Introduction
The primary breast lymphoma is rare, corresponding to only 0,04% to 0,5% of breast cancers. (1), (2 It represents <1% of all non-Hodgking lymphomas and about 2% of extranodals. (3
It has a bimodal distribuition, with incidence peaks in the fourth and seventh decades of life2. The main clinical presentation is the appearance of a painless breast node, which is clinically palpable or not, with or without lymphadenopathy in the ipsilateral axillary region. (1), (4
It is primordial that systemic lymphoma is excluded at the time of diagnosis considering the frequency of breast lymphoma’s secundary involvement, which represents 1% to 5% of all malignant breast tumors. (1), (2), (4 In primary breast lymphoma, the ipsilateral axillary region is the only one that can have tumour cells, besides the breast. (1), (2), (4
The aim of this study is to report two clinical case reports, raising the scientific community’s awareness to a rare pathology which main differential diagnosis is breast carcinoma. Patients’ informed consent for publication was obtained.
Case Report 1
51-year-old female, two pregnancies and two natural births, premenopausal, without previous breast implants, sent to a Senology appointment for palpable left axillary lymphadenopathy with approximately 20 mm, without further symptoms. Breasts appeared clinically and imagiologically without alterations. Ultrasound image showed a 3-cm heterogeneous hypoechoic mass with irregular margins located deep in the left axillary space. Additionally, two suspicious lymph nodes were observed in close proximity. An ultrasound-guided microbiopsy and an excisional biopsy were performed to the lymph nodes and both resulted in reactive lymphadenitis. Two months later, the patient went to the emergency department for left breast oedema and erythema and ipsilateral burning axillary pain. She presented inflammatory signs in the left breast without other alterations and was discharged home with Flucloxacillin and Ibuprofen for mastitis. One week after, her complains and breast inflammatory signs get worse and the antibiotic treatment was changed for ciprofloxacin. Two weeks later, although the inflammatory signs were better, the patient developed fever and a tumor-like mass in the left breast’s upper outer quadrant. The blood tests revealed 17900 leuc/μL with 87% neutrophils, CRP 16,12 mg/dL, slightly normocytic and normocromic anaemia (Hb 11,5 g/dL), prothrombin time slightly elevated (14 seconds) and hyperfibrinogenemia (8,2 g/L). It was performed a surgical exploration due to suspicion of mammary abcess, which resulted in the discovery of a 60 mm recess filled with cerebrum-formed content. The anatomopathological exam revealed to be slightly differenciated malignant neoplasia with morphological and phenoetypic characteristics of a large T-cell lymphoma, ALK-positive (Figure 1).
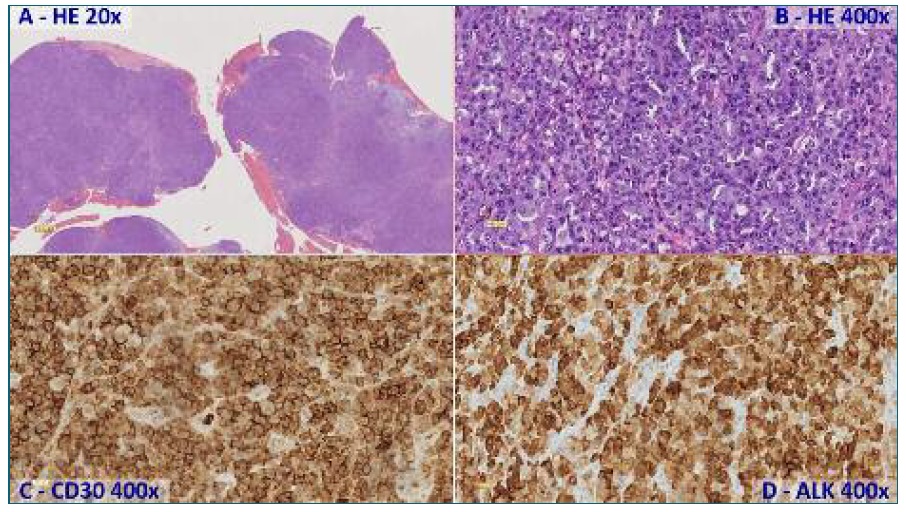
FIGURE 1 Fragments involving exclusively solid patterned neoplasia (A), consisting of big cells and moderate pleomorphism (B), which immunolabeling to CD30 (C) and ALK (D) is suggestive of anaplastic large T-cell lymphoma ALK-positive.
Staging thoraco-abdomino-pelvic contrast CT demonstrated the known left axillary mass (compatible with conglomerate lymphadenopathy), as well as two enhancing nodules located in the transition zone between the left breast and ipsilateral axilla (the largest measuring 12 mm). CT also revealed a small left pleural effusion with associated atelectasis. The bone marrow biopsy did not reveal infiltration by lymphomatous cells. Stage IIEB was attributed, the second in Ann Arbor staging system.
Accounting on patient’s young age and good performance status as well as tumour aggressiveness, it was proposed six cycles of CHOEP chemotherapy (cyclophosphamide, doxorubicin, vincristine, etoposide and prednisone) and an autologous peripheral blood stem cells (D+100) transplant afterwards. At the end of the third chemotherapy cycle, the patient had very good partial response (CT scan: enlarged left breast with marked diffuse increase in density as well as increased dermal thickness, no other relevant findings). At the end of the sixth cycle, the patient maintained similar response (PET/CT: diffusely increased left breast density and dermal thickening involving all breast quadrants. PET image showed intense and diffuse heterogeneous FDG uptake. (SUV/max.: 2,4/ hepatic SUV max.: 3,4), indicating lymphomatous disease in course). A guided needle biopsy was performed which came back negative for lymphomatous cells. The patient was considered in complete remission after chemotherapy. After the autologous blood stem cell transplant the patient remains in complete remission (negative PET/CT) for 22 months, and is currently under surveillance by the Hemato-Oncology Department.
Case Report 2
89-year-old female, no pregnancies, sent to a Senology appointment for palpable lump on the upper outer quadrant of her left breast, with 40 mm, without further signs or symptoms. Ultrasound and mammography presented a suspicious solid, hypoechoic and heterogenous node in the shift of the underarm, with irregular outlines and 37X18 mm, as well as two suspicious lymph nodes in the ipsilateral axillary region, with 7X4 mm and 14X6 mm, respectively. An ultrasound-guided microbiopsy of the breast node was performed, which resulted in follicular lymphoma (Figure 2).
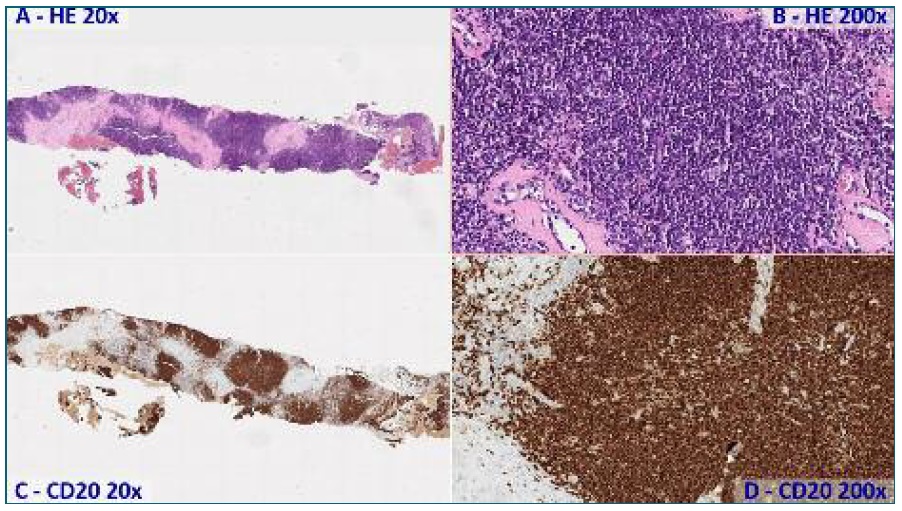
FIGURE 2 Fragments intercepted by neoplasia with geographical pattern (A) constitued by small, round blue cells (B), in which immunohistochemical study with CD20 (C, D) highlights aglomerated nodes of B lymphocytes, suggesting follicular lymphoma.
The staging thoraco-abdomino-pelvic CT scan did not reveal any other lesions and the bone marrow biopsy did not present lymphomatous cells infiltration, so a stage IEA was attribuited.
It was proposed chemotherapy with COP (cyclophosphamide, vincristine and prednisone), but the patient declined treatment and follow-up by the Hemo-Oncology Department after two cycles.
Discussion
Primary breast lymphoma is a rare tumour which incidence has been increasing, even in patients under 50-years-old. (5 The more frequent histological subtype is the diffuse large B-cell lymphoma (56-84%).1 Considering the rarity of these tumours, the abovementioned two cases represent two histological subtypes even more rare, given that the folicular lymphoma occurs in 10-19% of primary breast lymphomas and the anaplastic large T-cell lymphoma represents <1% of cases.1 That explains the small amount of case reports in literature.
As shown in these case reports and previously documented in literature, the B symptoms (fever, night sweats and weight loss) are rare1 and given that there are no clinical or pathognomonical imagiologic characteristics, the definite diagnosis and classification of the histological subtype must always be ascertained through biopsy. (1), (2), (4
The treatment of primary breast lymphoma is medical and, such as the prognosis, depends on the histological subtype, development state, size of injuries, presence or not of bilateral lesions, age and performance status of each patient, as well as one’s comorbilities, among other factors. The treatment shown in case report 1 with autologous blood stem cell transplantation with healing intent is an innovative treatment that lacks reports in literature. (6
So, the primary breast lymphoma is a rare tumour which histological diagnosis plays a pivotal part in the differential diagnosis of carcinoma. The multidisciplinary approach, including Services such Senology, Imagiology and Pathological Anatomy are essential to valuable clinical guidance of this pathology, which treatment and prognostic can vary and depend on an array of factors related to histological subtype, as well as patient and tumour characteristics.
Authors’ contributions
Cátia Sofia Ferreira, clinical data collection, literature revision and wording, article revision and approval;
Ana Helena Fachada, literature revision, article revision and approval;
Nuno Dias, availability of clinical data, interpretation and acquisition of histopathological images, literature revision, article revision and approval;
Paula Rocha, availability of clinical data, literature revision, article revision and approval;
F. Cortez Vaz, availability of clinical data, work design, article revision and approval.














