Introduction
Toker cells (TC) are epithelial cells with clear cytoplasm localized within the basal layer of the nipple epidermis, first described in 1970 by Cyril Toker.1 TC are seen in about 10% of nipple sections with hematoxylin and eosin (H&E) staining1, but recent advances in microscopy enabled their identification in up to 90% of specimens using cytokeratin 7 (CK7) staining.2
More rarely, TC are found in increased number, which is referred to as TC hyperplasia (TCH).3 Tommaso et al4 suggested to consider hyperplastic cases showing >10 isolated TC, or small clusters of >3 TC, that persist or increase after several sections and lack of cytological atypia. In most cases, TCH is a rare incidental histological finding, seen in less than 3% of nipple specimens.3 TC prevalence appears to distribute evenly among sexes and regardless of age.1),(4
TC origin is not fully elucidated, and their pathologic potential remains controversial. Some authors believe that TC represent the benign counterpart of the malignant cells of Paget’s disease (PD), due to their remarkable immunohistochemical similarities;1 others argue that TC are probably precursors of Paget’s cells.5),(6 Nevertheless, it is known that a fraction of TC can acquire the ability to proliferate and expand.3
We report a case confirmed of TCH in a nipple, from Centro Hospitalar Universitário Cova da Beira (CHUCB), with at least 17-years duration and associated with a non-specific chronic inflammatory lesion and no underlying breast disease, and a thorough review of cases reported in literature regarding TCH.
Case report
An 82-year-old woman, Caucasian, came to the office of Gynecology and Obstetrics Service from CHUCB, on 16/07/2018, referred by her Family Doctor. The cause of referral was an eczematous lesion in her left nipple, recognized by her as present for the last 17 years. She stated not have accompanying symptoms nor local trauma, why she has never sought medical attention. The lesion was noted during a routine examination by her Family Doctor, who immediately scheduled the referral. Past medical history, both gynecological and personal, was unremarkable. There was not known family history of breast disease. The patient was inquired about the possibility of publishing a case report and has provided her written informed consent.
Physical examination revealed a non-pruritic, erythematous desquamating lesion, involving the left nipple-areolar complex, with well-defined irregular borders (Figure 1). Breast exam revealed a non-tender breast and absence of palpable lymph nodes or nipple discharge. Patient’s last mammography, performed earlier in 2018, demonstrated no evidence of underlying disease - BI-RADS-1 (American College of Radiology).7
To obtain a definitive diagnosis, we performed a punch biopsy with a Keyes dermal punch number 6, obtaining a cylindrical specimen of 50mm in diameter and 40mm in depth. Histological study with H&E staining showed epithelioid cells, isolated or in clusters, scattered throughout the epidermis, with minimal atypia, fine chromatin, small nucleoli, and abundant clear cytoplasm. Additionally, it was identified a mild chronic inflammatory process associated with hyperkeratosis. Dysplasia or malignant neoplasia was not observed (Figure 2).
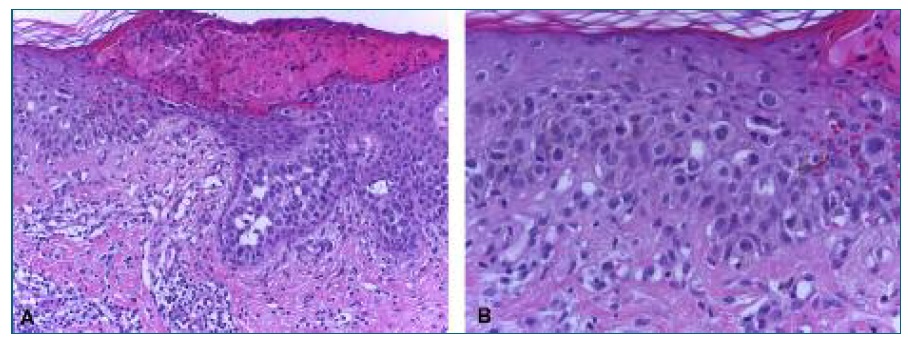
FIGURE 2 Histopathologic examination showing cells with abundant clear cytoplasm within the epidermis. H&E staining, (A) magnification x20, (B) magnification x40.
Histochemical staining with periodic acid-Schiff (PAS) and PAS-diastase (PAS-D) for mucins was negative. Immunohistochemical study, performed with Automated Immunostaining Ventana BenchMarckTMXT (Fritz Hoffmann-La Roche Ltd, Basel, Switzerland) using UltraView Dabv3 kit (Ventana Medical Systems, Arizona, USA), showed immunoreactive staining for CK7, carcinoembryonic antigen (CEA), epithelial cell adhesion molecule (EpCAM) and estrogen receptor (ER) (Figure 3), but lack of reactivity for cytokeratin 5/6 (CK5/6), cytokeratin 20 (CK20), the neural/melanocytic marker (S100), gross cystic disease fluid protein 15 (GCDFP-15), the myoepithelial marker member of p53 gene family p63 (henceforth, p63) and the human epidermal growth factor receptor 2 (HER2/neu).

FIGURE 3 Immunohistochemical study showing reactivity for CK7 (A, magnification x10), CEA (B, magnification x10), EpCAM (C, magnification x10) and ER (D, magnification x10).
Morphologic and immunophenotypic profile of the specimen matched the diagnosis of TCH associated with a non-specific chronic inflammatory lesion. Surgical excision of the affected area was proposed to the patient, which she declined. Therefore, clinical surveillance was scheduled.
Discussion
The differential diagnosis of the lesions of the nipple includes: PD of the breast, malignant melanoma, nipple eczema, psoriasis or nipple fungal infection.8),(9 Promptly evaluation for excluding malignancy, particularly PD, is mandatory, and biopsy is fundamental to achieve a definitive diagnosis (Table I).
table I Morphological and immunohistochemical characteristics of toker cells and paget cells. Adapted from references8),(9),(10.
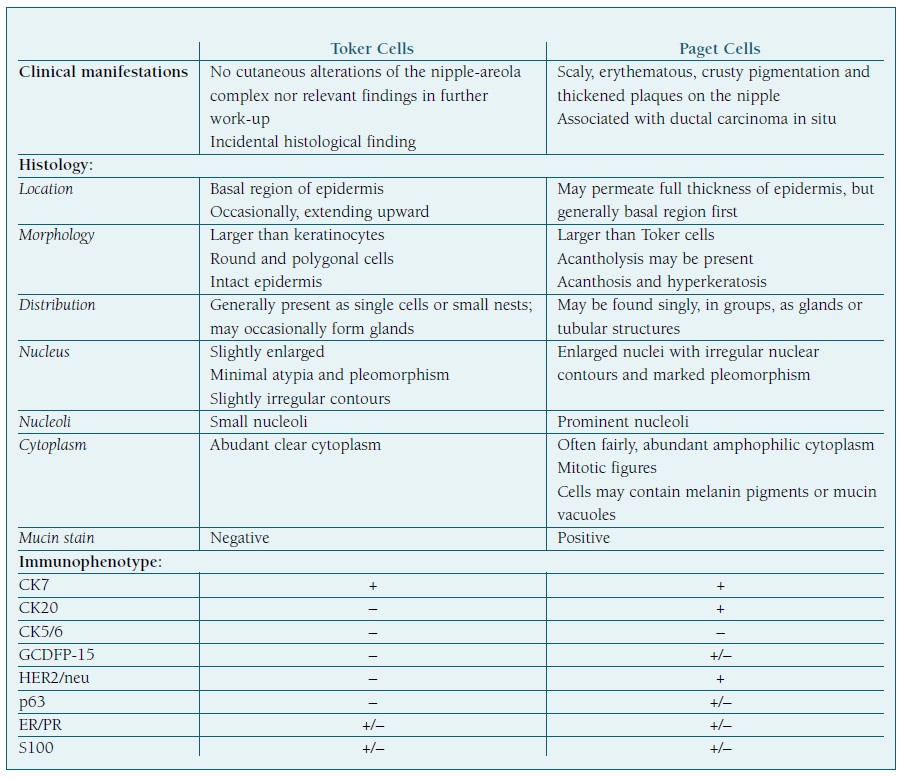
Legend: -, lack of immunoreactivity; +, positive immunoreactivity; +/-, variable immunoreactivity.
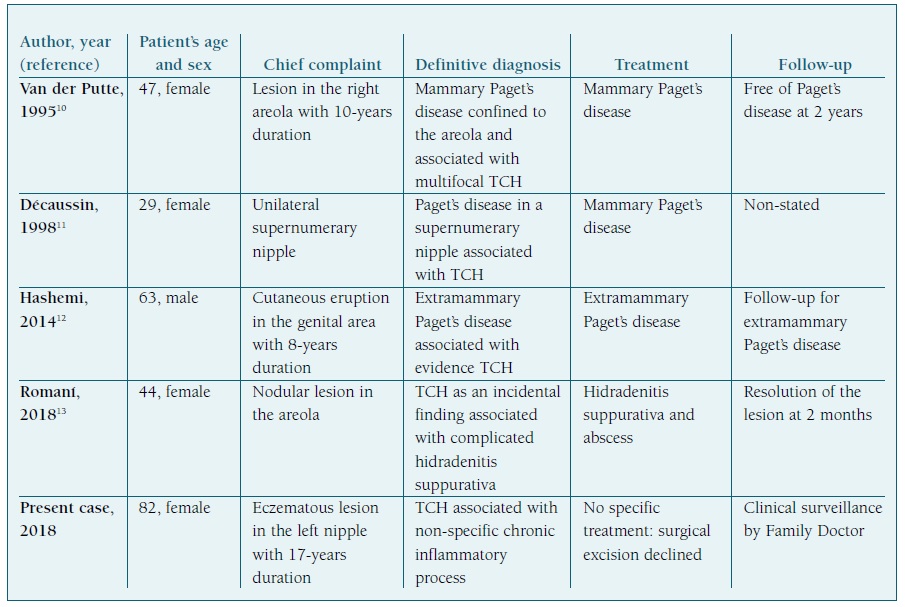
TCH is a rare entity recognized by the scientific community, but seldom mentioned in Literature. Four case reports were found regarding this condition (Table II).
Van der Putte et al11 reported in 1995 a case of mammary PD (MPD) confined to the areola and associated with multifocal TCH, in a 47-year-old woman. Immunohistochemical staining of the sections showed reactivity for CAM 5.2, EMA, RE and RP, compatible with TCH.
Décaussin et al12 reported in 1998 a case of PD arising in a supernumerary nipple of a 29-year-old woman without an underlying carcinoma and associated with TCH. Immunohistochemical staining of TC showed reactivity for CEA and EMA, while negativity for HER2/neu was observed.
In 2014, Hashemi et al13 reported a case of multicentric primary Extramammary PD (EMPD) with evidence of TC proliferation, in a 63-year-old white man. TC were morphologically identified in increased number within the epidermis surrounding the EMPD. These authors suggested that TCH was a precursor to EMPD.
Recently, in 2018, Romaní et al14 reported a case of TCH as an incidental histological finding in a biopsy, performed to exclude MPD, of a complicated hidradenitis suppurativa affecting the breast region, in a 44-year-old woman. Immunohistochemical staining showed reactivity for CK7, low molecular weight anticytokeratin 5.2 (CAM 5.2), epithelial membrane antigen (EMA) and ER, but lack of reactivity for CEA, the marker of cell proliferation Ki-67 (henceforth, Ki-67), tumor suppressor gene product p53 (henceforth, p53) and HER2/neu, supporting the diagnosis of TCH.
We report a case of an 82-year-old asymptomatic woman with an eczematous lesion of the nipple, with immunohistochemical staining showing reactivity for CK7, CAM 5.2 and EMA, but lack of reactivity for HER2/neu, and negativity for mucin staining. These findings, along with morphological characteristics and clinical background, supported the diagnosis of TCH associated with a non-specific chronic inflammatory lesion.
In the reported cases, as in ours, imaging demonstrated no evidence of underlying malignancy. However, in our patient, we have not identified any specific skin condition besides a mild non-specific chronic inflammatory process, which differs from previous reports, in which TCH was associated with cutaneous disease, particularly PD. Hence, surgical excision of the affected area was proposed, which the patient declined.
Attending to the patient’s advanced age, chronic course of the lesion and the lack of evidence of malignancy or other skin condition in our case, we might be induced to regard TCH as a rare manifestation of natural cutaneous aging process. Nevertheless, some authors consider TCH as a lesion associated with PD. Given this controversy, we must look cautiously to this findings and further research is needed to clarify this association.
Regardless of the chronic course of the lesion, only biopsy yielded the definitive diagnosis and excluded malignancy. We emphasize, therefore, that any eczematous lesion of the nipple should be subjected to histological study.