Introduction
Breast sarcoma is a severe malignancy of parenchymal origin, which represents less than 1% of all breast malignancies1), (2), (3. Given the rarity of primary angiosarcoma, risk factors are difficult to determine. However, there is an established association between secondary angiosarcoma and previous radiation therapy to the breast or the chest wall, or chronic lymphedema of the upper limbs (Stewart-Treves Syndrome) (1), (2), (3), (4), (5), (6. The widespread adoption of breast-conserving surgery and adjuvant radiotherapy in the management of primary breast cancer has been accompanied by a steady increase in the incidence of secondary breast angiosarcomas2)-(4. Nowadays it is considered a late complication of radiation treatment with a cumulative incidence of 0,9/1000 cases in 15 years5. In opposite to other breast sarcomas, secondary breast angiosarcoma is usually found in older women (60/70 years of age) (3), (4. The median latency period between radiation for breast cancer and subsequent diagnosis is about six years, but the risk remains for, at least, 20 years2), (3), (5. It is not known how new radiotherapy techniques, such as the delivery of intensity-modulated radiation therapy (IMRT), may influence the risk of secondary angiosarcoma. In 1948 Cahan presented the criteria to define a radiation induced lesion: previous radiation exposition of the area, long latency period between radiation exposure and lesion manifestation, different histology between the new lesion and the primary malignancy that elicited the treatment. (7 Since there is a rapid local progression of the disease and a high risk of distant metastasis, the prognosis is poor3), (4.
We report a case of a high grade angiosarcoma diagnosed nine years after a breast invasive carcinoma treated with breast-conserving surgery and radiotherapy.
Case report
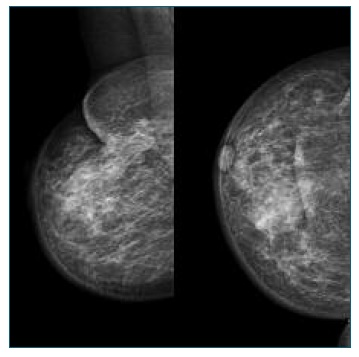
A 69 year-old woman with a previous breast-conserving surgery followed by radiation therapy after an invasive ductal carcinoma on the right breast was referred to our department with a lump at the previous surgery scar. The mammogram showed a high density area, which was biopsied and did not reveal malignancy (Figure 1). On Magnetic Resonance Imaging (MRI) there was a regular mass with 4,5 cm, involving the skin but far from the underlying muscle (Figure 2). The biopsy revealed a high grade angiosarcoma. Axillary or distant metastasis were not detected. After discussion in a multidisciplinary set, a mastectomy with excision of the affected skin was performed with immediate reconstruction. The sentinel node biopsy was negative (OSNA® assay). Pathology confirmed the high grade angiosarcoma, with negative surgical margins. Nine months later, the patient presented with back and abdominal pain associated with asthenia. The abdominal computed tomography scan (CT) revealed multiple nodular hepatic and splenic lesions. The bone scintigraphy showed multiple lytic lesions consistent with malignancy located in D7-L1, left humerus head and third and fourth ribs on the left. Due to the extensive metastization, the patient was referred to palliation and died two months later.
Discussion
Breast angiosarcoma usually presents as single or multiple ecchymotic macular or purplish macular cutaneous lesion in the breast or an edematous upper extremity3), (5. Findings on mammography are frequently nonspecific and unsuspicious3), (4), (8), (9. MRI enables the diagnosis suspicion and provides information on the extent of disease, including the involvement of the skin and the deep fascia and pectoralis muscle4), (8. If a patient with previous history of breast malignancy presents with a palpable mass on the breast or a skin lesion, a biopsy should be pursued, despite inconclusive imaging findings3), (8.
Even though regional lymph node metastasis are more common with angiosarcoma than with other sarcomas, the incidence is still low8. Yet, searching for axillary involvement is still recommended. All patients should be evaluated for spread of metastatic disease, particularly in bones, lungs and liver. CT of the chest and the abdomen, as well as a bone scintigraphy are recommended4.
Since angiosarcoma is a rare presentation of breast malignancy, treatment options arise from small retrospective and non-randomized studies. The first approach entails a multidisciplinary discussion. Surgery seems to be the only potentially curative option and adequate resection margins (at least 2-4 cm) is the single most important determinant of long-term survival with breast sarcomas3), (8. Since angiosarcomas are usually large and extensive, mastectomy is considered the standard approach. However, even with complete ressections with negative margins (R0), the recurrence risk is not negligible9. With respect to axillary involvement, biopsy of the sentinel node is suggested when the axillary investigation is negative. There are no validated conclusions on adjuvant and neo-adjuvant therapies, specially when dealing with radiation-induced malignancies1), (3. The decision should be customized depending on patient status and the risk/benefit balance of the treatment.
Angiosarcomas apparently behave more severely than other breast sarcomas2), (3), (9. The size of the tumor and the histologic stage seem to be the most important prognostic determinants8), (9. Since high grade angiosarcomas with high risk of local and distant metastatic spreading and high recurrence rate are the most common presentation, prognosis is usually poor. The over-all survival after surgical treatment in patients with no metastasis is about four years1)-(2.
In conclusion, even though the risk of developing a secondary angiosarcoma after radiation therapy might increase with the widening of breast-conserving surgery, the potential benefit of radiation therapy is, for now, frankly higher than the residual risk of developing a treatment-related angiosarcoma. In patients with previous radiation therapy there should be a close follow-up of new symptoms and findings , even if not suspicious of malignancy. An early diagnosis might lead to a better prognosis. Once again, the small number of cases reported and the scarce clinical evidence enhance the challenging approach to diagnosis and treatment of angiosarcoma.