Introduction
In 2019, a new virus of the Coronavirus family arose in the Chinese city of Whuan, infecting millions of people and causing thousands of deaths worldwide - the SARS-CoV2 (Severe Acute Respiratory Syndrome - Coronavirus 2), whose disease is called COVID19 (Coronavirus Disease 2019). The impact of this new virus was such, that the World Health Organization (WHO) declared a global pandemic in March 2020. Similar to other Coronavirus, SARS-CoV2 causes a severe acute respiratory syndrome (SARS) which may ultimately lead to respiratory distress, multiorgan fai lure and death.
SARS-CoV2 has an incubation period that can last as long as 14 days, disseminating through respiratory droplets, which make it highly contagious between humans. The spectrum of its clinical features is wide, ranging from asymptomatic carriers or mild illness to critical disease and death. Older patients and patients with comorbid conditions such as diabetes mellitus, hypertension or other cardiovascular diseases, obesity, respiratory conditions and immunosuppression are at much higher risk of developing severe symptoms 1.
Facing a new infection, some specific concerns regarding pregnancy have been raised. This includes a hypothetical risk of more severe maternal infection and its consequences on fetal wellbeing, pregnancy-related complications, congenital infection or harmful effects of the virus and the impact of antiviral and supporting care drugs. The postpartum period also raised some worries about the risk of mother-child transmission of the virus and subsequent newborn infection. In countries were lockdown measures were imposed to control the virus spread, there was also the concern of a lower availability or accessibility of health care services 2,3.
On one hand, regarding maternal complications, pregnancy, as a state of physiological immunosuppression, may theoretically contribute to a more severe condition. On the other hand, pregnant patients are young, and according to the literature, except for some minor changes, such as mild lymphopenia or thrombocytopenia, the rates of severe infection and other complications seem to be similar to general population4-6. However, one must remember that the hypoxia in cri tically ill pregnant patients may compromise fetal wellbeing and further fetal monitoring may be desirable7,8.
Pertaining to obstetric complications, COVID19 appears to be associated with higher rates of preterm labor. Although COVID19 is not an indication for caesarean section (C-section) and despite the fact that labor management should be similar to non-infected mothers, C-section rates reported to date are significantly higher4,5,9,10. In contrast, there seems to be no impact on miscarriage rates11.
There are some reports of vertical transmission, especially during the third trimester, so the risks to the fetus and the newborn are yet to be clarified12-15. Due to the lack of time since the appearance of the virus, there is still sparse data about the fetal risks of maternal infection, especially in early pregnancy. Despite that, there is no evidence of teratogenesis5.
There is some evidence that maternal breast milk may be contaminated. Nursing and skin-to-skin contact of the newborns with infected mothers may pose a risk of infection to the newborn, which must be weighed against maternal and neonatal benefits of these actions16.
The first case of COVID19 confirmed in Portugal was on the 2nd of March 2020 and a maximum of 1516 new cases was reached on the 10th of April. Since then, the number of daily new cases has fell to reach a plateau of around 200 to 300 new cases a day. At the beginning, the most affected region was Northern Portugal (Norte) and the major urban areas - Porto and Lisboa. In May, the situation slowed down throughout the country, except for the region of the capital city (Lisboa and Vale do Tejo). By the end of May, when this study started, a total of 32500 cases had been identified and 1410 people had died due to COVID19 in Portugal. During the last week of May, the week before this study took place, an average of 268 new ca ses and 13 death had occurred each day 17,18. Few information is available about this infection in this country in the obstetric population, but to date there were no maternal deaths.
Given the sparse information about COVID19 in the obstetric field and the unknown potential risks of an infection during pregnancy, preconception counselling during the pandemic is very challenging.
The aim of this work was to evaluate the Portuguese obstetricians preconception counselling during SARS--CoV2/COVID19 pandemic, their main concerns about pregnancy during this period and their opinion about vaccination when pregnancy is planned.
Methods
A cross-sectional study was preformed, based on an 8-question survey applied to national doctors of obstetrics and gynaecology, both specialists and residents. The survey was written in Portuguese and available online and in paper format (questionnaire in Portuguese as supplementary file). The sampling was performed following the snowball method - the questionnaire was primarily sent electronically via email and social networks, doctors were asked to fulfill the questionnaire once and send it to other colleagues of this specialty. When the paper format was used, people were asked not to answer if they had already answered the electronic version to avoid duplicates. Data was collected between the 31st of May and the 7thof June 2020. At the beginning of every questionnaire, after explaining the purpose of the work and guaranteeing confidentiality, all the inquired were asked to give their consent.
All data were collected, stored and analyzed anonymously.
Statistical analysis was performed using Statistical Package for the Social Science (SPSS®) version 23.0 using chi-square test. Statistical significance was set at p<.05. All the answers were used for analysis. When the area of expertise was taken into account, only specialists were considered.
Questions 1 to 4
The first 4 questions aimed to characterize the sample: gender, professional category, region (according to corresponding regional health administration - Administração Regional de Saúde - ARS) and area of expertise (main area of clinical practice: gynaecology, obs tetrics and reproductive medicine).
Question 5
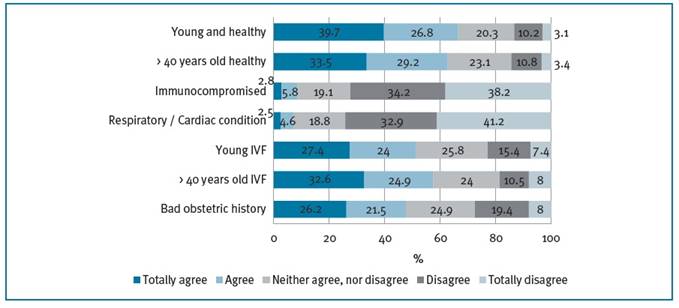
Question 5 was about counselling, in general, for patients who desire to get pregnant (option 1: the patient may get pregnant, there is no contraindication; option 2: recommendation to wait a few months until the si tuation gets stable; option 3: recommendation to wait until a vaccine is available; option 4: recommendation to wait until the end of the pandemic is declared; option 5: either situation 3 or 4).
Question 6
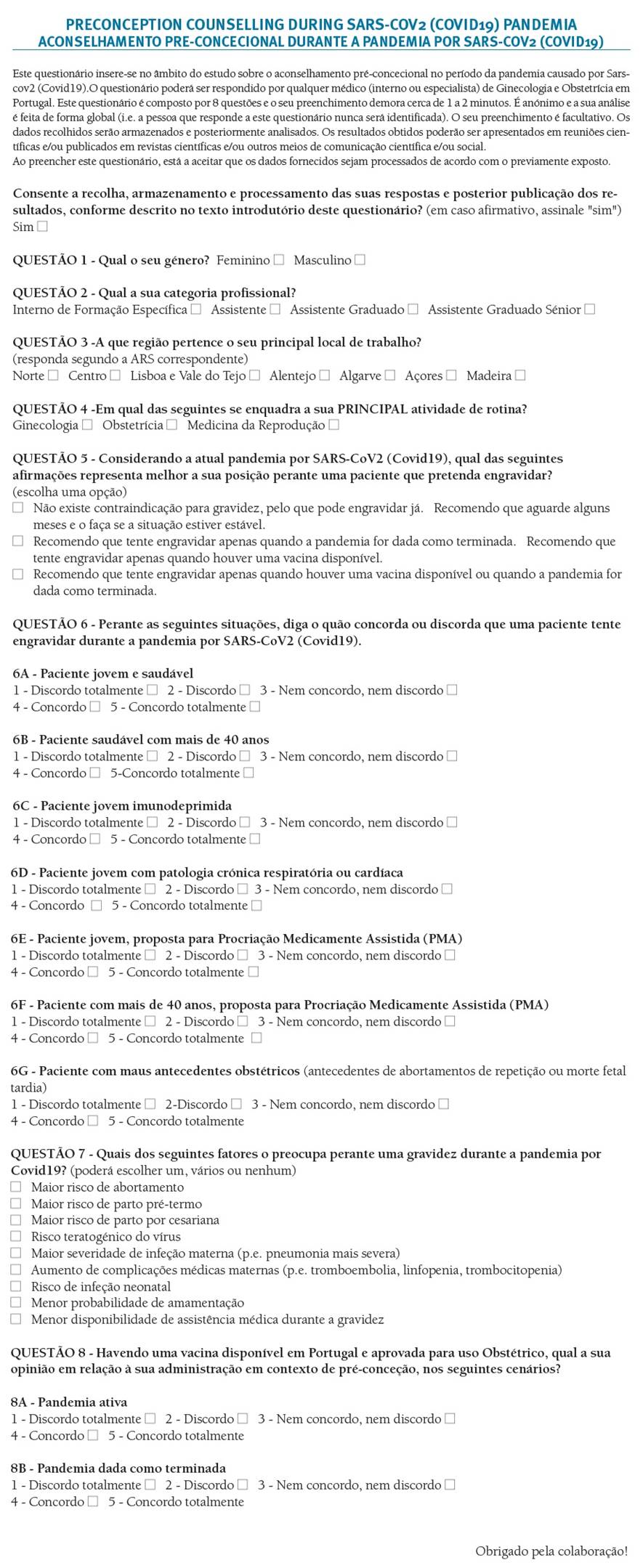
In question 6 respondents were asked to say how much did they agree with planning a pregnancy during the pandemic in 7 specific scenarios: situation A - young and healthy patient; B - healthy patient more than 40 years-old; C - immunocompromised young patient; D - young patient with respiratory or cardiac condition; E - young patient undergoing assisted reprodutive techonology treatments (ART); F - ART patient more than 40 years-old and G - patient with bad obstetric history.
Answers were given in a Likert scale: 1 - totally di sagree; 2 - disagree; 3 - neither disagree, nor agree; 4 - agree; 5 - totally agree. For reporting the results, 2 news categories were considered: “Agree” (answers “agree” and “totally agree”) and “Disagree” (“disagree” and “totally disagree”).
Question 7
Respondents were asked which of the following (if any) would be a concern in a pregnancy during COVID19 pandemic: A- Higher risk of miscarriage; B - Higher risk of preterm labor; C - Higher risk of C-section; D - Risk of teratogenesis; E - Risk of more severe maternal infection (i.e. more severe maternal pneumonia); F - Higher risk of maternal medical complications (embolism, thrombocytopenia, lymphopenia); G - Risk of neonatal infection; H - Lower probability of nursing and I - Risk of lower availability of medical care services.
Results
A total of 325 inquiries answered the survey. A large majority of the inquired were females (82.5%) and more than half were specialists (63.1%). The predomi nant region of the respondents was Norte (50.8%), followed by Lisboa e Vale do Tejo (24.9%) and Centro (12%). Within specialists, most of them had either
obstetrics or gynecology as the main field of clinical practice. Some of them reported more than one area of expertise (Table I).
The only differences found between groups were a higher percentage of male doctors in Madeira region (34.6%, p=.03) and within specialists (22%, p=.006) and the distribution of the specialists reporting acti vity in reproductive medicine, who were only from 4 regions (Norte, Centro, Lisboa e Vale do Tejo and Madeira).
General Counselling
When asked about the general counselling facing a patient who wants to get pregnant during COVID19 pandemic (question 5), more than half of the respondents considered there were no contraindications for pregnancy (53.2%), while some others would recommend to wait a few months until the situation got stable (39.7%). Only a minority considered it would be important to wait for a vaccine or the end of the pandemic (Figure 1).
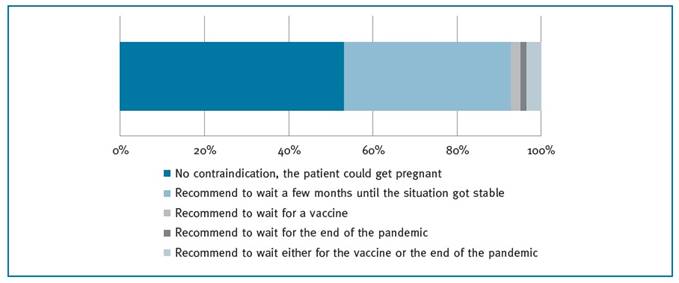
FIGURE 1 Answers to question 5 - What would be your general counselling to a patient desiring to get pregnant during the pandemic?
A lower percentage of experts in obstetrics would approve an immediate pregnancy (48.4%, p=.034). In contrast, a higher percentage of doctors in the reproductive medicine field would be in favor of pregnancy (78.6%, p=.013). No other significant differences were found.
Specific situations
Most of the respondents were in favor of pregnancy during the pandemic in a young and healthy patient (66.5%). A similar result was obtained for healthy patients more than 40 years old (62.8 %, p=.07). On the other hand, for all the other situations, the number of doctors in favor of pregnancy was significantly lower (p<.0001); when more than 40 years old ART patient (57.5%), young ART patient (51.4%) and patient with bad obstetric history (47.7%) were considered, the respondents agreed with planning pregnancy in 57.5%, 51.4% and 47.7% respectively. Concerning young patients with respiratory or cardiac conditions and immunocompromised patients, most of the inquired doctors disagreed with planning a pregnancy during this period (74.2% and 72.3% respectively) (Figure 2).
A lower percentage of doctors from Algarve and Lisboa e Vale do Tejo disagreed with planning a pregnancy in an immunocompromised patient (27%, p=.033 and 63%, p=.002 respectively). On the other hand, a much higher percentage was found in Centro (89.7%, p=.008). Also, doctors working in reproductive medicine were more prone to recommend a pregnancy in ART patients (82.1%, p=.002 were in favor of recommending ART to a young patient during the pandemic and 89.3%, p=.001 in case of a patient more than 40 years old). No other statistically significant differences were found.
Main concerns of a pregnancy during COVID19 pandemic
The most reported concerns regarding pregnancy during COVID19 pandemic were those related to maternal health - the risk of a more severe maternal infection (50.2%) and other maternal complications such as embolism, thrombocytopenia or lymphopenia (47.%). The respondents were showed to be also worried about the risk of preterm labor (41.2%) and the possibility of less access to medical care (39.1%). Roughly one fourth of the respondents reported the direct risks to the embryo, fetus and newborn as a major concern, such as the risk of teratogenesis (24%), miscarriage (22.8%) and infection of the newborn (21.4%). Both higher rates of C-section and lower rates of nursing were only reported by a minority (13.2% and 12.3% respectively) (Figure 3).
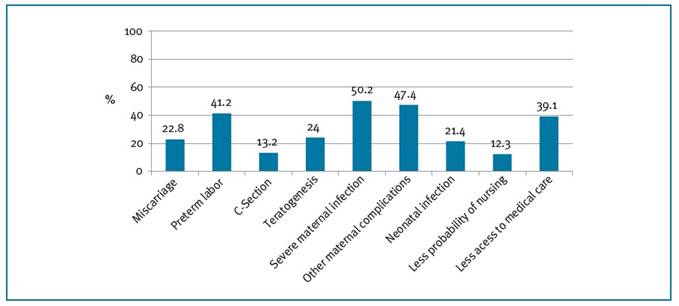
FIGURE 3 Answers to question 7 - Which of these factors do you consider a concern for a pregnancy during the Covid19 pandemic?
Compared to specialists, residents reported more concerns, including the risk of miscarriage (31.7% vs. 17.6%, p=.004), preterm labor (51.7% vs. 35.1%, p=.005), a higher probability of having a cesarean section (20% vs. 9.3%, p=.01), maternal complications (56.7% vs. 42%, p=.011), neonatal infection (28.3% vs. 17.6%, p=.026) and less access to medical care (49.2% vs. 32.2%, p=.005). Interestingly, within specialists, doctors dedicated to obstetrics were less likely to be worried about the risk of teratogenesis (16.8% vs. 29.2%, p=.047).
Preconception vaccination
In the presence of a vaccine against the SARS-CoV2 approved for obstetric use, most of the doctors would be in favor of its administration during the preconception period, both during the pandemic and after its end (93.3% and 76.6% respectively). The majority of them would highly recommend it (74.5% and 52.9% respectively) (Figure 4). Besides the fact the majority of residents and doctors from Algarve were in favor of vaccine administration, they were less likely to re commend it during the pandemic compared to other groups (89.2%, p=.038 and 72.7%, p=.032 respectively).
Discussion
Facing a new virus, especially one declared as a glo bal pandemic after causing thousands of deaths worldwide, concerns have been raised respecting its potential harmful effect to a pregnant woman and her fetus. The still poorly understood obstetric implications of COVID19 made preconception counselling a conside rable challenge during the pandemic.
The majority of the Portuguese obstetricians and residents considered there would be no contraindications for a pregnancy and so they would not oppose to a patient planning pregnancy during the pandemic. However, some of them would rather wait a few months. Interestingly, only a few of them considered pregnancy should only be planned either after the end of the pandemic or after vaccination. These observations meet the recommendations of major obstetric societies, which as a general rule, do not recommend avoiding pregnancy, despite the sparse data about COVID19 and pregnancy 19,20.
As expected, young and healthy patients were the ones obstetricians would more likely approve pregnancy planning during the pandemic. On the other hand, most of the respondents would not recommend pregnancy in immunocompromised patients or patients with respiratory or cardiac conditions. All of these conditions are well known risk factors of a more severe infection.
In respect to ART, most of the respondents, in particular those working in reproductive medicine, were in favor of approving these techniques during this period, especially for older patients. In these patients, the potential risks of a pregnancy during this period must be weighed against the progressively decreasing ovarian reserve and consequent lower rates of success. As for natural conception, international societies of reproductive medicine do not recommend suspending or postponing treatments 21,22.
The main concerns related to pregnancy during the pandemic were those concerning maternal health. Pregnancy, as a state of immunosuppression, may lead to a more severe infection, which may also ultimately be harmful for the fetus. Also, some medical complications have been reported so far, including a higher risk of embolism, thrombocytopenia and lymphopenia4-6.
In regard to labor and delivery, preterm labor was also highly pointed as a concern, which meets current evidence that shows a higher risk of preterm labor in infected patients. C-section rates also seem to be higher, however, according to our study, the majority of the Portuguese obstetricians and residents seemed not to be worried with the effect of COVID19 on the rates of C-section5,11.
Although information is sparse, the rates of miscarriage don’t seem to be higher but the possibility of congenital infection must not be ruled out. More information about the infection during early pregnancy and mid-trimester is needed to ensure its harmlessness12-15. Our results show that both miscarriage and teratogenesis were not a major concern for the majority of the respondents, almost 80% did not point these features.
It is interesting to notice that when this study took place, some weeks after the end of the lockdown and despite the lifting of restrictive measures, almost 40% of the Portuguese obstetricians and residents were still afraid of a possible lack of prenatal medical care.
If a vaccine was available and approved for obstetric use, the vast majority of the respondents would reco mmend it to a woman planning to get pregnant soon, especially if the pandemic was still active.
One of the main limitations of this study was its cross-sectional nature, in particular when addressing the specific situations. It would be interesting to compare the answers of each scenario to the results obtai ned before the pandemic.
The questionnaire and sampling methods had also their own limitations. The questionnaire lacked validation and the snowball method of sampling may have limited the access to some physicians. Furthermore, even though some measures were taken in order to avoid duplicated answers, this could not be ensured.
It’s important to notice that a part of preconception counseling in Portugal is performed by family doctors (general physicians) so the results of this study may not totally reflect the Portuguese reality. It’s also important to notice that this study was undertaken during a plateau phase of the pandemic and so it may not reflect the recommendations during its peak, when the knowledge about the infection was even more limited. Also, it may be stimulating to perform a similar study when there is more knowledge about the course of the disease during pregnancy, its work up and management, in order to compare results.
In a new future it would be interesting to broaden this study to other countries, to understand if local differences in the severity of the pandemic may have influence in pre-conception counselling.
Conclusion
Half of the Portuguese obstetricians and residents in this study would be in favor of planning pregnancy during the COVID19 pandemic. Nevertheless, a big part of them would rather recommend waiting a few months. There were more answers in favor of pregnancy in young and healthy women, and most of them would also approve ART during this period. On the other hand, most of them would not encourage pregnancy in case of maternal immunosuppression, respiratory or cardiac condition.
In general, the main concerns about pregnancy during the COVID19 pandemic were the higher risk of preterm labor, risks related to maternal health and lower availability of medical care services.
If approved for obstetric use, the vast majority of the Portuguese obstetricians in this study would be in favor of vaccinating women during the preconception period, both during and after the pandemic.