Introduction
Uterine leiomyomas are benign tumors arising from smooth muscle cells of the myometrium and commonly affect women of reproductive age1), (4. There are many risk factors associated with fibroids like black race, increased estrogen exposure, obesity, alcohol consumption, vitamin D deficiency, diets high in red meat, hypertension, and underlying genetic predispositions5. Patients can be asymptomatic or may present with abnormal uterine bleeding, abdominal pain and pressure symptoms, depending on the number, size, and location of the tumors. Acute complications of uterine leiomyomas requiring surgical intervention are exceptionally rare6.
Treatment includes expectant management, medical and surgical approaches, including Gonadotropin releasing hormone analogues, myomectomy, hysterectomy and uterine artery embolization4.
The authors report an hemoperitoneum with active extravasation from a surface vessel of a leiomyoma on a 46-year-old woman that required prompt intervention.
Case report
A 46-year-old nulliparous Caucasian woman presented in the emergency department with acute abdominal pain. Her past medical and surgical history was unremarkable and she was not under any medication or contraception. Abdominal pain began, suddenly, about 2-3 hours before observation, associated with nausea and vomiting. On our examination, the patient looked pale, hemodynamically stable (blood pressure 103/49 mmHg, heart rate 89 bpm) and abdomen showed mild tenderness. Gynecological exam exhibited an enlarged uterus.
At admission, patient’s hemoglobin was 9,9 g/dL (reference values 12-15 mg/dL) and serum beta human chorionic gonadotropin was negative.
It was decided to perform a transvaginal ultrasound that revealed an enlarged retroverted uterus, with a subserous posterior leiomyoma (FIGO type 6) of homogeneous echogenicity of roughly 97 x 68 x 52 mm, with no pelvic free fluid.
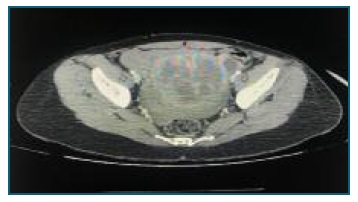
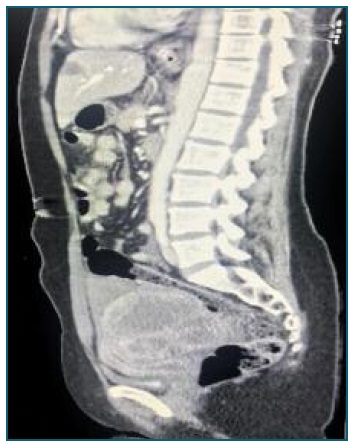
She was then submitted to an abdominal and pelvic CT scan. The exam exposed a large hemoperitoneum and a bulky pelvic mass protruding from the posterior uterine wall with 87 x 76 mm, with active bleeding of unknown origin (Figure 1 and 2).
During the administration of analgesic therapy, the patient started experiencing symptoms and signs of hypovolemic shock (dizziness, paleness, tachycardia and hypotension). Arterial blood sampling revealed a hemoglobin of 8,9 g/dL.
Thus, it was decided to perform an emergent exploratory laparotomy. During laparotomy,surgical team found a large hemoperitoneum (approximately 2 liters) and an enlarged uterus, deformed by a posterior intramural and subserous fibroid of 10 cm with an actively hemorrhaging superficial vein with blood filling the rectouterine pouch. Necrosis or degenerescence of fibroid was not visualized. Adnexa were macroscopically normal. It was tried to control active hemorrhage from the vessel, without success. As patient had no desire of future pregnancy, a total abdominal hysterectomy with ovarian preservation was executed (Figure 3 and 4).

Figure 3 Exploratory laparotomy shows a large uterine leiomyoma originating from the posterior uterine wall.

Figure 4 Following surgical excision, a uterine leiomyoma is shown with overlying congested blood vessels.
Following the surgery, the patient was transferred to the recovery unit in stable condition and was transfused two units of packed red blood cells on the first post-operative day. The patient had an uncomplicated postoperative course and was discharged home three days after the surgery with no furthert complications.
Histological examination of the surgical specimen revealed a leiomyoma.
Discussion
Uterine leiomyomas are the most common pelvic tumors in females and originate from smooth muscle. They constitute a usual cause of hysterectomy1. Rarely, acute complications may arise and include urinary retention with possible renal failure and torsion or avulsion of a pedunculated leiomyoma7. Hemoperitoneum due to rupture of a leiomyoma is an extremely rare complication. To date, there have been less than 100 cases of hemoperitoneum resulting from leiomyomas reported in literature3 and less than 30 of these cases resulted from rupture of a superficial vessel8), (10.
There have been several hypothesis regarding the reasons for spontaneous vascular rupture: fibroids greater than 10 cm in diameter might be associated with stretching of the overlying vessels resulting in rupture; vessels within the leiomyoma might rupture due to the tumor growth or rupture of superficial vessels overlying the uterine leiomyoma can occur due to passive venous congestion associated with increased abdominal pressure (resulting from menstruation or vigorous exercise) (9. The authors did not identify any of these risk factors on our patient, supporting this was a case of spontaneous hemorrhage.
Prompt diagnosis and management are required as this can be a life-threatening condition. This requires a detailed clinical history, excluding pregnancy. Imaging with ultrasound and CT scan are good allies in making the diagnosis. In this case, contrast enhanced CT was chosen because of its high sensibility for pelvic and abdominal etiologies of hemoperitoneum and acute abdomen. Early suspicion and prompt surgical intervention is recommended to resuscitate and control bleeding, minimizing patient morbidity.