Introduction
The epithelioid hemangioma (EH) is a benign vascular neoplasm uncommon in the oral mucosa that was first described by Wells and Whimster in 1969 as angiolymphoid hyperplasia with eosinophilia (ALHE).1,2 Its most accepted and currently used denomination - epithelioid hemangioma - was proposed by Enzinger and Weiss in 1983. The same lesions it refers to received other denominations, such as ALHE, nodular angioblastic lymphoid hyperplasia with eosinophilia and lymphofolliculosis, pseudo pyogenic granuloma, atypical pyogenic granuloma, and inflammatory angiomatous nodule.3,4
Cutaneous EH affects a wide age range, reaching its peak in the third decade of life, and has no gender predilection.5 In the extraoral region, it can typically be seen in reddish-brown color, resembling an angioma, in the form of small nodules or papules and crusts with pruritus. The lesion is usually painless, affecting mainly the intradermal or subcutaneous region, especially in the head and neck, located in the auricular and preauricular area and scalp.5,6 Extracutaneous lesions are uncommon, with reports involving muscles, bones, orbits, and oral mucosa. 3,6-14
Cases of EH in the oral mucosa are rarely observed and, when they occur, seem to have a greater predilection for the male gender, especially young adults. The lips, tongue, buccal mucosa, and palate are the most commonly involved sites.12,13
The oral presentation of EH is non-specific, and the lesion can easily be confused with other lesions such as angioma, pyogenic granuloma, facial granuloma, insect bites, Kaposi’s sarcoma, salivary gland tumor, lymphoma, lipoma, and squamous cell carcinoma.3,6,12,13The diagnosis is based on the lesion’s clinical appearance and typical histopathological characteristics.6,12,15
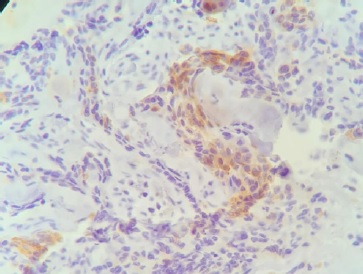
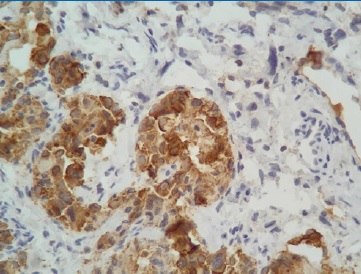
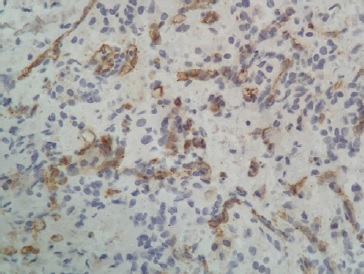
Histologically, the lesion is composed of well-formed round or ovoid vessels covered by epithelioid endothelial cells with a histiocytoid appearance; the vessels are surrounded by na infiltrate of lymphocytes and eosinophils.3,15,16 The immunohistochemistry of oral EH’s epithelioid endothelial cells is commonly immunoreactive for CD34 and antigen associated with factor VIII.3,6,11-14 The treatment of EH is performed through surgical excision. Although recurrence may be observed in one-third of cases of cutaneous EH,17 it is quite infrequent in the cases of the oral mucosa.6,12
The aim of this study was to report a rare case of oral EH in a 52-year-old female.
Case reportFigure 4
A 52-year-old white female was referred to the office of a stomatologist to evaluate a “stain on the gums.” The anamnesis revealed a systemically healthy patient medicated with calcium and vitamin D to control osteopenia who reported having a cervical hernia that would be surgically treated the following week. She brought the preoperative exams (blood count, coagulogram, blood glucose, creatinine, HIV), and all were normal. She also reported an annual medical check-up with her gynecologist, performed 3 months before, without any change in normality. When questioned about the lesion, the patient reported that it was asymptomatic and had been present for more than a year, with no change in size; however, in the previous month, the patient experienced local sensitivity and observed a change in color, which had become more intense. There was no history of local trauma.
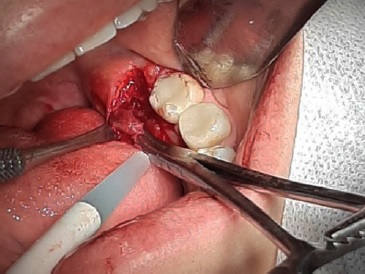
Extraoral physical examination revealed no change in normality. In the intraoral examination, a submucosal, well-delimited bluish-gray nodule of approximately 0.7 cm in diameter with a slight sensitivity to palpation was observed in the lingual gingiva of the left retromolar area (Figure 1). A conebeam computed tomography of the area showed no local boné alteration.
A vascular anomaly of the gingiva was suspected; diascopy was performed, and no alteration in the color of the lesion was observed. After signing an informed consent form, the patient underwent an excisional biopsy under local anesthesia, which revealed a round erythematous smooth nodule (Figures 2 and 3). There was no postoperative complication, and the patient returned 7 days later for removal of the sutures, with good local healing and no pain or paresthesia complaints.
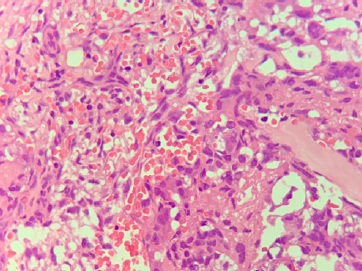
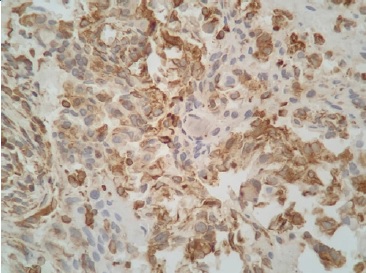
Figure 4 Histological aspect showing an epithelioid proliferation associated with an exuberant capillary vascular component in the mucous chorion
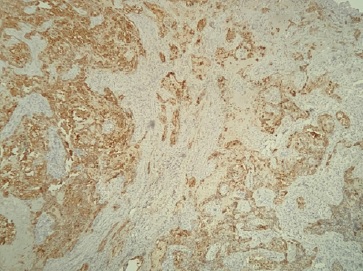
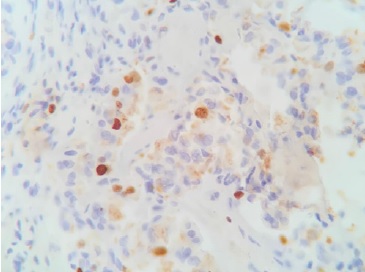
Immunohistochemistry results were positive for vimentin antibodies (Figure 5), AE1/AE3 (Figure 6), KI-67 in 10% of the cells (Figure 7), high-weight cytokeratin (Figure 8), diffusely positive cytokeratin 7 (CK7) in perivascular epithelioid cells (Figure 9), CD34 positive in several endothelial cells (Figure 10), and P63 in rare cells. The results were negative for protein S-100 and actin of smooth muscle 1A4 (with only positive internal control in vascular walls). The immunohistochemical study detected an increase of small vessels consistent with na epithelioid proliferation associated with a prominent vascular component, and the diagnosis of EH was established. The follow-up was performed every six months in the first year. Nowadays, the patient returns once a year for her anual oral check-up, and after 30 months, there is no sign of recurrence.
Discussion and conclusions
The epithelioid hemangioma (EH), also called angiolymphoid hyperplasia with eosinophilia (AHLE), is a benign neoplastic lesion composed of endothelial cells, rare in the oral cavity and recognized by the World Health Organization (WHO) as a vascular tumor.2,12
Although EH is considered a benign tumor, its exact etiology, whether neoplastic or reactive, has long been discussed.4,12 WHO classifies it as a benign neoplasm, but some authors state that its pathogenesis may be linked to other factors such as hypersensitivity reaction, inflammatory vascular manifestations, and infections or tissue reactions caused by trauma.2,3,11,14 In addition, sex hormones and high levels of sérum estrogen may be involved and may participate in the growth of the lesion.15 Association with HIV has also been reported in the literature.18 The hypothesis that EH is a reactive process is due to the greater occurrence of the lesion in sites above the bone, behaving symmetrically and organized around the larger vessels.4,12
Although its racial predilection has been little explored, EH is reported in several parts of the world, affecting Asians more.3,5 In one of the largest series of cases, however, there was a predominance in Whites, reaching 90% of cases, and a low occurrence in Blacks.15 The mean age of patients affected by oral EH is 37.7 years, with a higher incidence in males.12,13
In general, EH occurs more frequently in the head and neck skin, possibly in the scalp or the distribution of the superficial temporal artery, the forehead, the auricular pavilion, and the preauricular area.2-4,15 Generally, such lesions are sized 0.2 to 10 cm; larger sizes are usually rare.1,5,15 On the other hand, EH in the mouth is rare, with few cases reported in the literature.3,6,11-14
Clinically, the oral EH can manifest in various ways such as a macula, ulcer, crust, or nodule with a sessile or pedicled base, smooth or lobulated surface, painful or painless. However, the nodular presentation observed in the present case is the most common; the lesion may be single or grouped, na its coloration may vary from red to brown.3,6,11-14 The most frequently affected sites are the lips, buccal mucosa, tongue, and palate.12,13The main differential macroscopic diagnoses of oral EH are Kaposi’s sarcoma, pyogenic granuloma, lymphoma, squamous cell carcinoma, and salivary gland tumor.3,6,12,13
Despite the clinical similarity between EH, Kaposi’s sarcoma, and pyogenic granuloma, the histopathological characteristics of these diseases are quite distinct.15 The definitive diagnosis is usually based on each lesion’s typical clinical and histopathological characteristics.6,15 EH and Kimura’s disease (KD) have been described as a single disease but are now considered distinct entities.3,15,19 KD is characterized by subcutaneous edema also observed in the muscles and is associated with lymphadenopathy and eosinophilia in the blood; besides, serum IgE is clearly altered, which usually does not occur in EH.19
As EH is a rare disease of the oral mucosa, it is frequently confused with other soft-tissue lesions of non-vascular nature and vascular lesions with an epithelioid appearance.3 Therefore, histologically, EH in the oral mucosa should be distinguished from other vascular tumors that present epithelioid characteristics since some of these tumors, such as epithelioid hemangioendothelioma, epithelioid angiosarcoma, and bacillary angiomatosis, have different biological behavior, prognosis, and treatments.3,6,12
The histological characteristics of EH include a proliferation of blood vessels covered by prominent and enlarged endotelial cells, giving a typical appearance of cobblestones, nuclei that are typically ovoid, well symmetrical, and have intracytoplasmic vacuoles, and an abundant perivascular and interstitial infiltrate of lymphocytes and eosinophils around the vessels.2,3,14,16 Histological evidence of arteriovenous shunts is present in 42% of cases.15 In the present case, the morphological characteristics are consistent with epithelioid proliferation associated with a prominent vascular component.
Some authors reported that eosinophils are usually responsible for 5 to 15% of the infiltrate but may reach up to 50% in rare cases, and eventually, the infiltrate is devoid of eosinophils.3 Others point out that the presence of lymphocytes and eosinophils is not mandatory to establish the diagnosis of EH.2
Epithelioid endothelial cells of oral EH have been shown to be commonly immunoreactive for CD34 and factor VIII.3,6,11-14 Approximately 20% of patients with EH have eosinophilia in the blood, without increasing serum IgE levels, and around 19% may have lymphadenopathy;15 none of these alterations were observed in our patient.
Although epithelioid vascular tumors are difficult to diagnose due to their rarity, their correct diagnosis is of paramount importance to adequately treat the lesion.8 Histopathological examination is considered the gold standard to determine the definitive diagnosis of EH.5,12,15 However, in some cases, na immunohistochemical study may be necessary to establish the definitive diagnosis, as observed in the present case. Some authors state that the lack of objective molecular markers often impedes the diagnosis of EH and recommend an immunohistochemical panel including not only pan-cytokeratin AE1/AE3 and endothelial markers but also FOSB since it helps in the diagnosis of epithelioid vascular tumors.16 Despite its value for differential diagnosis, FOSB immunohistochemistry was not necessary to establish the final diagnosis in this case.
Regarding treatment, complete local excision is the optimal management of oral EH. Although there are several other treatment strategies such as corticosteroids, cryotherapy, pulsed light, intralesional chemotherapy, topical imiquimod, systemic propranolol, and interleukin-5 for cutaneous EH, they are rarely applied for oral EH.3,6,12 Topical imiquimod causes tumor regression through its apoptotic receptors; this therapy increases the innate and acquired immune response and activates the TH-1 cells, which provides a long-term memory of the immunological response.14 Propranolol is used when complete excision of the lesion is not possible or in cases of recurrence after excision; this therapy showed satisfactory short-term results without side effects.9,10 The interleucin-5-based therapy presented good results; this cytokine interferes in the differentiation and activation of the eosinophils, one of the fundamental stages in the pathogenesis of EH.20 The pulsed dye laser combined with the CO2 laser is a good alternative when na aesthetic treatment is necessary, without leaving deep scars.21
In a systematic review of EH, there were significant associations between earlier age of onset, longer disease duration, multiple lesions, bilateral lesions, pruritus, pain and bleeding, and higher rates of recurrence after excision. The authors stated that the finding of higher post-excision recurrence rates for multiple versus single lesions indicated that excision is probably more useful in unilesional or limited cases of EH and laser therapies are the main candidates for investigation in extensive cases.5 Recurrences in oral EH are quite uncommon and have been successfully treated with re-excision.6,12
EH is a rare lesion in the mouth, with a varied clinical manifestation, resembling other vascular and non-vascular lesions. Differentiation of EH from malignant epithelioid vascular tumors is of paramount importance because their clinical behavior and prognosis are very different. Although the histopathological findings generally establish the diagnosis of oral EH, in many cases, an immunohistochemical study may be necessary. Surgical excision is the most widely used form of treatment and, in the present case, has been effective so far, with no signs of recurrence 30 months after surgery.