Introduction
The identification of anti-N-methyl-D-aspartate encephalitis receptor (NMDAR) encephalitis made it possible to recognise that some patients with rapidly progressive psychiatric symptoms, cognitive impairment, seizures, movement disorders, or coma of unknown cause, had an autoimmune disease1. It is characterised by a complex neuropsychiatric syndrome and by the presence of cerebrospinal fluid (CSF) antibodies against the GluN1 subunit of the NMDAR, which is particularly important for controlling synaptic plasticity and memory function1.
The disease was first described in 2007 as one of the most common autoimmune encephalitis, with female predominance (a female to male ratio of around 8:2), affecting mainly children or young adults with a median age of 21 years-old (range < 1- 85 years). The clinical presentation is deverse and frequent association with tumours (mostly ovarian teratoma) (1), (3. Very often, the diagnosis is not straightforward due to its heterogeneous clinical presentation, requiring a high index of suspicion in order to make a prompt diagnosis and start the effective treatment2.
A paraneoplastic mechanism has been proposed: disruption of immunologic self-tolerance to NMDAR expressed by neuroglial tissue in the ovarian teratoma results in abnormal production and circulation of NMDAR antibodies that subsequently enter the central nervous system (CNS) (5. Despite the severity of the disorder, patients often recover after tumor removal and immunotherapy1. The paraneoplastic mechanism of disease may not explain all cases of this syndrome, as some patients do not have a detectable tumour and can be triggered by viral illness, mostly commonly found with herpes simplex virus (HSV) (4.
Case report
A 22-year-old woman, nulliparous, with no previous psychiatric history, was admitted to the Emergency Department of a Tertiary Hospital for tonic-clonic seizures with response levetiracetam. Additionally, she referred a 2 weeks history of insomnia, irritability, unusual behaviour and abnormal stereotyped limb movements, for which she was assessed by a psychiatrist and medicated with neuroleptics, without symptomatic improvement. On examination a severe memory, attention and language impairment was noted without other neurological focal signs. Initial laboratory studies with complete blood count, metabolic and toxic panel had no major alterations. Brain Computed Tomography (CT) was normal as well as brain Magnetic Resonance Imaging (MRI). Lumbar puncture showed lympho-cytic pleocytosis. Search for CSF antineuronal antibodies was performed. Given the clinical picture of neuropsychiatric signs and symptoms in a young woman, anti-NMDAR encephalitis was considered the most probable diagnosis and a 5-day course of methylprednisolone followed by a 5-day course of immunoglobulin were initiated on empiric basis. Acyclovir 750 mg 8/8h i.v. was also empirically started until a herpetic encephalitis could be excluded.
A gynaecology ultrasound was performed: inside of the parenchymal of the left ovary (24x16x27 mm) was identified a mass with 13x12x15 mm corresponding to a unilocular cyst, with mixed echogenicity, presence of shadowing an no vascularization with colour Doppler. Applying IOTA Simples Rules, this adnexal mass was classified as benign and according to the IOTA-ADNEXAL Model the chance of being a benign tumour was 99.9%. The tumoral markers (CA-125, alfa-fetoprotein and hCG) were negative. The ultrasound features of left adnexal mass suggested an ovarian teratoma. (Figure 1)
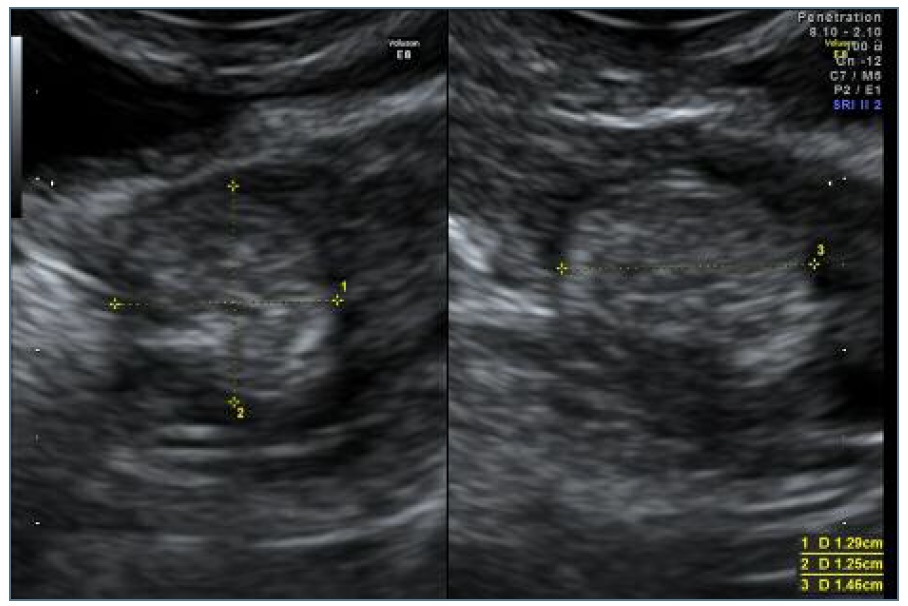
Figure 1 Unilocular cyst, with mixed echogenicity, presence of shadowing and no vascularization at colour Doppler (IOTA Terminology).
Subsequently, 35 hours after the ultrasound, the patient underwent a laparoscopic surgery and a left adnexectomy was performed, since the small dimension of the dermoid cyst precluded its clear individualization and complete ressection. (Figure 2) After the surgery, the patient showed a progressive and significant recovery of cognitive and behaviour functions and was discharged after 17 days with a moderate episodic memory and attention impairments. One month after discharge, only mild episodic memory impairment was noted with no episodes suggestive of seizures or abnormal behaviour.
CSF anti-NMDAR antibodies were positive and PCR for HSV1 and HSV2 were negative. The pathological diagnosis of left adnexal mass was a 15 mm trigeminal teratoma.
Discussion
Two confirmed triggers of anti-NMDAR encephalitis are tumours (mostly ovarian teratomas) and HSV infection1), (5. Its real incidence is unclear, but studies suggest that it is the most frequent antibody-mediated encephalitis6. The only specific diagnosis test of anti-NMDAR encephalitis is the demonstration of IgG antibodies against the GluN1 subunit of the receptor in patient´s CSF6. Recovery from anti-NDMAR encephalitis occurs as a multistage process that happens in the reverse order of symptom presentation7. Patients undergoing early tumour removal have a better outcome and recovery than those which tumour is belatedly removed7. In the acute stage of the disease, many patients need to be hospitalised for at least 3-4 months, including admission to an Intensive Care Unit due to severe autonomic dysfunction and central hypoventilation, followed by several months of physical and behavioural rehabilitation1. Recovery from this disorder is typically slow, and symptoms may relapse. Mortality rates varies from 4% to 8-10% in the different studies3), (4), (5. The first management should focus on immunotherapy and the detection and subsequent removal of an identified tumour8. In patients without tumour or a late diagnosis, additional treatment with second-line immunotherapy (rituximab or cyclophosphamide) is required7. It is reasonable to hypothesize that, in this particular case, the time between the onset of the symptoms, and the teratoma identification by ultrasound and subsequent laparoscopic surgery, prevented a severe clinical worsening of the patient condition: coma, respiratory failure and need for Intensive Care Unit. This case report contributes to better elucidate the importance of recognizing the wide spectrum of signs and symptoms of anti-NMDAR encephalitis to rapidly engage diagnosis workup and treatment. It shows the importance of an gynaecological ultrasound screening when the diagnosis is suspected.















