Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Obstétrica e Ginecológica Portuguesa
versão impressa ISSN 1646-5830
Acta Obstet Ginecol Port vol.13 no.4 Coimbra dez. 2019
REVIEW ARTICLE/ARTIGO DE REVISÃO
Ptyalism Gravidarum
Ptyalism Gravidarum
Manuel Gonçalves-Henriques1, Pedro Brandão2
Hospital Professor Doutor Fernando Fonseca Centro Hospitalar Tâmega e Sousa
1 MD, Resident in Obstetrics and Gynaecology, Department of Obstetrics and Gynaecology - Hospital Prof. Doutor Fernando Fonseca.
2 MD; MSc, EFOG, Attending in Obstetrics and Gynaecology, Department of Obstetrics and Gynaecology - Hospital da Senhora da Oliveira - Guimarães; Faculty of Medicine, University of Porto.
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
This is a systematic review of ptyalism gravidarum. Very few data concerning ptyalism gravidarum has been published so far, which culminates in health care providers’ lack of knowledge about this disorder and its management. Ptyalism gravidarum is a rare disorder associated with pregnancy, characterized by an excessive production of saliva beginning during the first trimester and persisting until delivery or some weeks after. Its exact pathophysiology remains unknown. Most of the few data published about the subject consider ptyalism gravidarum not to pose any specific risks to pregnancy. It’s a self-limited condition and there is no treatment for the disorder.
Keywords: Pregnancy complication; Sialorrhea.
Background
Ptyalism gravidarum (PG) is a rare condition affecting pregnancies, characterized by an excessive production of saliva. Although benign and self-limited, it can cause significant discomfort during pregnancy. Very few data about PG has been published so far, which ultimately culminates in health care providers’ lack of knowledge about this disorder and its management.
Objective and methods
The aim of this work is to review all published data about ptyalism gravidarum.
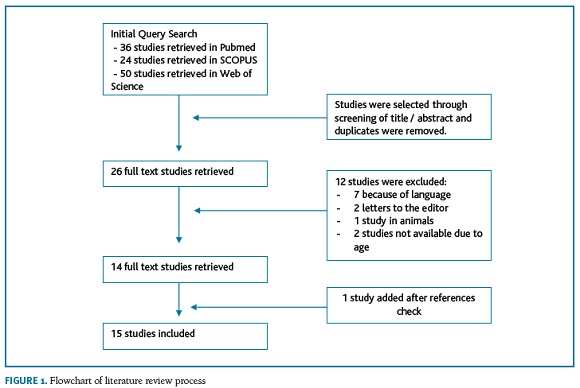
A review of all articles listed in Pubmed, SCOPUS and Web of Science was performed in April 2019 using the query: “ptyalism gravidarum OR ((sialorrhea OR ptyalism OR hypersialorrhea) AND pregnancy)”. Original works, reviews, case reports and cases series concerning PG in humans were included. Articles written in languages other than English as well as articles not available online due to their age were excluded. The articles’ titles of the references of the included studies were checked to be included if related to PG.
With the initial search, a total of 110 results were obtained (36 in Pubmed, 24 in SCOPUS and 50 in Web of Science). After analysing all the articles’ titles, removing duplicates, applying the inclusion and exclusion criteria and checking references, 15 studies about sialorrhea in pregnancy were obtained. (Figura 1)
All articles were fully read and all data concerning ptyalism gravidarum was summarized in this review.
Review
Definition and Epidemiology and Risk Factors
Ptyalism gravidarum is a rare condition affecting 0.05 to 0.3% of all pregnancies1. It is characterized by excessive secretion of saliva. Due to its low frequency, there are no specific criteria to establish the diagnosis. It is commonly associated with nausea and vomiting during the first trimester from mild morning sickness to hyperemesis gravidarum (HG), symptoms of gastroesophageal reflux disease, as well as other eating disorders such as bulimia, anorexia nervosa or PICA Syndrome2-5. Some studies suggest it may be more frequent in women with family history of the disorder and in psycotic patients. Multiple pregnancies and fetal gender have been pointed as possible risk factors but the evidence is contradictory6,7. There seems to be no association with maternal age7.
Clinical Presentation
Ptyalism gravidarum is described as excessive salivation, up to 2L per day (versus an average of less than 1L/day on a healthy non pregnant adult). It begins during the first trimester of pregnancy, as early as the 4th week and it may improve with time or persist until the end of pregnancy or some weeks postpartum. Patients may struggle to swallow the high amount of saliva requiring spitting cups or paper tissues to dispose redundant saliva6. Ultimately accumulation of saliva may cause speech impairment8.
There may be some associated symptoms such as nausea, vomiting, anorexia, bad taste, ice craving and intolerance to diverse smells or tastes. Parotid and submandibular glands may be swollen due to enlargement of the gland and local vasodilatation9. Some patients may end up with sleep deprivation and emotional distress. Although PG symptoms usually improve during sleep time, some patients report being awaken by the excessive salivation. It’s not clear whether this entity may have any impact in weight gain during pregnancy10-12.
Pathophysiology
The pathophisiology of ptyalism gravidarum is unknown. Some authors consider it may have a psychological origin, others believe it has an organic explanation. The improvement of symptoms during sleep is more indicative of a psychological aetiology. On the other hand, its higher prevalence during early pregnancy suggests a hormonal effect7.
The secretion of saliva is regulated by the Autonomous Nervous System (through the glossopharyngeal and facial nerves), highly stimulated by the parasympathetic nerves which increase the amount of saliva produced9.
As for most of the changes related to pregnancy, high hCG, progesterone and oestrogens levels may play an important role4,8. There is some evidence that pregnancy related salivation may be mediated by Substance P like peptides segregated by the hypothalamus and the K1R agonist activity of the Placental Endokin B (EKB)13. Also, the vomiting centre and the salivary control area are anatomically close14. All these features support a common aetiology to nausea and sialorrhea during pregnancy.
Diagnosis
The diagnosis of this disorder is based on its clinical presentation. Due to the fact that most of the times other conditions may also be present, when PG is suspected, physicians must always rule out simple nausea related to pregnancy, hyperemesis gravidarum, PICA and eventually more serious eating disorders such as anorexia nervosa or bulimia2,10. No complementary tests are required. Except in the event of concomitant HG, no abnormalities are expected in biochemical or electrolyte test. Salivary gland ultrasound may reveal enlargement of these glands10.
Management
Ptyalism gravidarum is a self-limited disorder associated with pregnancy. It may improve or persist during pregnancy. Usually it resolves during the second trimester or at delivery, but in rare cases it may persist as long as 1 month postpartum7. Nevertheless, its symptoms may be quite limiting and thus pregnant women may require symptomatic treatment. It is important that every health care provider is aware of PG and tries to understand the severity of the disorder as well as its impact on patients quality of life and their ability to handle its symptoms.
There is little consensus on how to manage patients with established PG. Many therapies have been attempted to reduce symptoms, but their efficacy is questionable and highly variable.
Some conservative measures include consumption of hard candies, chewing gums, dry toasted bread or crackers, frequent drinks of still unflavoured water. Lemon drops or oral lozenges or may be used to avoid bad taste. Most of the case series report few patients submitted to hypnosis, acupuncture or other alternative treatments such as Chiropractic therapy (also known as manual therapy) resulting in no effect to complete resolution of symptoms15,16.
Some herbal agents have also been used, including alpinia oxyphylla, a traditional Chinese medication used for helping digestion, antidiuresis and salivation restraint. Not only the efficacy of these treatments is inconclusive but also its safety in pregnancy is still to be determined6.
Medication used to treat pregnancy related sickness has been widely used to treat this condition, such as the association of docylamine and pyridoxine and metoclopramide. Even though their role in improving PG symptoms is not clear, it may relief nausea which is quite commonly associated with this disorder and considered safe during pregnancy. Other pharmacologic agents have been used to reduce saliva production and/or relief symptoms such as barbiturates, anticholinergics, belladonna alkaloid, phenothiazine or scopolamine2,9. Unfortunately the evidence of the efficacy of these treatments is sparse and most patients keep their symptoms until complete spontaneous resolution of the disorder 6,17.
Outcomes, prognosis and recurrence
Published data about obstetric outcomes of pregnancies complicated by PG is poor and somehow contradictory. Some authors found an increased incidence of low birth weight, probably related to low maternal weight gain and prematurity, but others have found no association with worse fetal, neonatal or maternal outcomes1,7,9.
PG appears to be more frequent in previously affected patients, so women must be warned that they have a higher probability of suffering from this condition again in a future pregnancy7.
Conclusion
Ptyalism gravidarum is a rare disorder associated with pregnancy that usually begins during the first trimester and persists until delivery or post-partum. Most of the few data published about the subject are case reports or case series and they consider PG not to pose any specific risks to pregnancy other than its bothersome symptoms. Its exact pathophysiology remains unknown. It’s a self-limited condition and there is no proven therapy to effectively relief symptoms or treat the disorder.
REFERENCES
1. Suzuki S, Fuse Y. Clinical significance of ptyalism gravidarum. Arch Gynecol Obstet 2013;287:629-631. [ Links ]
2. Cardwell MS. Eating Disorders During Pregnancy. Obstet Gynecol Surv 2013;68:312-323. [ Links ]
3. Godsey RK, Newman RB. Hyperemesis gravidarum. A comparison of single and multiple admissions. J Reprod Med 1991;36:287-90. [ Links ]
4. Diko ML, Siewe épse Diko CN. Physico-chemistry of geophagic soils ingested to relief nausea and vomiting during pregnancy. Afr J Tradit Complement Altern Med 2014;11:21-24. [ Links ]
5. Lacasse A, Rey E, Ferreira E, Morin C, Bérard A. Determinants of early medical management of nausea and vomiting of pregnancy. Birth 2009;36:70-77. [ Links ]
6. Suzuki S, Igarashi M, Yamashita E, Satomi M. Ptyalism gravidarum. N Am J Med Sci 2009;1:303-304. [ Links ]
7. Bronshtein M, Gover A, Beloosesky R, Dabaja H, Ginsberg Y, Weiner Z, Khatib N. Characteristics and Outcomes of Ptyalism Gravidarum. Isr Med Assoc J 2018;20:573-575. [ Links ]
8. Thaxter Nesbeth KA, Samuels LA, Nicholson Daley C, Gossell-Williams M, Nesbeth DA. Ptyalism in pregnancy - A review of epidemiology and practices. Eur J Obstet Gynecol Reprod Biol 2016;198:47-49. [ Links ]
9. Freeman JJ, Altieri RH, Baptiste HJ, Kuo T, Crittenden S, Fogarty K, Moultrie M, Coney E, Kanegis K. Evaluation and management of sialorrhea of pregnancy with concomitant hyperemesis. J Natl Med Assoc 1994;86:704-708. [ Links ]
10. Canverenler E, Canverenler S. Ptyalism gravidarum : A case report. 2017;3615:144-146.
11. Shiny Sherlie V, Varghese A. ENT Changes of Pregnancy and Its Management. Indian J Otolaryngol Head Neck Surg 2014; 66:6-9. [ Links ]
12. Hartfield VJ. Ptyalism and Partial Hydatidiform Mole Associated with a Normal Term Male Fetus. Aust New Zeal J Obstet Gynaecol 1983;23:53-56. [ Links ]
13. Lowry P, Woods R. The placenta controls the physiology of pregnancy by increasing the half-life in blood and receptor activity of its secreted peptide hormones. J Mol Endocrinol 2018;60:R23-R30. [ Links ]
14. Mandel L, Tamari K. Sialorrhea and gastroesophageal reflux. J Am Dent Assoc 1995;126:1537-1541. [ Links ]
15. Beevi Z, Low WY, Hassan J. Successful Treatment of Ptyalism Gravidarum With Concomitant Hyperemesis Using Hypnosis. Am J Clin Hypn 2015;58:215-223. [ Links ]
16. Skarica B. Effectiveness of Manual Treatment on Pregnancy Symptoms: Usefulness of Manual Treatment in Treating Pregnancy Symptoms. Med Arch 2018;72:131. [ Links ]
17. Van Dinter MC. Ptyalism in pregnant women. J Obs. Gynecol Neonatal Nurs. 1991:206-209. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Manuel Gonçalves-Henriques
E-Mail: manuelghenriques@gmail.com
Recebido em: 18/06/2019
Aceite para publicação: 13/10/2019