Introduction
Approximately 15% of the global population currently suffers from a disability, and this number is increasing due to aging and the growing prevalence of non-communicable diseases.1 “Disability” encompasses a wide range of conditions, particularly physical, developmental, psychological, sensory, behavioral, or emotional changes or conditions that require medical treatment, health care intervention and/or even specialized services or programs.1 People with disabilities have a higher risk of developing oral pathologies due to having physical and/ or mental limitations that make it difficult to perform their oral hygiene, following a diet rich in carbohydrates and soft foods, having chewing or swallowing problems associated with reduced maxillofacial motor function and, possibly, neglecting oral hygiene.2,3
In Portugal, oral health (OH) initiatives are scarce in terms of prevention, treatment, and maintenance and fail to give information to caregivers.4 Moreover, just a few clinical centres provide dental care to people with disabilities. The most common reasons mentioned are the lack of professionals with specialized training, communication barriers, control of behavioral characteristics, and geographic aspects. 2,4,5OH care for people with disabilities requires a level of specialization, specific knowledge, and adaptive techniques beyond those considered routine in the training base program of OH professionals.
In addition to its teaching mission, the Faculty of Dental Medicine of the University of Lisbon (FMDUL) provides OH care to the community, including people with disabilities.6 The Dental Hygiene Clinic for People with Disabilities at FMDUL University Clinics has been operating since 1987. It is specialized and focused exclusively on people with disabilities (mostly profound disabilities) and is the only clinic of its kind in the country. This clinic operates weekly, and there are about 450 appointments annually.
The aims of this study were to analyze the appointment flow of people with disabilities at FMDUL Dental Hygiene Clinic in order to characterize its clients and study their dental state by type of disability, level of dependency, oral hygiene difficulty, and frequency of appointments.
Material and methods
This observational, analytical, cross-sectional study had a non-probabilistic sample of individuals who attended the FMDUL Dental Hygiene Clinic for People with Disabilities. The study was authorized by the FMDUL Ethics Committee, following the international guidelines of the Declaration of Helsinki.
Subsequently, authorization was requested from the Clinical Management Board of FMDUL to analyze the physical clinical records of the individuals who attended the appointment in a period of five years, between January 2015 and December 2019 (Figure 1).
One researcher collected data between January and March 2021 by analyzing each individual’s clinical records. Data collected comprised sociodemographic data and general health data like main disability (rare diseases or syndromes were grouped into a single variable - “other pathologies”) and comorbidities, medication, level of dependency, dental hygiene habits and difficulties performing it, and the number of appointments attended. The level of dependency was classified as independent (daily living activities without help), semi-dependent (difficulty in feeding, mobility, and hygiene), and dependent (every daily living activity with help). OH clinical data included the decayed, missing, and filled teeth (DMFT) index,7 the simplified oral hygiene índex (DI-S),8 and the simplified gingival index (GI-S).9 The medication was registered by the official Portuguese Pharmacotherapeutic Classification, corresponding to the “Anatomical Therapeutic Chemical Code” (ATC) of the World Health Organization.10
The data collection was statistically analyzed using the Statistical Package for the Social Sciences software program (IBM SPSS 26.0). Association tests were performed between dental health status and the variables under study. The Shapiro-Wilk test was used to assess the normality of continuous variables, and the Mann-Whitney and Kruskal-Wallis tests were used as non-parametric alternatives, with Bonferroni correction, for variables that did not follow a normal distribution. Significance was set at a p value ≤0.05.
Results
Between 2015 and 2019, 3120 appointments were made to 654 individuals, averaging 624 appointments per year. In the period studied, there were 207 new individuals in the Dental Hygiene Clinic for People with Disabilities. Ninety-nine individuals were excluded due to missing charts, incomplete data, or death. Thus, the final study group included 555 individuals (Figure 1).
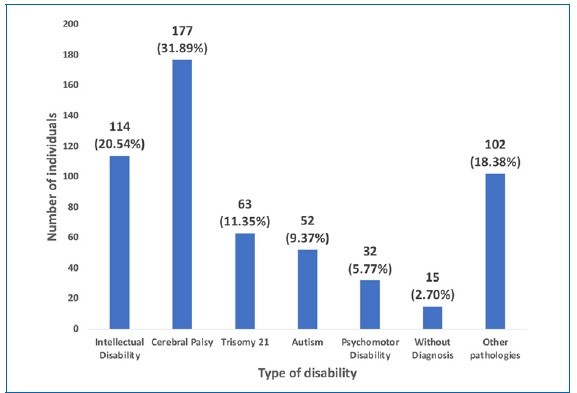
The average age of individuals was 37.05 (±13.9), and most were male (311; 56%). The majority lived in the district of Lisbon (511; 92.3%), and 407 (73.3%) were institutionalized. Cerebral palsy was the most prevalent pathology (177; 31.8%), followed by intellectual disability (114; 20.5%) (Figure 2). Epilepsy was the most reported comorbidity (152; 27.3%), followed by respiratory problems (83; 15%). Each individual took an average of 2.20 (±2.07) drugs, with predominance for the central nervous system group in 360 (64.9%) of the cases.
Regarding daily activities, 187 (34%) individuals were independente in activities of daily living (such as eating, bathing, and dressing), 104 (18.7%) did not communicate, 192 (34.6%) had difficulty speaking, and 135 (24.3%) used wheelchairs. In terms of diet and chewing difficulties, 89 (16.7%) individuals followed a soft or liquid diet, and 112 (21%) had poor chewing.
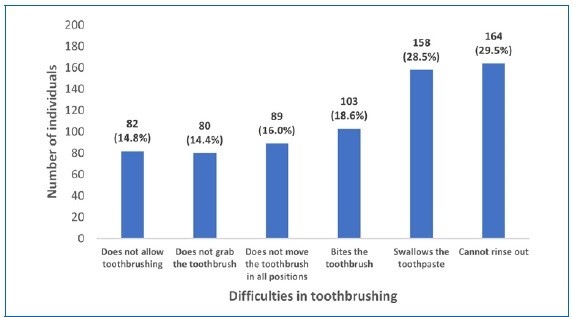
The caregivers mentioned several difficulties regarding toothbrushing (Figure 3).
During the last dental hygiene appointment, 187 (33.7%) individuals had not cooperated, requiring adaptive techniques such as head stabilization (172; 31%), limbs stabilization (115; 20.7%), the use of bite blocks (113; 20.4%), and/or velcro straps (6.1%).
The DMFT index, registered in 532 individuals at the last appointment, was 9.51 (±7.49), with a higher contribution from the missing teeth component (4.30±5.46), and about a half of the individuals were free from active caries (223; 46.9%). Individuals with intellectual disability showed the highest DMFT (11.31) as well as a higher value for decayed teeth (3.05) (p<0.001). Individuals with trisomy 21 had the highest number of missing teeth (5.36) (p<0.001). Regarding the GI-S and DI-S, no statistically significant differences were found between the main disabilities (Table 1).
Table 1 Distribution of the mean decayed, missing, and filled teeth (DMFT) index, simplified gingival index (GI-S), and simplified oral hygiene index (DI-S) by type of disability.

Kruskal-Wallis test with Bonferroni correction; *statistically significant. Values that share the same letter are not significantly different
The level of dependency in activities of daily living and the autonomy in toothbrushing were associated with DMFT (p<0.001) and missing (p<0.001) and filled componentes (p<0.001), with lower values in all these variables in the dependente individuals. The GI-S was only associated with toothbrushing autonomy, with the semi-dependent individuals presenting the highest result (p=0.013). The DI-S results did not yield statistical significance regarding the level of dependency (p=0.468) and toothbrushing autonomy (p=0.196) (Table 2). The individuals that presented a higher toothbrushing frequency had lower GI-S and DI-S means (p=0.03 and p=0.01, respectively), as well as less decayed teeth compared to those that never or rarely toothbrushed (p=0.008) (Table 2).
Table 2 Association between dependency level, autonomy, and frequency of toothbrushing and the mean decayed, missing, and filled teeth (DMFT) index, simplified gingival index (GI-S), and simplified oral hygiene index (DI-S).
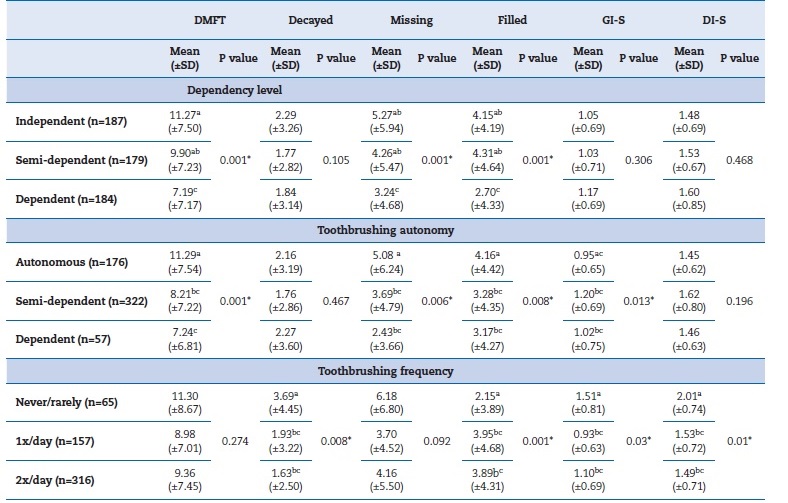
Kruskal-Wallis test with Bonferroni correction; *statistically significant; Values that share the same letter are not significantly different
The DMFT mean was higher in individuals who attended the clinic for longer (p<0.001), but the decayed teeth componente was lower in this group (p<0.001). No significant diferences were found in the GI-S and DI-S, although the mean values were lower in the group that came to 6-10 appointments in the last 5 years. The individuals who had attended the clinic for longer had the lowest DI-S mean but the highest GI-S mean.
The individuals who cooperated during the appointments had higher DMFT mean (p<0.001), missing teeth (p<0.001), and filled teeth (p<0.001) when compared to the uncooperative group. On the other hand, the decayed teeth (p=0.02), GI-S mean (p<0.001), and DI-S mean (p=0.004) were higher in the uncooperative group (Table 3).
Table 3 Association between appointment frequency, date of the first appointment, behavior, and number of techniques and the mean decayed, missing, and filled teeth (DMFT) index, simplified gingival index (GI-S), and simplified oral hygiene index (DI-S).
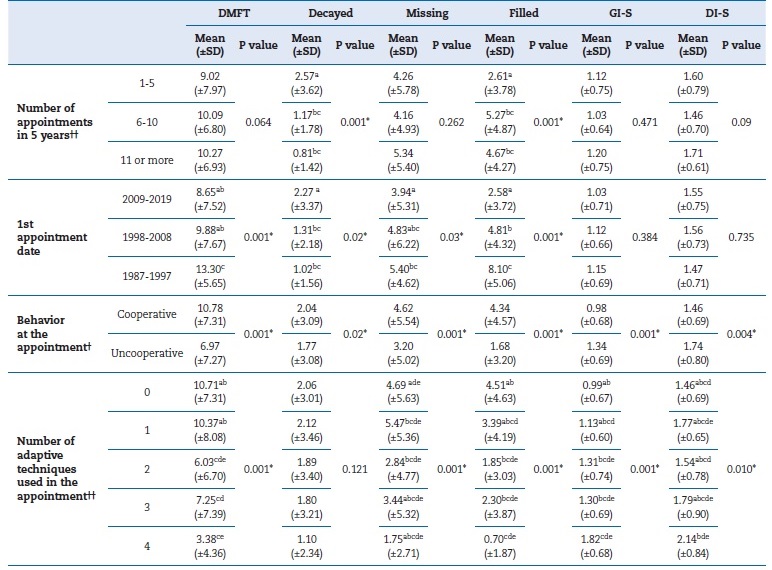
† Mann-Whitney test; †† Kruskal-Wallis test with Bonferroni correction; *statistically significant. Values that share the same letter are not significantly different
Discussion
The present study aimed to characterize the individuals who attended the FMDUL Dental Hygiene Clinic for People with Disabilities between 2015 and 2019 and to analyze whether their main disability, level of dependency, oral hygiene difficulty, and frequency of appointments influenced their dental status.
Since 2010, when another study was made in the same university clinic,5 the number of annual appointments increased, despite the decreased number of first ones, probably owing to the increase of private clinics providing dental care treatments to this population group. On average, each individual attended one appointment per year. The recommendation for adults is to visit an OH professional twice a year. Nevertheless, this frequency should be based on the impact of routine visits on dental and periodontal health,11 and the assessment of OH indexes.12 Moreover, because people with disabilities face difficulty in maintaining effective control of the oral biofilm and have cognitive, physical, and behavioral limitations that influence cooperation in appointments, they may have a greater risk of developing oral diseases,13 which justifies shorter maintenance intervals.
The institutionalized individuals had a higher frequency of appointments, as in the study by Bizarra,14 but lower than described in a systematic review with people with intelectual disabilities.15 The institutions choose the FMDUL University Clinics for their clients’ dental treatments, and this agrees with international studies that indicate that this population seeks community or hospital services more frequently.16,17
Since most individuals were residents of the Lisbon area, they were closer to the University Clinics, which can facilitate access to dental treatments. However, the aging of this population and of their parents/caregivers poses difficulties. Additionally, 33.5% of the individuals were dependent, sometimes requiring the help of more than one person to accompany them to the appointment. Also, approximately a quarter of this population used a wheelchair, with an increase since 2010.5
For individuals from other districts of the country, it becomes more expensive to come to the clinic using their own car or, when there are no other options, by requesting ambulance services that must be paid.
Regarding the adaptive techniques used, there was an increase in the use of the stabilization head technique and the bite blocks compared to 2010.5 This increase might be justified by the 207 new clients, who could not yet feel confident in the clinical environment, or maybe because individuals were older or had suffered worsening of their clinical condition over time.
Estimations indicate that 74.3% of the Portuguese population brushes their teeth twice or more daily.14 Comparatively, in the present study, there was a twice-daily toothbrushing frequency in 56.9% of the patients, a higher value than in 2010.
The toothbrushing autonomy dropped to 37.6%, which was expected considering the increased number of dependent individuals and their aging.5
The DMFT value found agrees with other studies on people with disabilities18-20 and with the national study on the prevalence of oral diseases in Portugal.21 These results show that despite the barriers and added difficulties in accessing dental treatments this group faces, their OH can be similar to that of the general population.
The tooth loss in this population is high since extraction can be the treatment of choice in urgent/painful situations due to the lack of cooperation from the individuals during appointments. In addition, oral rehabilitation is very limited in this population.5,14,19,22,23
Other studies report that the filled teeth contribute less to the total value of DMFT, which reflects that restorative strategy is not the treatment choice in this population.24,25It should be emphasized that the component of decayed teeth was lower than the filled teeth in this study, which is only possible because there is an organized service for dental treatment.
Compared to 2010, the mean of decayed teeth decreased, and the mean of filled teeth rose. These results might indicate that the appointment is effective in preventing and controlling dental caries and that more dental treatments are being performed when needed.5
Studies in people with disabilities describe inflammation and gingival bleeding related to poor control of oral biofilm levels.22,26 In this study, the GI-S and DI-S means were lower than the previously recorded, possibly because the study sample includes individuals who had already attended this appointment in 2010 and improved their oral hygiene habits through follow- up.5 Even so, the GI-S and DI-S were higher in individuals who had attended appointments for more years, demonstrating that even with follow-up appointments, under maintenance, some oral problems persist.11 The individuals who required help for toothbrushing and were uncooperative in the appointment showed a higher value of gingival bleeding, which reflects the importance of motor skills in the maintenance of OH.27
Awareness of this population’s oral hygiene difficulties is important to identify ways to control oral biofilm and the diseases resulting from its presence. It is crucial to insist on OH education for the caregivers and training of students in the OH field on providing care for people with disabilities.18,19
The limitations of this study were the irregular completion of the clinical charts or the fact they were not archived, maybe due to difficulties during the appointment, making the collection or updating of some data impossible.
Conclusions
The study of the individuals who attended the Dental Hygiene Clinic for People with Disabilities indicates that the OH indicators are positive. However, the results are influenced by the dependency on activities of daily living and autonomy in performing oral hygiene, as well as by the cooperation in the appointment. Thus, it is important to promote this service of FMDUL for people with disabilities, which continues to be a fundamental resource for this population and essential in preventing oral diseases and maintaining their OH.