region. The presence of vascular endothelial growth factors, tumor necrosis factors, and pro-inflammatory cytokines promote the activation of cellular receptors on macrophages, inactive osteoclasts, and undifferentiated cells that differentiate into mature osteoclasts, whose function is to mediate boné resorption.9 Besides, piezoelectricity also plays a role in the development of cystic spaces, as the generation of electrical potential in the bone caused by a displacement of mechanical charges influences the cellular activity of osteoclasts.9 In the present case there was the presence of two possible etiological factors, trauma and orthodontic treatment; although the patient could not remember a specific trauma, he mentioned that traumas in the face were very common during his sports activities.
Regarding the prevalence of SBC between gender, some studies found no difference.3 However, some authors claim that women are more affected, due to the high index of estrogen and lack of progesterone, especially at a young age, resulting in bone resorption and development of the lesion.9,10 Other authors, however, reported a predominance in males in their case series.7
Although SBC can be found at any age, there is agreement among the authors that younger patients, between the first and second decade of life, are the most affected, once they are the ones that suffer more traumatic injuries.1,3,7,11,12 A study with a case series finds a history of trauma in patients aged 14-22 years, as observed in the present case.9
The posterior region of the mandible2,3,7-9,11 is the most affected site by SBC, but lesions in the anterior region may occur.7,13 Maybe there are more cases in the mandible compared to the maxilla because the mandible has more cortical bone, which is repaired more slowly.7 However, the involvement of condyle, anterior maxilla, and zygomatic bone regions have also been described.2,3,9,12
Patients are usually asymptomatic, but in 20% of the cases they may present symptoms of pain, edema, tooth sensitivity, paresthesia, and in very rare cases, pathological fracture of the jaw.1-3 The absence of symptoms explains the detection of lesions by chance during routine radiographic examinations.3,8,10
The pulp tissue of teeth involved in the injury is vital. Color change, tooth mobility, or displacement are non-existent and there is no root resorption in most cases.2,9,11Pathological fractures are reported in 0.6% of the cases.3 In the present case, there was an imminent risk of injury to the left side if the diagnosis had been postponed. Mandibular fracture and damage to the lower alveolar nerve can occur in the presence of considerable bone resorption, due to the substantial growth of the lesion.2
A radiolucent image, with an irregular shape, well-circumscribed, and with well-defined borders is observed in radiographs.2,8,13 Lesions can be presented with an uni-or multilocular pattern, but unilocular is the most common.1,3,7,9,11 The multilocular lesions may be associated with unerupted and/or impacted teeth and are similar to tumors.7,9The presence of inter radicular scaling, as observed in the lesion on the left side of the present case, is highly suggestive of SBC, but it is not pathognomonic.9 Staggering around the roots of adjacente teeth is evident in 40% of the lesions.3 The majority of cases do not present bone expansion, but thinning of the cortical may be observed.3 Multiple lesions are more commonly associated with bone expansion, but they are rare.1,3 In a study with 132 SBC, multiple lesions accounted for 13% of cases.15 Damage to the mandibular canal will depend on the extent of the lesions and expansion of the cortical bone.2
The differential diagnosis should include odontogenic and nonodontogenic cysts and tumors, such as radicular cyst, keratocyst, ameloblastoma, myxoma, lateral periodontal cyst, and other lesions such as aneurysmal bone cyst, cherubism, focal osteoporotic bone marrow defect, intraosseous vascular malformations, and central giant cell lesions.7,10 The final diagnosis is established during the surgical procedure, by seeing the empty bone cavity, characteristic of SBC, excluding all the above lesions.1,2,10 The lesion, when discovered in the beginning, can reveal fluids inside. As it progresses, it usually becomes empty.8
Histopathological examination can detect fibrotic connective tissue and normal bone tissue.1 Some authors describe the lesion as fragments of fibrovascular connective tissue, cholesterol fissures, giant foreign body cells, with a protein portion of the cystic content containing bilirubin, similar to serum.2,8
Others say that the histology of the SBC reveals only a connective tissue membrane that lines the entire pathological cavity.7 The content for histological analysis is usually scarce.7,9 There is no protocol for the treatment of SBC in the maxillofacial region,12 however, a simple curettage is the most recommended procedure.1-3,7-9It also establishes the final diagnosis of the lesion.1,8The procedure consists of surgical exploration of the cystic cavity, which will display an empty or semi-empty space, followed by careful curettage of the bone walls, inducing bleeding and blood clot formation, filling the entire cavity, and ending with the suture of the wound.1-3,8 The new bone is similar to the one obtained with the placement of a local bone graft.14 Bleeding around the lesion is enough to trigger cell differentiation and, consequently, the regeneration of bone tissue in the affected region in a short time.1,3,10
The use of bone grafting materials to fill the cavities is also reported in the literature.10-12,14 For some authors it presents advantages, as early bone healing, preservation of the surrounding soft tissue, and recurrence is easily identified when it occurs.10 The placement of lyophilized bovine bone, autologous blood with autogenous bone, hydroxyapatite, bioglass, platelet-rich fibrin, cryogenic therapy, corticosteroid injection and surgical resection are some of the other proposed therapies.8,11,12,14 A simple curettage is the treatment of choice, with bone repair within 6 months and with an excellent prognosis.3,7,9
The spontaneous regression of the lesion can occur, and this fact would justify its low incidence in older age groups.2,3,14 However, the non-surgical intervention, with only radiographic follow-up throughout life, does not rule out other injuries.12 Besides, the patient is frequently exposed to radiation, and a pathological fracture can occur.3,12
Post-surgical follow-up, with radiographic exams is necessary. Panoramic radiographs are taken shortly after the surgical procedure. Some authors recommend within 1, 3, and 6 months and 1 year after surgery.2,4,10,11 On the other hand, for other authors it is more reasonable to perform the first radiographic examination between 12 and 17 months after surgery because this is the period within which most cases with healing were confirmed,15 Longer follow-up periods, from 22.8 to 25.3 months, have also been described.3
Altough recurrence of SBC of the jaws is assumed to be extremely rare,2,7,13one study found an overall recurrence rate of 26%.15 According to some radiographic findings, it is possible to predict the prognosis for SBC.3 Studies show that in multilocular lesions, the recurrence rate is 65.4%, versus 4.8% in cases of unilocular lesions.8 Multiple lesions are also associated with a higher probability of recurrence.15 Larger lesions, with an inter radicular staggering, which makes it difficult to form enough blood clot for bone repair, have a greater probability to persist or reappear;3 in the present case, despite the lesion on the left side having shown these characteristics, complete local bone formation was observed and, after 8 months, there was no sign of recurrence of the lesion.
Cases of bilateral SBC are rare in the literature. A thorough analysis of clinical and radiographic findings, combined with surgical treatment, contributes to the correct diagnosis and resolution of the lesion. In the present case this was achieved through a conservative surgical approach, based on simple curettage, recommended by many authors, which guaranteed a good prognosis for the patient. Finally, there is a need for more comprehensive research to better elucidate the true pathogenesis and the most appropriate treatment for SBC.

















