Serviços Personalizados
Journal
Artigo
Indicadores
Links relacionados
Compartilhar
Acta Obstétrica e Ginecológica Portuguesa
versão impressa ISSN 1646-5830
Acta Obstet Ginecol Port vol.11 no.1 Coimbra mar. 2017
ORIGINAL STUDY/ESTUDO ORIGINAL
Shoulder dystocia: obstetric maneuvers and its morbidity
Distócia de ombros: manobras obstétricas e morbilidade associada
Maria Carvalho Afonso*, Andreia Fonseca*, Nuno Clode**, Luis Mendes Graça***
Departamento de Obstetrícia, Ginecologia e Medicina da Reprodução Clínica Universitária de Obstetrícia e Ginecologia, CHLN - Hospital Universitário de Santa Maria
*Interna da especialidade de Obstetrícia e Ginecologia
**Chefe de serviço de Obstetrícia e Ginecologia
***Director de serviço de Obstetrícia e Ginecologia e Professor catedrático
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Shoulder dystocia (SD) is known for being an unpredictable and unpreventable event associated to substantial morbidity to the mother and neonate. The aim of this study was to determine the incidence of SD in a tertiary care hospital and the morbidity according to the type of maneuvers (McRoberts’ maneuver and suprapubic pressure versus rotational maneuvers or delivery of the posterior arm) used to resolve the dystocia.
Methods: This was a prospective cohort study of pregnancies complicated with SD carried during two years and a half. Maternal characteristics, duration of second stage of labor, type of delivery, fetal weight, neonatal morbidity (Apgar score <7 at 1st minute, type of injury, neonatal intensive care unit admission) and maternal morbidity (3rd or 4th degree laceration, cervical tear, post-partum hemoglobin < 8g/dL, perineal haematoma, post-partum fever, dehiscence of episiotomy) were collected. According to the maneuver performed, data were compared using Chi-square test, Fischer exact test or Student t test, as appropriate. A p-value of < 0,05 was considered significant.
Results: During the study period 123 (3.3%) pregnancies were complicated with SD. Baseline patient characteristics for age, parity, BMI, weight gain did not vary significantly according to type of maneuver. Rotational maneuvers and delivery of the posterior arm were associated to longer second stage of labour (60 min vs 45 min), higher proportion of instruments applied in a transverse fetal head position (30%) and increased neonatal (45%) and maternal (27%) morbidity.
Conclusion: Although rare, SD is associated to increased neonatal and maternal morbidity, specifically when rotational maneuvers and delivery of posterior arm are used.
Keywords: Shoulder dystocia; Obstetric emergency; Obstetric maneuvers; Maternal morbidity; Neonatal morbidity.
Introdução
Shoulder dystocia (SD) is defined as a delivery where an additional manoeuvre beyond gentle traction of the fetal head is needed to complete the baby delivery. It occurs in 0.2 to 3.0 percent of all births1,2. Although the effort on trying to find risk factors ante and intrapartum, most of the cases can not be anticipated, therefore SD its known for being an unpredictable and unpreventable event.
In order to expedite the delivery, many maneuvers have been described for successful disimpact of the anterior shoulder behind symphysis pubis. The choice of the maneuver should be based on the degree of invasiveness of the maneuvers, individual training and clinical experience, as well as the prevailing circumstances3. Tough, it is acceptable that we should begin with the least invasive maneuvers (suprapubic pressure and McRoberts tecnique) and, if unsuccessful, moving on to more invasive ones1,4.
The main goal of management of SD is to prevent fetal asphyxia and permanent Erb’s palsy or death, but on the other hand to avoid physical injury - fetal fractures and maternal trauma. The exact incidence and type of fetal injury has been difficult to determine because of the fact that not all SD cases have a comprehensive documentation of the involved procedures and/or information on adverse neonatal outcomes5. The aim of this study was to determine the incidence of SD in a tertiary care hospital and the risk factors associated to morbidity according to type of maneuvers (McRoberts’ maneuver and suprapubic pressure versus rotational maneuvers and posterior arm delivery) used to solve the problem.
Methods
This was a prospective cohort study of pregnancies complicated with SD between 1st June of 2012 and 31st December of 2014, in our institution. SD was defined according to the American College of Obstetricians and Gynaecologists’ (ACOG) practice bulletin as “the requirement of additional obstetric maneuvers to release the shoulders after gentle downward traction has failed”1. In our institution, prophylactic maneuvers are not performed routinely, but in case of SD, McRoberts and supra-pubic pressure are always the first maneuvers to perform.
All singleton cephalic pregnancies were included. In the cases were SD was diagnosed maternal characteristics, duration of second stage of labor, type of delivery, fetal weight, neonatal morbidity (Apgar score <7 at 1st minute, type of injury, neonatal intensive care unit admission), neonatal injury (brachial plexus injury, fracture of the clavicle or humerus diagnosed by radiography, hypoxic-ischemic encephalopathy or neonatal death) and maternal morbidity (3rd or 4th degree laceration, cervical tear, post-partum hemoglobin <8g/dL, perineal haematoma, post-partum fever, dehiscence of episiotomy) were collected from hospital medical records. We did not considered bruising, cephalo-hematomas or other soft tissue injuries that could have resulted from the management of the shoulder dystocia as neonatal injury.
The final maneuver used to release the impacted shoulders was considered the successful one. The cases were divided into the following two groups: (1) those solved through McRoberts and supra-pubic pressure and (2) those requiring rotational maneuvers and posterior arm delivery.
Statistical analysis was conducted using Statistical Package for the Social Science for Mac version 10.0 (SPSS Inc., Chicago, IL, USA). Continuous variables were compared using the Student’s t-test for different sample sizes. Nominal and categorical variables were compared using the χ2-test. The level of statistical significance was set at p < 0.05.
Results
During the study period, there were 123 cases (3.3%) of SD among 3746 vaginal deliveries. In 78, (64%) McRoberts’ maneuver and supra-pubic pressure solved the SD and in 45 (36%) further maneuvers were needed.
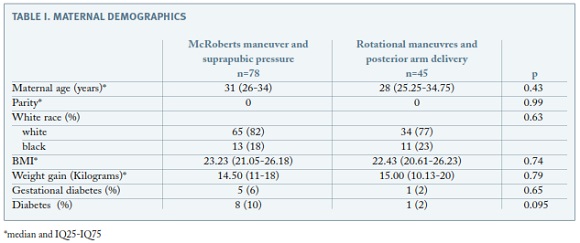
Maternal demographics are presented in Table I. Baseline patient characteristics for age, parity, BMI, weight gain in pregnancy did not vary significantly according to type of maneuver used to resolve the SD. There was just one patient with history of SD in a previous pregnancy she was in the group where rotational maneuvers or delivery of posterior arm were necessary to resolve SD. The proportion of women with either gestational diabetes or pre-existing diabetes was not statistical different between groups.
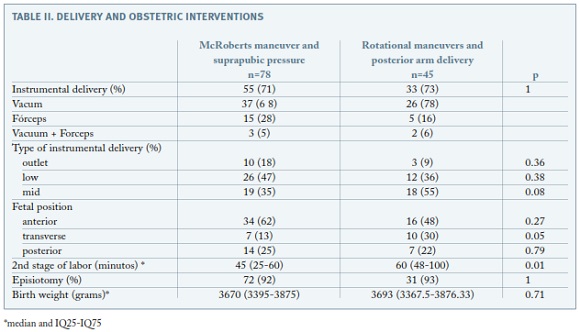
Obstetric management is detailed in Table II. Instrumental delivery was performed in the same proportion between groups. Although no statistically significant difference in the type of operative vaginal delivery (mid, low, outlet) was noted, when the instrument was applied in a transverse position of the fetal head the rate of rotational maneuvers or delivery of posterior arm were higher. The duration of second stage of labor was longer in the group of women who needed further rotational maneuvers (45 minutes versus 60 minutes, p= 0.014). The median birth weight of the neonates was not different between the groups. All women had epidural/sequencial anesthesia.
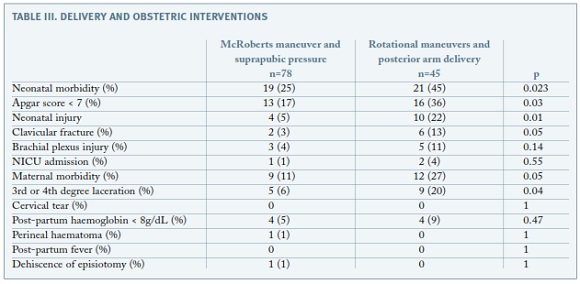
Rotational maneuvers and posterior arm delivery for resolution of SD resulted in higher percentage of neonates with Apgar score <7 at the first minute (36%, p= 0.03) and clavicular fracture (13%, p=0.05), with no further increase in brachial plexus injury (4% versus 11%, p=0.14). No case of humerus fracture, hypoxicischemic encephalopathy and neonatal death were reported. Regarding to maternal morbidity, with the need of more extensive maneuvers there was an increased likelihood of 3rd or 4th degree lacerations (20%).
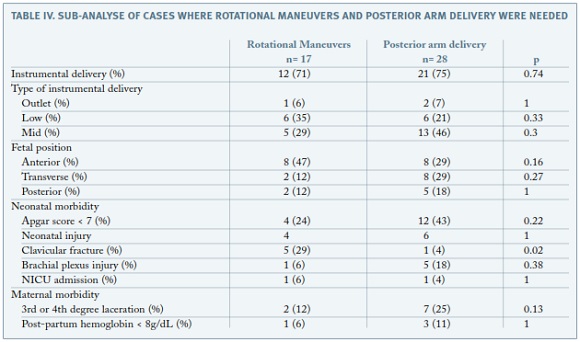
In order to compare rotational maneuvers with delivery of posterior arm, we performed a sub-analysis: no statistical differences in the proportion of instrumental delivery, type of operative vaginal delivery and fetal head position were seen (Table IV). Regarding to neonatal morbidity there was a higher rate of clavicular fracture in the group of rotational maneuvers (28% versus 4%, p= 0.05). Maternal morbidity was not different between groups.
Discussion
After the diagnosis of shoulder dystocia, the operator has up to five minutes to deliver a previously well oxygenated fetus before an increased risk of asphyxia injury occurs6,7. In order to release the impacted shoulder, several maneuvers have been used, but there are no randomized trials for comparing their effectiveness. No single maneuver is clearly more effective or safer for the fetus and the initial choice and order of progression will depend on the operator experience1,3,4.
The incidence of SD ranges from 0.2% to 3.0% of all vaginal deliveries1,2. This wide range may be a consequence of the subjectivity of the definition. We found an incidence of 3.3% among our population. It is possible that this higher rate is due to the fact that this was a prospective study and, consequently, obligation for precise documentation of the cases was often stressed during the study period.
We found that almost 70% of SD cases were solved with McRoberts’ and supra-pubic pressure, and the need of rotational maneuvers and posterior arm delivery was associated with a longer second stage of labor and transverse fetal head position. In a retrospective review of consecutive cases of SD done by Gherman, the McRoberts’ maneuver alone was found to have a success rate of 42% and 54.2% when combined with supra-pubic pressure and/or proctoepisiotomy8. McFarland found that 39.5% of SD cases were solved with McRoberts’ maneuver only, and the subsequent addition of supra-pubic pressure had a success rate of 58%9. In our study the higher incidence of SD solved with the use of McRoberts and supra-pubic pressure may have two explanations. Firstly, the fact that this was a prospective study might have lead to more precise diagnosis of SD and a fast attempt of resolution with the simpler maneuver, and, secondly, most obstetricians in our department employ the McRoberts’ maneuver as their initial step for the disimpaction of the shoulder.
We could not find any association between maternal characteristics, rate of instrumental delivery, type of instrumental delivery and fetal birth weight, and the need of additional maneuvers after McRoberts’ and supra-pubic pressure. The same finding was observed in the work of Leung, when he analyzed the effectiveness and safety of individual maneuvers, according to the sequence of the maneuvers used10. However, we found that cases requiring more extensive maneuvers were associated with longer second stages of labor (45 (25-60) minutes versus 60 (48-100) minutes) and the transverse fetal head position. Gherman showed that when the McRoberts’ maneuver was compared with the need of further actions, the first group of patients had a shorter second stage of labor (46.4±44.2 minutes versus 84.7±75.4 minutes, p< 0.00001) 8. Nevertheless, 15 minutes of difference does not seem clinically relevant and, moreover, parity and spinal anesthesia have not been taken into account for the statistical analysis.
Interestingly, when the instruments where applied in a transverse fetal head position, there was a higher need for rotational maneuvers or delivery of posterior arm for solving a SD. However, we believe this finding needs to be further evaluated in prospective studies where the fetal head position is recorded regardless of the type of delivery.
There are only a handful of studies that evaluated the different types of maneuvers to overcome shoulder dystocia and the rates of associated fetal injury. We found that when more extensive maneuvers were needed, newborns had lower Apgar score at the first minute and an higher rate of neonatal injuries, specifically clavicular fracture. The few studies reporting the neonatal morbidity according to the type of maneuvers used to resolve SD are retrospective and the data is not completely clear. Nocon studied the neonatal injury rate according to the final maneuver used to solve the SD, and the incidences for the McRoberts’ maneuver, suprapubic pressure, rotation and posterior arm delivery were 14.9, 20.0, 14.3 and 37.9%, respectively11. In the same way, McFarland found higher neonatal injuries when three or more maneuvers were needed9. On the other hand, Leung reported no increase in either brachial plexus injury or clavicular fracture when additional maneuvers were used after McRoberts’ technique10. In our series, when we compared the McRoberts’ and supra-pubic pressure versus rotational maneuvers and posterior arm delivery, we found a higher percentage of neonates with clavicular fracture in the last group. There were no cases of humeral fracture. As seen in previous studies, when the McRoberts’ and supra-pubic pressure were initially unsuccessful, the addition of other maneuvers did not increase the incidence of brachial plexus injury (4% versus 11%). Although McRoberts’ maneuver will slightly modify the angle to maternal pelvis, lateral traction is still needed to dislodge the fetal anterior shoulder. At this step, brachial lesion might occur. It must be emphasized that, due to this fact, traction should be done carefully and since in our institution the majority of the deliveries are accomplished by doctors or midwifes trained in the resolution of SD, that may explain why in our series the proportion of cases with brachial plexus injury was lower than the one reported in literature, even having a higher rate of cases solved with McRoberts’ and supra-pubic pressure.
Further analysis of our data showed a higher proportion of clavicular fracture when rotational methods were used (29% versus 3%) and this finding is consistent with Leung’s findings10. The force applied either on the anterior surface of the posterior shoulder - Woods’ corkscrew maneuver - or on the posterior surface of the most accessible part of the fetal shoulder - Rubin’s maneuver - causes minimal stress on the brachial plexus or humerus. However, because the clavicles are part of the shoulder girdle, they will be under stress during rotation in both directions, thus increasing the risk of fracture.
Regarding maternal complications, although rare, it is well established that cases of excessive force or prolonged placement of the patient’s legs in a hyperflexed position have led to symphyseal separation, sacroiliac joint dislocation, and transient lateral femoral cutaneous neuropathy13. In our series, none of these complications have occurred. Understandably, rotational maneuvers and delivery of posterior arm were associated with higher maternal morbidity - 3rd or 4th degree laceration. Similar findings had previously been reported by McFarland, who found that the incidence of maternal fourth-degree laceration or episiotomy increased as the number of maneuvers increased.9
Limitations and strengths
This was a prospective study and therefore we were able to include a reasonable number of women and complete outcome data. Moreover, the uniformity in the management of pregnancy complications and shoulder dystocia based on protocols that followed standard guidelines and were adopted by our department is another strength. The new insight that a transverse fetal head position might be associated to the need of rotational maneuver and/or posterior arm delivery is an important achievement. Nonetheless, more prospective studies where the fetal head position is recorded are needed.
As seen in other studies, the use of a subjective definition can overestimate the rate of SD. This is a weakness of virtually all SD studies. The authors point that the fact that head-to-body delivery time haven’t been recorded, as well as the last maneuver used to solve the dystocia are important limitations to study the relationship between the type of maneuver and its morbidities.
Conclusion
Our results indicated that most (70%) cases of shoulder dystocia can be solved by application of McRoberts’ and supra-pubic pressure and this is associated to a small risk of brachial plexus injury and clavicular fracture. Furthermore, if an instrumental delivery is performed, when the instruments are applied in a transverse fetal head position, there is a higher need for rotational maneuvers or delivery of posterior arm for solving SD.
REFERENCES
1. ACOG Committee on Practice Bulletins-Gynecology, The American College of Obstetrician and Gynecologists. ACOG practice bulletin clinical management guidelines for obstetrician-gynecologists. Number 40, November 2002. Obstet Gynecol 2002; 100:1045. [ Links ]
2. Hoffman M, Bailit J, Branch D, Burkman R, Van Veldhusien P, Lu L, et al. A comparison of obstetric maneuvers for the acute management of shoulder dystocia. Obstet Gynecol 2011; 117:1272. [ Links ]
3. Leung TY, Chung TK. Severe chronic morbidity of childbirth. Best Pract Clin Res Obstet Gynaecol 2009; 23:401-423. [ Links ]
4. Royal College of Obstetricians and Gynecologists. Shoulder Dystocia. Green-Top Guideline No. 42. London: RCOG, 2005. [ Links ]
5. Gherman R, Chauhan S, Ouzounian J, Lerner H, Gonik B, Goodwin T. Shoulder dystocia: the unpreventable obstetric emergency with empiric management guidelines. Am J Obstet Gynecol. 2006; 195:657-672. [ Links ]
6. Leung T, Stuart O, Sahota D, Suen S, Lau T, Lao T. Head-to-body delivery interval and risk of fetal acidosis and hypoxic ischaemic encephalopathy in shoulder dystocia: a retrospective review. BJOG 2011; 118:474. [ Links ]
7. Lerner H, Durlacher K, Smith S, Hamilton E. Relationship between head-to-body delivery interval in shoulder dystocia and neonatal depression. Obstet Gynecol 2011; 118:318. [ Links ]
8. Gherman R, Goodwin T, Souter I, Neumann K, Ouzoinian, Paul R. The McRoberts’ maneuver for the alleviation of shoulder dystocia: how successful is it? Am J Obstet Gynecol 1997; 176:656-661. [ Links ]
9. McFarland M, Langer O, Piper J, Berkus M. Perinatal out- come and the type and number of maneuvers in shoulder dystocia. Internat J Gynecol Obstet 1996; 55:219-224. [ Links ]
10. Leung T, Stuart O, Suen S, Sahota D, Lau T, Lao T. Comparison of perinatal outcomes of shoulder dystocia alleviated by different type and sequence of manoeuvres: a retrospective review. BJOG 2011; 118:985-990. [ Links ]
11. Nocon J, McKenzie D, Thomas L, Hansell R. Shoulder dystocia: an analysis of risks and obstetric maneuvers. Am J Obstet Gynecol 1993; 168:1732-1739. [ Links ]
12. Gherman R. Shoulder dystocia: an evidence-based evaluation of the obstetric nightmare. Clin Obstet Gynecol. 2002; 45:345-362. [ Links ]
13. Heath T, Gherman R. Symphyseal separation, sacroiliac joint dislocation and transient lateral femoral cutaneous neuropathy associated with McRoberts’ maneuver. A case report. J Reprod Med. 1999; 44:902. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Maria Carvalho Afonso,
Hospital de Santa Maria
Lisboa, Portugal
E-mail: mariafonso@yahoo.com
Recebido em: 26/01/2016
Aceite para publicação: 02/08/2016