Introduction
Hydatidiform mole (HM) is part of a group of uncommon conditions classified as Gestacional Trophoblastic Diseases (GTD), which originates in the placenta and have the potential to locally invade the uterus and metastasize1), (2. HM is categorized as partial hydatidiform mole or complete hydatidiform mole based on morphology, histopathology, karyotype and risk of malignancy2. When GTD recurs, is invasive or there’s evidence of metastatic disease it is called Gestational Trophoblastic Neoplasia (GTN) (3.
Although the reported incidence of HM varies widely around the globe, it is mostly around 1 per 1000 pregnancies. The two main risk factors for developing HM are history of previous mole and extremes of reproductive age1), (2), (4. Women over 45 years old have a 5-10 times increased risk for developing HM and the risk for the development of complete HM at a postmenopausal age is greater than partial HM1), (2), (5), (6. Moreover, in women over 40 years old HM develops more frequently severe complications, like theca lutein cysts, hyperemesis gravidarum, severe hyperthyroidism or early onset of preeclampsia2. That said, HM is extremely rare in perimenopausal woman7.
We present a rare case of complete HM presenting with severe preeclampsia in a perimenopausal woman. An informed consent was obtained from the patient for the elaboration of this article.
Case report
A 50-year-old perimenopausal caucasian woman, gravida 2 para 2 (two vaginal deliveries), was referred to our institution by her general practitioner doctor for suspicion of molar pregnancy. The patient consulted her doctor due to a three-week long vaginal bleeding and feet edema for the last four days. Transvaginal ultrasound revealed a uterus of increased dimensions at the expense of voluminous hyperechogenic and heterogeneous intrauterine formation in the fundus region, with internal hypoechogenic areas, measuring approximately 105x97x122mm with echographic characteristics of a complete hydatidiform mole (HM), without unequivocal signs of fetus or fetal parts (Image 1).
The patient had a history of total thyroidectomy and was medicated with levothyroxine 125 micrograms with recent normal analytical thyroid function. She had two children and her last pregnancy was 23 years back. She stopped combined oral contraceptive pill 10 months ago and she experienced menstrual irregularities afterwards (last vaginal bleeding the month before and five months before that).
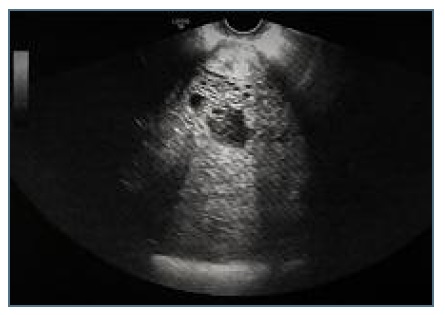
Figure 1 Transvaginal ultrasonograghy showing a heterogeneous intrauterine formation with vesicular pattern.
Arriving our institution, the patient’s only symptom was vaginal bleeding. At physical examination blood pressure was 155/80 mmHg; she denied headache, epigastric pain or visual symptoms. She had no personal history of chronic hypertension. On gynecologic examination there was no vulvar, vaginal or cervical lesions and an enlarged uterus was noted. Transvaginal ultrasound was repeated and findings were in accordance with the ultrasound previously reported. Blood analysis revealed hemoglobin 10,2 g/dL, platelets count 110.000 x 106/L. Liver enzymes were elevated (aspartate aminotransferase (AST) 89 Ul/L, alanine aminotransferase (ALT) 163 Ul/L), serum total bilirubin 1.14 mg/dl, unconjugated bilirubin 0.35 mg/dl; thyroid function was compatible with hypothyroidism (free thyroxine (T4) 1.24 ng/dL, thyroid stimulating hormone (TSH) 7.520 Ul/mL)). Serum hCG was >200.000 mUl/mL. The diagnosis of complete HM was assumed and the patient was admitted in our institution for further evaluation. A few hours after admission the combination of severe hypertension despite parenteral medication (blood pressure values reaching 205/105 mmHg), thrombocytopenia and liver dysfunction in the laboratory work up raised the suspicion of severe preeclampsia and an emergent abdominal hysterectomy with bilateral salpingo-oophorectomy was performed. On gross examination the uterus weighed 495g and was 17cm high (Image 2) and the uterine cavity was entirely occupied by spongy, hemorrhagic tissue with the presence of countless vesicular formations of varying size. Histological examination described molar pregnancy with characteristics of a complete HM and there were no morphological aspects of aggressive behavior, namely invasion of the myometrium. Day 1 after surgery, patient’s blood pressure remained high, reaching a maximum of 183/95 mmHg, and was only stabilized after parenteral treatment with labetalol and captopril. On the 3rd day after surgery, analytical profile improved and serum hCG was significantly lower at 74.116 mUl/mL. A chest computed tomography (CT) was performed and described a consolidation of the alveolar pattern in the anterior and laterobasal segment of the lower lobe of the right lung, extending to the base of the middle lobe that was compatible with pneumonia, without signs of pulmonary metastasis. The patient had no respiratory symptoms and after evaluation by Internal Medicine she was empirically medicated for pneumonia with amoxicillin with clavulanic acid. She was discharged on the seventh postoperative day. Serum hCG values dropped consistently and reached normal reference range (<5 mUl/mL) six months after surgery. The patient remains under surveillance in our institution.
Discussion
We present a rare case of a HM with severe preeclampsia in a perimenopausal woman. Perimenopause is characterized by menstrual cycle changes and irregularities and vaginal bleeding in this period is most commonly due to anovulatory cycles and structural abnormalities such as uterine fibroids, endometrial polyps and endometrial hyperplasia/neoplasia8), (9. As pregnancy is not a frequent diagnosis, a pregnancy test is not always included in an initial approach of these patients, whereby the diagnosis of HM may be missed at first10. Late diagnoses of HM can expose these women to serious complications, namely preeclampsia, as seen in the presented case.
Clinically, vaginal bleeding and an enlarged uterus are common presenting symptoms of HM. Very high levels of serum human chorionic gonadotropin (hCG) (> 100.000 mUl/mL) support the diagnosis. Transvaginal ultrasound can raise a high suspicion of the diagnosis, especially in complete HM, and sonographic findings include the presence of a central heterogeneous mass with numerous discrete anechoic spaces, which correspond to the hydropic villi, and the absence of an embryo or fetus and amniotic fluid. However, definitive diagnosis is histological1), (2. In this case the diagnosis of complete HM was suspected due to ultrasound findings and maternal serum hCG >200.000 mUl/mL. In complete HM, high levels of hCG can lead to development of complications as previously mentioned, however, nowadays preeclampsia as a complication of complete HM is less common and it usually occurs when the diagnosis is delayed2), (5), (10), (11. In this case diagnosis of severe preeclampsia was made by the patient’s hypertension with systolic blood pressure over 160 mmHg and diastolic blood pressure over 110 mmHg, despite parenteral medication, and liver dysfunction with patient’s liver transaminases being greater than twice the upper limit of normal reference values12.
Suction uterine evacuation is the preferred method of treatment of HM, but primary hysterectomy can be an option if childbearing is complete2), (13), (14. Preeclampsia in HM usually also resolves after uterine evacuation13. We performed an abdominal hysterectomy given the patient’s clinical and analytical aggravation combined with her wish of permanent contraception. Hysterectomy has an advantage of treatment, permanent sterilization and decreases the need of subsequent chemotherapy and further risk of postmolar GTN1), (4. As HM is considered a premalignant disorder, follow-up with hCG monitoring is mandatory to confirm resolution of disease or to identify development of GTN, even after performing hysterectomy, once surgery does not prevent all cases of metastatic disease and in this cases the risk of postmolar GTN remains at 8-20%, especially in older women1, (10), (13), (15. Postmolar GTN is very rare after the spontaneous return of hCG levels to normal2), (13.
In conclusion, although HM is rare in perimenopausal woman, the condition can present with severe complications. When perimenopausal patients present with irregular vaginal bleeding the possibility of pregnancy should always be considered and HM must be recognized as differential diagnosis.















