Introduction
Ectopic pregnancy happens when implantation of the blastocyst occurs somewhere other than the uterine endometrial cavity. The most common site of implantation is the ampullary portion of fallopian tubes, which accounts for 70% of ectopic gestations1.
The interstitial implantation is rare, with an incidence between 2-3%1), (2. It occurs when the blastocyst implants in the proximal segment of the fallopian tube, located into the myometrial wall3.
The risk factors for an interstitial pregnancy (IP) are the same as for ectopic pregnancies in general, and include everything that affects the normal tubal anatomy and function, such as previous ectopic pregnancy, surgery, infections, congenital anomalies, smoking and hormonal contraception4), (5. However, an history of ipsilateral salpingectomy is a specific risk factor for development of IP6), (7.
IP has higher risk of bleeding and uterine rupture, even in the early stages of pregnancy, due to the presence of vascular anastomosis between uterine and ovarian arteries3), (8), (9. It can be managed surgically or medically, according to its clinical presentation and serum human chorionic gonadotropin (HCG) levels3.
The authors report two cases of IP, one of them managed with a surgical laparoscopic procedure and the other treated conservatively with intramuscular methotrexate (MTX).
Case report 1
A 28-year-old pregnant woman went to a routine antenatal appointment to begin pregnancy surveillance. It was her third gestation. She had a normal delivery 3 years before and an ectopic left tubal pregnancy that was treated with laparoscopic salpingectomy, 2 months before. Other than this, her medical history was irrelevant.
She had 7 weeks and 3 days of menstrual delay and was completely asymptomatic.
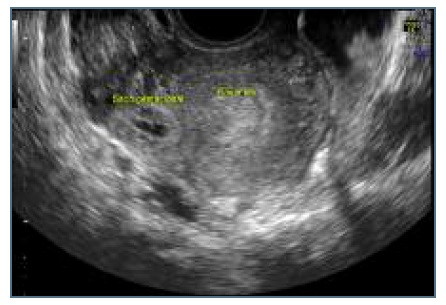
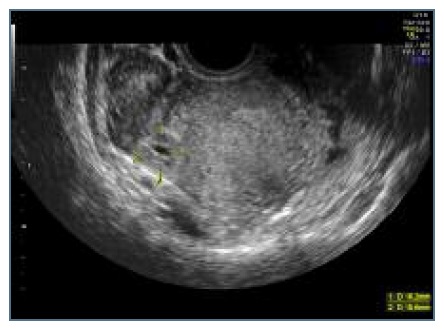
We did a transvaginal ultrasound that revealed the presence of a rounded anechoic mass in the interstitial portion of the left tube, with maximum diameter of 1,7 centimeters and peripheral ring vascularization. This mass was delimited by a hyperechoic wall and contained a yolk-sac but no visible embryo, and it was surrounded by a thin myometrial layer. It caused a bulging of the external limit of the uterus and had no communication with the endometrium (Figures 1 and 2). Three-dimensional (3D) ultrasound findings were also in line with the previous suspicion of an ectopic pregnancy in the interstitial portion of the left tube (Figures 3 and 4). There was also a decidual reaction in the uterine cavity and an hematometra. No free fluid was detected in the pouch of Douglas.

Figure 1 Ultrasound image: ectopic mass separated from endometrial cavity, surounded by thin myometrium.

Figure 2 Ultrasound image: ectopic mass with 1,7cm, delimited by a hyperecoic wall, with yolk-sac but no embryo.

Figure 3 Ultrasound 3D scan: ectopic mass without communication with uterine cavity and causing an external bulging in the uterine wall.
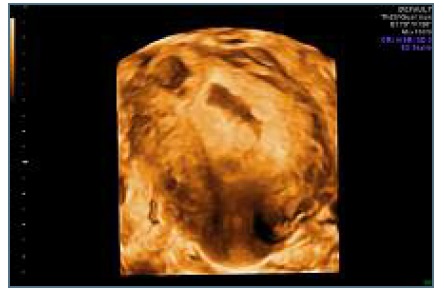
Figure 4 Ultrasound 3D scan: ectopic mass without communication with uterine cavity and causing an external bulging in the uterine wall.
Her laboratory results revealed a HCG level of 17,013 UI/L.
She was immediately referred to the emergency department where she was submitted to a laparoscopy, which showed an ectopic pregnancy in the left cornual region of the uterus (Figure 5). We performed a laparoscopic excision of the ectopic mass, using bipolar electrocoagulation and laparoscopic scissors. After removing the mass, intracorporeal knots were used to close the uterine incision and to assure hemostasis (Figure 6). The intraperitoneal pressure was then diminished to 4 mmHg to confirm hemostasis. There were no hemorrhagic points, hence we used an haemostatic knit - Surgicel ® NU-KNIT - to cover the suture in order to prevent further blood loss. The surgery lasted 50 minutes and the amount of blood loss was 50 milliliters.

Figure 6 Laparoscopic image: small incision of the uterus after removing the mass and closing with intracorporeal knots.
No postoperative complications were reported and the laboratory results showed a significant decrease of the HCG serum concentration to 4651 Ul/L, one day after the surgery. She was discharged in the first postoperative day.
Pathological results confirmed our hypothesis of an interstitial ectopic pregnancy.
Two weeks later, in the postoperative appointment, she was asymptomatic, her gynecological exam was normal and the incisions were healing well.
She underwent weekly monitoring of HCG levels, which were in a descending pattern and became undetectable four weeks after surgery.
Case report 2
A 22-year-old women, 5 weeks and 4 days pregnant, presented to the emergency department of our hospital with complaints of vaginal bleeding and pelvic pain. It was her second pregnancy, as she had an abortion without curettage one year before. Her personal and medical history was irrelevant.
The transvaginal ultrasound identified an eccentric gestational sac in the right cornual region, surrounded by a thin myometrial layer, with maximum diameter of 1,6 centimeters. (Figures 7 and 8) This gestational sac was empty and had a hyperechoic wall and peripheral ring vascularization, as is expected from trophoblastic tissue. (Figure 9) This sac had no communication with the endometrium and caused a bulging of the external limit of the uterus, which was confirmed by the 3D ultrasound images. (Figure 10) There was a decidual reaction in the uterine cavity.
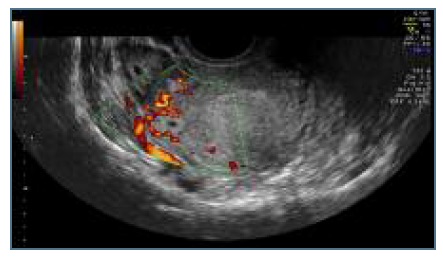
Figure 9 Ultrasound image: gestacional sac with hyperecoic wall and peripheral ring vascularization.
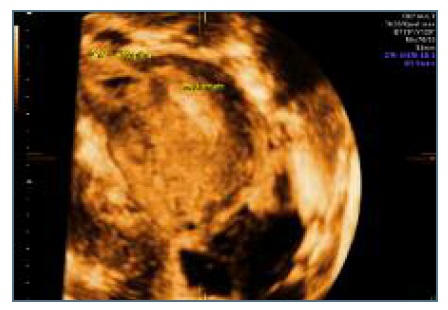
Figure 10 Ultrasound 3D scan: ectopic mass without communication with uterine cavity and causing an external bulging in the uterine wall.
Moreover, her HCG level was 3,733 UI/L.
Thereon, we proposed her conservative treatment with intramuscular administration of MTX, that she accepted. After confirming normal blood count and liver function, we treated her with 80 mg (50mg/m2) of MTX and she was discharged.
Her HCG levels were closely monitored and the values showed a decrease of 17% between day 4 and day 7, which was in line with a successful treatment.
During the follow-up period she was asymptomatic and her HCG levels continued to descend until became undetectable one month after treatment.
Discussion
IP is a rare condition associated with a high rate of complications as it can lead to uterine rupture with possible life-threatening hemorrhage, usually occurring in the early stages of pregnancy3), (8), (9), (10), (11. However, as the trophoblastic tissue is implanted in the myometrial layer, the pregnancy can also develop and reach advanced gestacional ages without causing any alarm symptom. It is challenging to diagnose IP that may be misdiagnosed as an angular pregnancy - an intrauterine pregnancy that extends into the lateral “angle” of the uterine cavity12. An early diagnosis is essential to prevent complications and to select the proper management strategy3), (13.
In both cases, the women were asymptomatic or had few and unspecific symptoms. This highlight the importance of a high suspicion level, specially in the presence of specific risk factors, like previous ipsilateral salpingectomy, as happened in the first case.
Besides clinical history, laboratory and ultrasound findings are equally important.
An empty uterine cavity and eccentrically located gestational sac surrounded by incomplete myometrium with thickness smaller than 5 mm were described as highly suggestive ultrasound indicators of IP3), (13), (14.
As we can see in the ultrasound images, the gestational sac has an eccentric location and the uterine cavity appears empty, corroborating the diagnosis with a high level of certainty. Additionally, the coronal 3D scans give us a better view of the fundal and cornual regions of the uterus, confirming the absence of communication between the sac and the endometrium and the presence of an external bulging of the uterus induced by the ectopic mass.
As for the treatment, current data supports the most conservative treatment possible, in order to preserve uterine integrity and subsequently improving future fertility and future obstetric outcomes7), (11. There are no published treatment guidelines for IP, so the treatment should be individualized.
Medical treatment with MTX is an option to initial, non-complicated, selected IP15), (16. Intramuscular injection of MTX was administered successfully in the second case. It was an early pregnancy, with relatively low HCG levels and an empty gestational sac. Therefore, we opted for a conservative management that proved to be effective, did not cause any side effects, complications or suspected sequelae in the woman’s reproductive future.
When surgery is required, there has also been a progression towards more conservative techniques, such as laparoscopic cornuostomy or laparoscopic cornual resection.
In a laparoscopic cornuostomy we are able to remove the gestational tissue without removing the surrounding myometrium, so the uterine integrity is better preserved than in a cornual resection7.
Some authors suggest that the size of the ectopic mass should determine the choice between these two techniques, defining that when the mass is over 3,5-4 centimeters a cornual resection is more appropriate17), (18. However, at least equally important is the extent of penetration into the myometrium, that should be accessed during surgery and can preclude a more conservative approach.
In our first case, we chose to perform a cornuostomy to excise the ectopic mass, using bipolar coagulation and cutting, as the mass was located superficially and the surrounding myometrium did not appear too damaged. We were able to remove the mass with a small amount of blood loss and a small incision in the uterus that was then sutured and closed with intracorporeal knots.
It was an effective, minimally invasive surgery, without any peri- or post-operative complications.
Since the ectopic mass had similar dimensions, the choice of medical treatment in one case and surgical treatment in the other was based on the HCG levels, as a high concentration is associated with MTX treatment failure, more marked when inicial HCG is above 5000IU/L19), (20.
Persistent ectopic pregnancy is an important complication of both conservative surgical approach and medical treatment7. Therefore, appropriate selection of cases and close monitoring of HCG levels after treatment are crucial. In both cases we observed a solid decrease of HCG levels, that ensured the treatment was successful as all gestational tissue was removed.
To conclude, more conservative treatment options should be recommended in selected cases, as they proved effectiveness without increased morbidity and few future sequelae.
Both patients signed an informed consent for publication of the case report.