Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Obstétrica e Ginecológica Portuguesa
versión impresa ISSN 1646-5830
Acta Obstet Ginecol Port vol.11 no.4 Coimbra oct. 2017
IMAGE OF THE TRIMESTER/IMAGEM DO TRIMESTRE
An adnexal mass at the cesarean section
Uma massa anexial durante uma cesariana
Ana Edral*, Fernanda Vilela*, Ângela Ferreira**
Centro Hospitalar Universitário do Algarve
*Interna de Formação Específica em Ginecologia e Obstetrícia, Centro Hospitalar Universitário do Algarve - Faro
**Assistente Hospitalar de Ginecologia e Obstretrícia, Centro Hospitalar Universitário do Algarve - Faro
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Splenosis refers to the presence of ectopic splenic tissue through autotransplantation following traumatic rupture of the spleen or splenectomy. We report the case of a previously asymptomatic 31-year-old pregnant woman who had undergone splenectomy at 12 years of age after traumatic splenic rupture. She was submitted to cesarean section, during which multiple bluish-red nodules were found on the greater omentum and a bigger one adjacent to the right ovary as an incidental finding. Histopathology revealed the presence of supernumerary splenic tissue. We aim to raise awareness to this diagnosis since this benign finding can mimic several gynecological diseases.
Keywords: Splenosis; Pelvic tumour.
We report the case of an asymptomatic adnexal mass diagnosed during a cesarean section.
A 31-year-old pregnant caucasian female (gravid 3, parous 0), 0Rh+, was admitted to the obstetrics department at 39 weeks and 2 days with premature rupture of membranes five days before. She had undergone splenectomy due to traumatic rupture during a car accident at 12 years of age. Familial antecedents were unremarkable.
At admission, physical examination, vital signs and obstetric ultrasound were within the normal range, except for positive placental alpha microglobulin-1 test (AmniSure® test - Quiagen Company, USA). She was hospitalized and labor induction with misoprostol and oxytocin was started. Simultaneously, ampicillin antibiotic prophylaxis was initiated. On the second day she went into labor. Cesarean section was performed after 8 hours of labor for probable fetopelvic disproportion and fetal tachycardia. A male newborn weighing 3310g was delivered with an Apgar Score of 4/9 at 1' and 5', respectively.
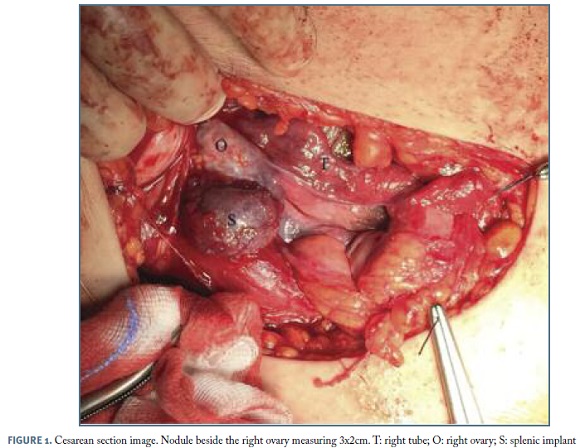
At the cesarean section we observed multiple elastic bluish-red nodules on the greater omentum measuring ≤1cm each and a bigger hemorrhagic one adjacent to the right ovary (Figure 1). The remaining abdominal cavity was apparently normal.
An excisional biopsy of the epiplon was performed and sent for histopathological examination, which revealed “two supernumerary spleens”. Post-surgery evolution was uneventful.
Splenosis refers to the presence of heterotopic splenic tissue, resulting from spillage of splenic cells after traumatic rupture or splenectomy1,2.
The real prevalence of splenosis is unknown. Most patients are asymptomatic and the diagnosis is frequently incidental. Since the first disease report, in 1939, few cases have been described in the literature. Estimates of its prevalence vary widely: 26-65% following trauma and 16-20% following elective splenectomy2.
Splenic implants can be found anywhere in the abdomen: most often on the upper left quadrant2, on serosal surfaces of the bowel, peritoneum, mesentery and diaphragm. Rarer locations include female genital organs, chest and breast tissue3.
Gynecological cases are a minority and pose a diagnostic challenge since these implants may resemble gynecological neoplasms, metastasis, endometriosis, lymphoma or pelvic hemangioma4,5.
Usually, patients are asymptomatic, however, some may present with abdominal pain or with a clinical picture of an abdominal mass with intestinal obstruction, hydronephrosis or intra-abdominal hemorrhage3,5.
It is important to be aware of this diagnosis, since it may lead to unnecessary surgical intervention. The alleged diagnosis can be made when the patient underwent prior splenectomy or suffered severe abdominal trauma5. A pelvic ultrasound may reveal a well-defined mass, with homogeneously hypoechoid echotexture and blood flow with normal resistance indexes4,5. The CT-scan, may reveal the number, shape and size of masses. Radioisotope scanning using Tc99 labeled platelets or heat-denatured red cells may confirm the diagnosis2. On peripheral blood smear, there should be no Howell-Jolly bodies or just a low percentage of pitted red blood cells2.
If the patient is asymptomatic, no further workup or invasive measures are required.
Splenic ectopic tissue should be left untouched in asymptomatic patients, since it may be beneficial as it partially replaces the function of absent spleen5.
REFERENCES
1. Zitzer P, Pansky M, Maymon R, Langer R, Bukovsky I, Golan A. Pelvic splenosis mimicking endometriosis, causing low abdominal mass and pain. Hum Reprod. 1998 Jun;13(6):1683-1685. [ Links ]
2. Schrier SL. Approach to the adult patient with splenomegaly and other splenic disorders. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (Accessed on November 15, 2016. [ Links ])
3. Metindir J, Mersin HH, Bulut MZ. Pelvic splenosis mimicking ovarian metastasis of breast carcinoma: a case report. J Turk Ger Gynecol Assoc. 2011;12(2):130-132. [ Links ]
4. Levy AD, Shaw JC, Sobin LH. Secondary tumors and tumorlike lesions of the peritoneal cavity: imaging features with pathologic correlation. Radiographics. 2009 Mar-Apr;29(2):347-373.
5. Zvi V, Moti P, Mendlovic S, Arie H, Maymon R. Pelvic splenosis - a gynaecological challenge. Reprod Biomed Online. 2009 Mar;18(3):421-423. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Ana Edral
E-mail: edral.ana@gmail.com
Recebido em: 01/12/2016
Aceite para publicação: 22/08/2017