Introduction
Fetal arrhythmias can occur in about 1% of every pregnancy1,2. A fetal heart rate that is sustained and superior to 180 beats per minute (bpm) is classified as fetal tachycardia2. These fetal tachyarrhythmias can present as cardiac failure, hydrops fetalis and eventually fetal demise, even in a fetus with a structurally normal heart1,2,3,4. The most common fetal tachyarrhytmia detected prenatally is supraventricular tachycardia (SVT) (4. Atrioventricular reentry tachycardia (AVRT) is the most common etiology of fetal SVT, with atrial flutter (AF) being the second4. In uterus, the diagnosis of these disturbances presents a challenge, since it is done through fetal echocardiography. The use of M-mode echocardiography (and pulsed Doppler) presents a valuable diagnostic tool since it can identify the temporal relation between the contraction of the atria and the ventricles in the fetus5. This allows for the differential diagnosis between AVRT and AF. The distinction between the two might be tricky but usually, in AVRT, atrioventricular conduction is usually 1:1 whereas AF presents with a 2:1 or 3:1 conduction5,6.
Historically, digoxin and amiodarone were the most commonly used drugs in the therapy of SVT. However, rates of conversion to sinus rhythm with these drugs were lower, and time to conversion to sinus rhythm longer, especially in the presence of hydrops fetalis, likely due to poor tissue penetration in the pre-sence of edema4,6.
Nowadays, the use of flecainide in the treatment of fetal tachyarrhythmias is well established and this drug is now used as first line therapy in many centers1,2,4,7. Despite this, there is still some controversy, due to the lack of randomized studies and specific guidelines4. We describe three cases of fetal tachyarrhythmias successfully treated with flecainide without any side effects and fast conversion to sinus rhythm.
Clinical cases
Case 1: A 34 year old, primigravida, presented to the emergency department at 30 weeks of gestational age due maternal perception of reduced fetal movements. An emergency fetal ultrasound revealed hydrops fetalis (pleural effusion and ascites) (Figure 1) as well as a sustained fetal heart rate of 300bpm (Figure 2 (A)). Fetal echocardiography was performed and the diagnosis of fetal SVT was made. No structural anomalies were detected. The gravida’s electrocardiogram (ECG) was normal and she was started on oral flecainide (100mgs tds). The fetus’ rhythm was reevaluated in 48 hours with conversion to sinus rhythm (Figure 2 (B)). The mother’s ECG was unaffected. After 6 days of treatment hydrops fetalis reverted, and sinus rhythm was maintained until delivery, with weekly fetal and maternal reevaluations. No maternal side-effects were noted. Spontaneous labour occurred at 40 weeks. The newborn was asymptomatic, in sinus rhythm, and was started on flecainide. Currently, at 16 months of age he remains in sinus rhythm, asymptomatic, with no medication.
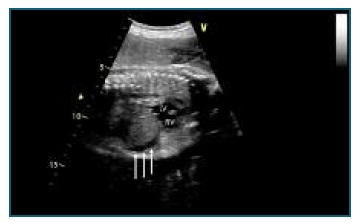
Figure 1 Case 1 - Fetal echocardiogram, sagittal view, demonstrating ascites (white arrows). RV - right ventricle; LV - left ventricle.

Figure 2 Case 1 - Fetal echocardiogram and pulsed Doppler traces demonstrating fetal supraventricular tachycardia before (A) and after (B) treatment with flecainide.
Case 2: A 40 year old, gravida 4, para 0, presented to the emergency department of a secondary care hospital, due to vaginal bleeding. Fetal echography diagnosed SVT at 250bpm. No other abnormalities were noted. The gravida’s ECG was normal, and, under the advice of the pediatric cardiology department she was started on oral flecainide (100mg tds). Fetal echocardiography 24 hours after the beginning of flecainide (2 doses) showed sinus rhythm (fetal heart rate of 130bpm). Sinus rhythm was maintained until delivery, with no adverse side effects related to flecainide therapy either in the fetus or in the mother. Spontaneous uncomplicated labour occurred at 39 weeks. The newborn was asymptomatic, in sinus rhythm, and was started on flecainide. Currently, at 14 months of age he presents no symptoms and remains in sinus rhythm, with no medical therapy.
Case 3: A 36 year old, gravida 2, para 1, is referred for evaluation by pediatric cardiology due to suspected aortic coarctation in the fetus (ventricular and great arteries size disproportion) at 19 weeks’ gestation. Revaluation at 33 weeks revealed a SVT with 2:1 AV conduction, ventricular rate of 160bpm - possible AF (Figure 3, Figure 5 (A)). Treatment with sotalol 80mg tds was started and revaluation performed after 48 hours of therapy. The fetus remained in sustained AF and the sotalol dose was doubled. After 10 days of the-rapy, the flutter was deemed refractory to the initial medical therapy and sotalol was stopped. Combination therapy with flecainide 100mg tds and digoxin 0,25mg tds was started instead. After 48 hours the fetus was found to be in sinus rhythm (Figure 4, Figure 5 (B)), which was sustained until the birth, at 38 weeks. The newborn underwent neonatal aortic coarctation surgical correction, which was uneventful. He has been in sinus rhythm since birth until now, at 13 months of age, without any medication.
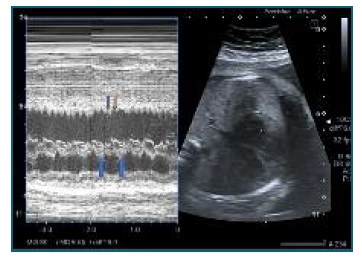
Figure 3 Case 3 - Fetal echocardiogram detailing the fetal supraventricular tachyarrhythmia. M mode documentation of an atrioventricular conduction of 2:1, with a ventricular rate of 170 bpm (blue arrows); atrial contraction with an atrial rate of 340bpm (orange arrows).

Figure 4 Case 3: Fetal echocardiogram with M mode demonstrating conversion to sinus rhythm after flecainide + digoxin therapy. There is now an atrioventricular conduction rate of 1:1, with a ventricular rate of 127 bpm. Atrial contraction (orangearrows); Ventricular contraction (blue arrows).
Discussion
SVT treatment with flecainide presented a paradigm shift, as it provided a fast and safe therapeutic option, even in the presence of hydrops fetalis2,6. Several authors advocate the use of flecainide as first-line treatment for fetal tachyarrhytmias1,2,4,7.
In the article by Strizek et al, a rate of conversion to sinus rhythm of 81,2% was achieved using flecainide in monotherapy4. Similarly, Vigneswaran et al and Ekiz et al, reported conversion to sinus rhythm in 88.2% and 78% of cases treated with flecainide as a first-line drug, respectively. In all studies the mean time of conversion to sinus rhythm was 3 days2,4,7. These finding are consistent with the cases described, where conversion to sinus rhythm occurred under 48 hours after treatment was started. The most common side-effects of flecainide therapy include nausea, vomiting, dizziness, headaches and ECG changes - prolonged PR interval and widened QRS complexes1,6. In our practice we follow a standardized protocol: after diagnosis of fetal SVT the mother is started on 100mg tds if her baseline ECG is normal. We perform weekly revaluations with fetal echocardiogram and maternal ECG. After delivery the baby is treated with flecainide until 12 months of age, when, if he’s asymptomatic and 24 hour Holter monitoring is normal, therapy is discontinued. Fetal AF does not usually require treatment in the neonatal period.
In our experience, flecainide presents as an effective, fast-acting and safe first-line therapy for the treatment of fetal SVT, even in the hydropic fetuses.
Author contributions
Conceptualization M.L., J.R., G.S., A.T.; formal analysis M.L., R.A.; resources A.T., M.L.; writing-original draft preparation, M.L., A.T.; writing-review and editing, J.R., G.S., R.A.; design and figures, M.L., A.T.; supervision, A.T., R.A.;
All patients gave their express consent authorizing the publication of theirs and their children’s medical data.















