Introduction
Leiomyomas (or fibroids) are the most frequently benign smooth muscle tumor of the uterus, affecting 20%-60% of women in reproductive age and may negatively affect fertility and outcome of pregnancy.1 They are often an incidental finding discovered during an ultrasound examination performed in early pregnancy.2 The incidence of leiomyomas in pregnancy ranges from 0.1 to 10.7% and increases as the woman chooses to postpone pregnancy.1), (3), (4 True prevalence of leiomyomas during pregnancy is likely to be underestimated due to difficulty differentiating it from physiologically thickened myometrium and because most leiomyomas are asymptomatic.2), (5
A lot of ante-, intra-, and postpartum complications have been associated to leiomyomas, like spontaneous miscarriage, premature rupture of membranes, malposition of the fetus, antepartum hemorrhage, placental abruption, fetopelvic disproportion, preterm delivery, increased rate of cesarean deliveries, retention of placenta, postpartum hemorrhage and low birth weight.1), (3), (6)-(8
While often asymptomatic, leiomyomas have the potential of becoming clinically important during pregnancy, depending on size and location.2)-(4), (6 Althout leiomyomas growth pattern during pregnancy remains controversial, it seems to grow substantially during the first trimester of pregnancy. There is inconsistent evidence about the changes during second and third trimesters, but it is supposed that its growth is attenuated with minimal progress towards the end of gestation.2), (9), (10 Leiomyomas can manifest during pregnancy with pain and discomfort due to torsion or degeneration.2), (9
Postpartum spontaneous vaginal expulsion of leiomyomas is a rare phenomenon and studies reporting it are scarce. Here we present a case of spontaneous vaginal expulsion of a large hybrid leiomyoma 10-weeks after a cesarean delivery.
The report complies with the Declaration of Helsinki and it was approved by local Ethics Committee for Health research. We were given informed consent from the patient to use the medical history and images.
Case report
A 38-year-old healthy, caucasian, primigravida was referred to obstetrics appointment at our institution with a history of multiple symptomatic leiomyomas providing pelvic pressure and pain. Previously, she had been attended at our gynecology appointments for the same reason, with the greatest leiomyoma at that time measuring 110 x 80 x 88 millimeters (mm), in a subserous location (type 6 on FIGO uterine fibroid classification system) (11) on posterior wall of the uterus. She was firstly managed with ulipristal acetate (completed a 3-months cycle), and a modest reduction in leiomyomas size was observed. Two months after concluding the medical treatment, she was submitted to a laparotomic myomectomy with resection of 3 leiomyomas: the greatest a subserous with approximately 70 mm (at its largest) and two intramurals with slighter dimensions. Subsequent ultrasound performed approximately 1-year after surgery, still demonstrated the presence of leiomyomas in different locations, the greatest a type 2-5 on FIGO uterine fibroid classification system, measuring 84 x 65 x 78 mm. A second 3- months cycle of ulipristal acetate was performed and no significant reduction on leiomyomas size was observed in the ultrasound performed at the end of the treatment (the greatest leiomyoma dimensions were 81 x 67 x 80 mm). The treatment was interrupted as she wanted to become pregnant. Five-months later, she performed the first trimester obstetric ultrasound, at 13 weeks’ gestation, and multiple leiomyomas were described, the greatest an hybrid leiomyoma (type 2-5 on FIGO uterine fibroid classification system) with 119 x 146 x 150 mm on the left posterior-lateral wall of the uterus. At 15 weeks’ gestation she had an episode of left pyelonephritis. Despite that, pregnancy proceeded uneventfully, and it was shown in subsequent ultrasounds that leiomyoma size was gradually increasing. At 33 weeks’ gestation, a Magnetic Resonance Imaging (MRI) was requested to characterize the leiomyoma size and location in order to plan the mode of delivery. MRI revealed the presence of a large hybrid leiomyoma on the left posterior-lateral wall of uterus prior to fetal presentation measuring 181 x 171 x 185 mm (Figures 1, 2 and 3). It was decided to perform an elective cesarean section at 37 weeks of gestation, that went without complications. A healthy male was born, in breech presentation with 2670g and Apgar index score at 1st, 5th and 10th minutes of 9, 9 and 10, respectively. During cesarean section multiple leiomyomas were identified (the greatest with submucosal component), but no interventions were performed. A large palpable mass on abdominal wall, compatible with a leiomyoma, persisted few weeks after delivery (Figure 4). On 6-weeks postpartum evaluation she had no complains and was referred again for gynecology appointments. Approximately 10 weeks after the cesarean section, she went to the emergency department with fever, vaginal smelly discharge for 2 days, accompanied by intense pelvic pain. On gynecological examination, she presented abundant purulent foul-smelling discharge and an open cervix, with a big mass extruding from it. Ultrasound revealed a heterogeneous mass on uterine wall without vascularity, features consistent with degeneration (Figure 5). An irregular, pink, long and broad sarcoid mass was removed through the vagina by twisting off the long pedicle along with more than a liter of purulent discharge, under ultrasound control (Figure 6). On transvaginal ultrasound after the procedure, no leiomyoma or endometrial lesions were noted (Figure 7). A broad-spectrum antibiotic was administrated for 14 days. Anatomopathological evaluation confirmed a leiomyoma measuring 145 x 80 x 50 mm with signs of necrosis. The patient had a rapid recovery. Control ultrasound performed 3-months after vaginal leiomyoma expulsion revealed the presence of two submucosal leiomyomas (type 1 on FIGO uterine myoma classification system) one with 29 and another with 26 mm.
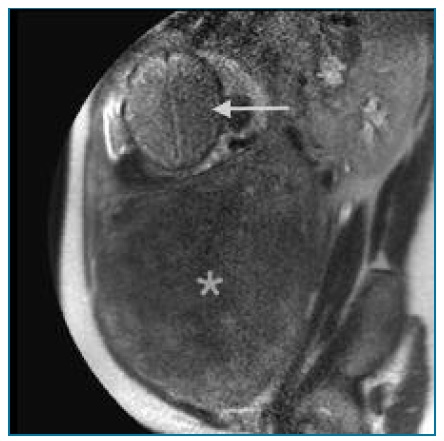
FIGURE 1 MRI showing the presence of a large hybrid leiomyoma (*) on the left posterior-lateral wall of uterus prior to the fetal (arrow) presentation measuring 181 x 171 x 185 mm.

FIGURE 2 MRI showing the presence of a large hybrid leiomyoma (*) on the left posterior-lateral wall of uterus prior to the fetal (arrow) presentation measuring 181 x 171 x 185 mm.
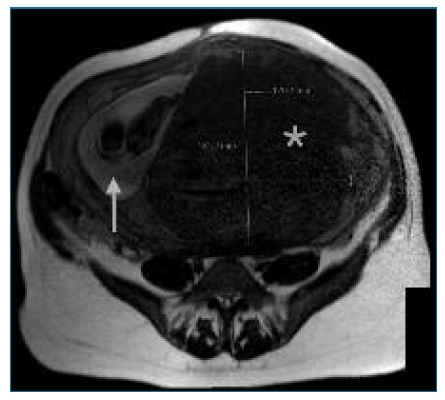
FIGURE 3 MRI showing the presence of a large hybrid leiomyoma (*) on the left posterior-lateral wall of uterus prior to the fetal (arrow) presentation measuring 181 x 171 x 185 mm.

FIGURE 4 Immediate postpartum after cesarean delivery: a large palpable mass on abdominal wall, compatible with a leiomyoma persisted after delivery.
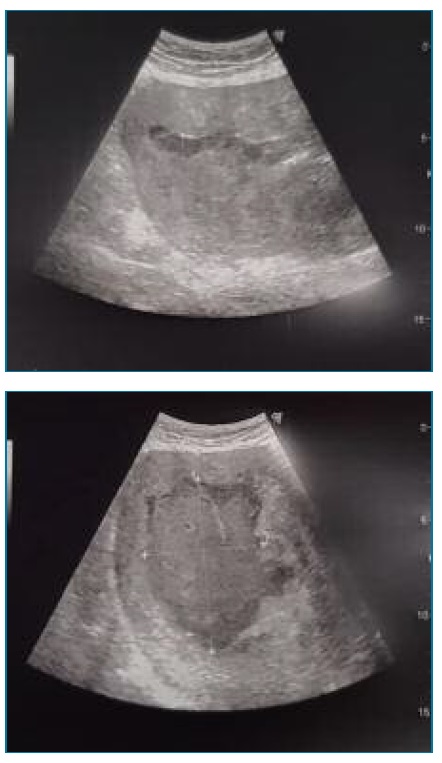
FIGURE 5 Ultrasound revealing a heterogeneous mass on uterine wall with features consistent with degeneration and no vascularity.

FIGURE 6 An irregular, pink, long and broad sarcoid mass was removed through the vagina by twisting off the long pedicle along with more than a liter of purulent discharge.
Discussion
Due to increasing maternal age, leiomyomas are becoming more frequent among pregnant women.1), (3 The patient in our case has 38-years-old and history of multiple leiomyomas. The greatest leiomyoma growth seems to have occurred during first trimester (doubled in size from 81 mm to 150 mm, at its largest) and continued to grow until 33 weeks’ gestation (185 mm, at its largest). The effect of pregnancy on leiomyomas size and its growth pattern remains a controversial subject.2), (9), (10 During postpartum period, the majority of leiomyomas do not change, however some reduce its dimensions.9 Size, number and location of leiomyomas are the most important factors influencing pregnancy outcomes. Considering the location, there is evidence that submucosal leiomyomas may impair fertility and affect pregnancy outcomes.8 Impact of intramural leiomyomas on reproductive potential is not clear, but some studies reported a causal relationship between leiomyomas larger than 40 mm and infertility.7 The only complications this patient had during pregnancy was an episode of left pyelonephritis at 15 weeks’ gestation and malpresentation of fetus. This last one, has been consistently associated to leiomyomas by other studies.1), (3), (6), (8 Urinary retention has also been described12 and by promoting urinary stasis it may contribute to a higher risk of urinary tract infections.
Spontaneous vaginal expulsion of uterine leiomyomas is a rare phenomenon, especially in young women. The causes of spontaneous expulsion are not yet well understood. It is supposed that ischemia followed by necrosis of leiomyomas is the main mechanism for dead tissue expulsion.13 Leiomyoma necrosis and subsequent vaginal expulsion occurs mostly following uterine artery embolization. Other factors that have been associated includes drug administration, intrauterine devices, miscarriage and cesarean delivery. (13 Red degeneration is the most common type following delivery, and this occurs because blood supply can no longer support the growing leiomyoma. (14 In postpartum, uterine contraction and softening of cervix might also contribute to the expulsion process. (15 Preceding vaginal leiomyomas expulsion most women present with severe abdominal pain, fever, vaginal bleeding, smelly discharge and feel of an extrusion mass through vagina. (13)-(17 In this case, vaginal leiomyoma expulsion occurred 10-weeks after the cesarean section however, in most reported cases leiomyomas expulsion occurred in the first 6-weeks following delivery14-17 and were related to submucosal or cervical leiomyoma. (15)-(17 Sagoo et al. reported a case of spontaneous vaginal expulsion of an intramural leiomyoma and they hypothesized that the thinning of uterine cavity was the only possible explanation for how an intramural leiomyoma which was completely surrounded by thick uterine muscle could have become submucosal and be expelled through vagina. They also postulated that postpartum physiological involution of uterus, may push intramural leiomyoma towards the line of the least resistance (uterine cavity) and interrupt its blood supply, promoting ischemia and then necrosis of the leiomyoma. (14
Self-expulsion of a leiomyoma might be a life threathning condition due to delay in diagnostic process and implementation of treatment. If fragments of degenerated leiomyoma become trapped in the uterine cavity or if the evacuation process is slow, the necrotic tissue can become infected with development of pyomyoma. Degeneration of leiomyomas will remain an unusual cause of postpartum fever and sepsis, however it is important to consider this as a differential diagnosis.
This case highlights the importance of early identification of leiomyomas (location, number and size) and close surveillance of its growth during pregnancy in order to prevent adverse pregnancy outcomes. It also describes a rare occurrence of spontaneous vaginal expulsion of an hybrid leiomyoma 10-weeks after delivery.