Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Obstétrica e Ginecológica Portuguesa
versión impresa ISSN 1646-5830
Acta Obstet Ginecol Port vol.10 no.3 Coimbra set. 2016
CASE REPORT/CASO CLÍNICO
Caudal regression syndrome: a case of early prenatal diagnosis without maternal diabetes
Síndrome de regressão caudal: um caso de diagnóstico pré-natal precoce sem diabetes materna
Mariana Mouraz*, Joana Cominho*, Cátia Gameiro**, Joana Pauleta**, Sónia Pedroso**
Obstetrics and Gynecology Dept., Hospital Dr. José de Almeida, Cascais, Portugal
*Interna do Internato Complementar de Ginecologia e Obstetrícia
**Assistente Hospitalar de Ginecologia e Obstetrícia
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Caudal regression syndrome (CRS) is a rare and severe syndrome in which a segment of the lumbo sacral spine and spinal cord fails to develop. CRS is generally diagnosed at prenatal assessment, commonly in the late second trimester. The pathogenesis is still unclear, however its relationship to maternal diabetes is well established. The authors report a case of CRS diagnosed at 17 weeks of gestation.
Keywords: Lumbosacral region/abnormalities; Spinal cord/abnormalities; Ultrasonography; Prenatal diagnosis
Introduction
Caudal regression syndrome (CRS) is a complex, heterogeneous constellation of congenital caudal anomalies affecting the caudal spine and spinal cord, the hindgut, the urogenital system, and the lower limbs1.
CRS is caused by developmental field defects of blastogenesis involving the caudal mesoderm2. Evidence has indicated that maternal diabetes may play a role in the pathogenesis of this condition2.
CRS is estimated to occur in 1 to 2.5 per 100,000 pregnancies3,4. This anomaly is much more common in infants born to mothers with diabetes. It affects 1 in 350 of these newborns, representing an increase of about 200-fold over the rate seen in the general population4, 5. Diabetes is a major risk factor for CRS. CRS, being it the most characteristic fetal abnormality of diabetic embryopathy3.
Case report
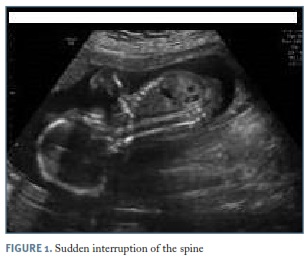
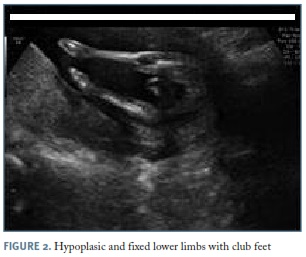
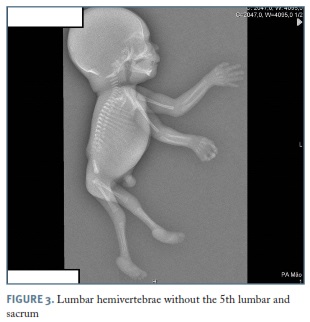
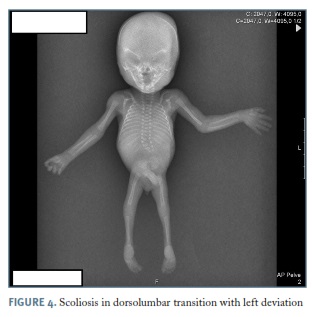
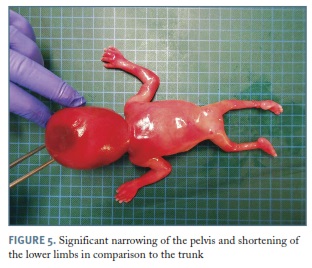
A 32-year-old healthy primigravid woman was referred to our unit from primary care at 13 weeks of gestation because of nuchal translucency superior to P95, absence of nasal bone and a hyperflexion fetal position. There was no history of maternal diabetes, ingestion of drugs besides folic acid or genetic anomalies. First trimester combined screening for trisomy 21 was 1/704. The ultrasound was repeated at 14 weeks and revealed equinovarus feet, beyond the changes described in the previous ultrasound. Vaginal ultrasound was not performed, because woman did not allowed. Invasive prenatal diagnosis was proposed and accepted by the couple, which revealed a 46, XY karyotype. At 17 weeks of gestation the ultrasound showed a sudden interruption of the fetal spine (Figure 1) and hypoplasic and fixed lower limbs with club feet (Figure 2). These findings were strongly suggestive of the CRS. Two weeks later the ultrasound was repeated and revealed shortened column with absence of sacrum and fusion of iliac wings. It also showed genitourinary changes: left hydronephrosis and genital hypoplasia. Other organ system examinations and placenta looked normal for gestational age. After counseling about the fetus’ sonographic findings and probable complications after birth, the couple opted for the interruption of the pregnancy. Radiological studies and autopsy findings of the fetus confirmed the diagnosis. Postpartum radiologic examination showed absent lumbosacral vertebrae and a hypoplastic pelvis (Figures 3, 4). Autopsy examination demonstrated shortening of the lower limbs and narrowing of the pelvis, anomalies of lumbar-sacral column (Figures 5, 6), consisting of 4 lumbar hemivertebrae and absence of the 5th lumbar vertebra and the sacrum, no anal canal, imperforate anus and shortening with absence of distal spinal cord.
Discussion
CRS is a rare anomaly, with about 300 cases reported, characterized by abnormal development of the caudal spine of the developing fetus6-8. This syndrome presents varying degrees of distal neural tube disruption, may include incomplete development of the sacrum and, to a lesser extent, the lumbar vertebrae, disruption of the distal spinal cord and extreme lack of growth of the caudal region7.
The embryologic insult occurs at the midposterior axis mesoderm and the lesion originates before the 28th day of gestational period which interfere with the formation of notochord, resulting in abnormal development of caudal structures5,8,9. Advances in the understanding of axial mesoderm patterning at early gestation reveal that a process of primary neuralization is compromised3,10.
Maternal diabetes, genetic predisposition and vascular hypoperfusion have been proposed as possible causative factors1, 9. Although diabetes is the major risk factor for CRS it also occur in non-diabetic women, as in our case, with confounding etiologic factors. More recently has been suggested a drug-related etiology with minoxidil and trimethoprim-sulfamethoxazole3,11.
Identification of skeletal dysplasias was relatively easy, but the ability to make an accurate specific antenatal diagnosis was more difficult12. CRS is generally diagnosed at prenatal assessment3,5. This article reported an early prenatally diagnosed case of CRS.
Prenatal ultrasound is the best method to diagnosis this anomaly. Ultrasonographic findings are variable and will depend on the extent and severity of the defect7. In first trimester we may suspect of such a case of CRS if we find: short crown-rump length, “protuberance” of lower spine, increased nuchal translucency and abnormal yolk sac11. In the second and third trimester we can find: abrupt termination of spine (best seen on sagittal section), no spine visible on axial views of abdomen and short trunk11. Many additional anomalies are common and may be observed, most frequently involving the muscle-skeletal (iliac wings approximated or fused, clubfeet and lower extremities contractures), genitourinary (cystic renal, dysplasia, hydronephrosis, penoscrotal inversion, penile agenesis and cryptorchidism), gastrointestinal (anorectal and duodenal atresia), central nervous (Chiari II malformation) and cardiovascular (congenital heart disease) systems4,7,8,11,13. In our case clubfeet, flexion contractures of hips and knees were the orthopedic deformities. Hydronephrosis and penile hypoplasia were the associated genitourinary malformations. There were no gastrointestinal, central nervous system or cardiac anomalies described in ultrasound in our case report. Diagnosis is usually made by demonstrating the termination of lumbar spine and small and abnormal lower extremities5. Absent sacrum with hypoplastic lower extremities is the best diagnostic clue11. Magnetic resonance findings have a potential benefit for associated anomalies, especially in obese pregnant11.
In differential diagnosis sirenomelia, segmental spinal dysgenesis (SSD), myelomeningocele and VACTERL association should be evaluated5,11. Sirenomelia was formerly thought to be an extreme form of CRS, but it is reclassified to be considered a separate entity8. Sirenomelia is a rare, lethal, congenital anomaly characterized by single fused lower extremities and renal agenesis with severe malformations of the gastrointestinal, genitourinary, cardiovascular and musculo-skeletal systems6,11,14. SSD is a rare spinal congenital anomaly characterized by localized agenesis or dysgenesis of the lumbar or thoraco-lumbar spine, severe congenital kyphosis or kypho-scoliosis and focal abnormalities of the underlying spinal cord and nerve roots13. SSD and CRS probably represent two faces of a single spectrum of segmental malformations of the spine and spinal cord5,11,15. VACTERL association includes combination of abnormalities: vertebral, anorectal, cardiac, tracheoesophageal, renal and limbs11. All anomalies described above were excluded.
The prognosis for children with CRS depends on the severity of the lesion and the presence of associated anomalies5. However, given the severity of some cases it may be an indication for termination of pregnancy, as ours.
The authors concluded that this syndrome can be diagnosed sooner than is described in the literature and may be seen without any risk factors. Early prenatal diagnosis of CRS, which has a high morbi-mortality rate, gives parents time to make informed decisions that at a later gestational age may not be available and allows for earlier less traumatic termination of pregnancy.
REFERENCES
1. Al Kaissi A, Klaushofer K, Grill F. Caudal regression syndrome and popliteal webbing in connection with maternal diabetes mellitus: a case report and literature review. Cases J. 2008 Dec 19;1(1):407. [ Links ]
2. Rougemont AL1, Bouron-Dal Soglio D, Désilets V, Jovanovic M, Perreault G, Laurier Oligny L, Fournet JC. Caudal dysgenesis, sirenomelia, and situs inversus totalis: a primitive defect in blastogenesis. Am J Med Genet A. 2008 Jun 1;146A(11):1470-1476.
3. Yeniel AÖ, Ergenoğlu AM, Sağol S. Prenatal diagnosis of caudal regression syndrome without maternal diabetes mellitus. J Turk Ger Gynecol Assoc. 2011 Sep 1; 12(3):186-188.
4. Bicakci I, Turgut ST, Turgut B, Icagasioglu A, Egilmez Z1, Yumusakhuylu Y. A case of caudal regression syndrome: walking or sitting? Pan Afr Med J. 2014 May 26; 18:92.
5. Aslan H, Yanik H, Celikaslan N, Yildirim G, Ceylan Y. Prenatal diagnosis of Caudal Regression Syndrome: a case report. BMC Pregnancy Childbirth. 2001;1(1):8. [ Links ]
6. Das SP, Ojha N, Ganesh GS, Mohanty RN. Conjoined legs: Sirenomelia or caudal regression syndrome? Indian J Orthop. 2013 Jul;47(4):413-416. [ Links ]
7. González-Quintero VH, Tolaymat L, Martin D, Romaguera RL, Rodríguez MM, Izquierdo LA. Sonographic diagnosis of caudal regression in the first trimester of pregnancy. J Ultrassound Med. 2002 Oct; 21(10):1175-1178 [ Links ]
8. Sharma P, Kumar S, Jaiswal A.Clinico-radiologic Findings in Group II Caudal Regression Syndrome. J Clin Imaging Sci. 2013 Jun 29;3:26. [ Links ]
9. Mandour C, El Mostarchid B. A rare congenital malformation: caudal regression syndrome. Pan Afr Med J. 2013;14:30. [ Links ]
10. Garcia T, Libório R, Pais R, Gonçalves O, Seabra J, Pais FF. Caudal regression syndrome. Lumbo-sacral agenesis. Acta Med Port. 2001 Jan-Feb;14(1):83-88.
11. Woodward PJ, Kennedy A, Sohaey R, Byrne JLB, Oh KY, Puchalski M. Diagnostic imaging - obstetrics (1st Edition). Amirsys; 2005: 14-17 (3).
12. Parilla BV, Leeth EA, Kambich MP, Chilis P, MacGregor SN. Antenatal detection of skeletal dysplasias. J Ultrasound Med. 2003 Mar;22(3):255-258. [ Links ]
13. Khemakhem R, Toumia HB, Francoise Ben Dridi M, Chaouachi B. Caudal regression syndrome. Tunis Med. 2012 Apr;90(4):342. [ Links ]
14. Seidahmed MZ, Abdelbasit OB, Alhussein KA, Miqdad AM, Khalil MI, Salih MA. Sirenomelia and severe caudal regression syndrome. Saudi Med J. 2014 Dec; 35 Suppl 1:S36-43. [ Links ]
15.Pahwa S, Garg A, Mishra NK. Segmental spinal dysgenesis: a rare malformation of the spinal cord. Neurol India. 2010 Mar-Apr;58(2):334-335.
Endereço para correspondência | Dirección para correspondencia | Correspondence
Mariana Mouraz
Hospital de Cascais
E-mail: mariana_mouraz@hotmail.com
Recebido em: 18/5/2015
Aceite para publicação: 15/9/2015