Original Study/Estudo Original
Association between corpus luteum volume and the success of termination of pregnancy with mifepristone
Associação entre o volume do corpo lúteo e o sucesso da interrupção da gravidez com mifepristona
1.Departamento de Obstetrícia, Ginecologia e Medicina da Reprodução, Hospital de Santa Maria, Centro Hospitalar Universitário Lisboa Norte, Portugal.
Abstract
Background:
Mifepristone is a progesterone antagonist often used in medical termination of pregnancy. One of its targets is the corpus luteum, the main source of progesterone in initial pregnancy maintenance. Corpus luteum volume is related to serum progesterone levels.
Objective:
This study intended to evaluate whether there is an association between corpus luteum volume and the success rate of pharmacological termination of pregnancy with mifepristone and misoprostol.
Methods:
This was a prospective, longitudinal, observational study. 176 women deciding to terminate their pregnancy were included. At the first medical visit we confirmed the presence of a viable pregnancy with less than 10 weeks and estimated corpus luteum volume by transvaginal ultrasound. Medical termination of pregnancy protocol in our hospital consisted of oral mifepristone 200 mg followed (24 hours) by oral misoprostol 200 µg one pill every hour until a maximum of eight doses. At the reevaluation visit, we registered clinical data and confirmed the success of the procedure by vaginal ultrasound.
Results:
The success rate of medical termination of pregnancy was 95.5%. No differences regarding corpus luteum volume were observed between successful and unsuccessful termination of pregnancy groups.
Conclusion:
In our sample there was no association between corpus luteum volume and the success rate of medical termination of pregnancy.
Keywords: Corpus luteum; Medical termination of pregnancy; Mifepristone; Progesterone; Ultrasound
Resumo
Introdução:
A mifepristona é um antagonista da progesterona frequentemente utilizado na interrupção médica da gravidez. Um dos seus alvos é o corpo lúteo, a principal fonte de progesterona na manutenção da gravidez inicial. O volume do corpo lúteo relaciona-se com os níveis séricos de progesterona.
Objetivo:
Este estudo teve como objetivo avaliar a existência de associação entre o volume do corpo lúteo e a taxa de sucesso da interrupção farmacológica da gravidez com mifepristona e misoprostol.
Métodos:
Este foi um estudo prospetivo, longitudinal e observacional. Foram incluídas 176 mulheres com intenção de interromper a gravidez. Na primeira consulta médica foi confirmada a presença de uma gravidez viável com menos de 10 semanas e estimado o volume do corpo lúteo por ecografia transvaginal. O protocolo de interrupção médica da gravidez no nosso hospital consistiu na administração de mifepristona oral 200 mg seguida (24 horas) de misoprostol oral 200 µg um comprimido a cada hora até ao máximo de oito doses. Na consulta de reavaliação foram registados dados clínicos e confirmado o sucesso do procedimento por ecografia vaginal.
Resultados:
A taxa de sucesso da interrupção médica da gravidez foi de 95,5%. Não foram observadas diferenças no volume do corpo lúteo entre os grupos de sucesso e insucesso da interrupção da gravidez.
Conclusão:
Nesta amostra no houve associação entre o volume do corpo lúteo e a taxa de sucesso da interrupção médica da gravidez.
Palavras-chave: Corpo lúteo; Interrupção médica da gravidez; Mifepristona; Progesterona; Ecografia
Introduction
Mifepristone is a synthetic steroid with a high affinity for progesterone receptors, competing for binding in the endometrium and decidua1-3. Owing to its antiprogestin properties, it has been used in clinical practice with the prostaglandin analog misoprostol for medical termination of pregnancy3. The combination of these two drugs generally results in a complete abortion rate of 92-99%4,5.
The corpus luteum, formed from the regressing ovarian dominant follicle, is an active endocrine gland, the primary function of which is the secretion of progesterone, required for the initial maintenance of a normal pregnancy3.
If implantation occurs, regression of the corpus luteum is delayed and luteal function is maintained until progesterone secretion is taken over by the developing placenta6. This change in progesterone synthesis and secretion is called luteoplacental shift and, in humans, it takes place at 7-8 weeks of pregnancy3. It is known that lutectomy before the 7th week of gestation results in miscarriage7.
It has been hypothesized that progesterone might have an autocrine or paracrine role in regulating corpus luteum function6. As such, in addition to trophoblastic tissue, the corpus luteum is also the target organ of mifepristone3. Due to the luteoplacental shift, the effect that mifepristone has on the corpus luteum decreases with advanced gestational age3.
It has been demonstrated that after the administration of mifepristone there is a decline in the volume of the ovary carrying the corpus luteum3. Also, studies have suggested that blockage of progesterone action using mifepristone could enhance apoptosis in the corpus luteum8,9.
The corpus luteum relative size, as assessed by ultrasound, may be a surrogate marker of endocrine activity because it correlates with serum progesterone levels10-12.
Finally, although medical termination of pregnancy has a small failure rate13, it is still important to identify potential causes and understand if some women would benefit from a different approach.
This study intended to evaluate whether there is an association between corpus luteum volume and the success rate of pharmacological termination of pregnancy with mifepristone and misoprostol.
Methods
This prospective observational study was carried out in the Department of Obstetrics, Gynecology and Reproductive Medicine of a tertiary hospital between September 2018 and December 2019, with the approval of the ethics committee.
The inclusion criteria were: women aged ≥ 18 years, able to give written consent and who intended to undergo a voluntary medical abortion.
Women with no identifiable corpus luteum by ultrasound were excluded.
Written informed consent was obtained from all patients.
Our hospital’s abortion protocol entails four different medical visits. The first step of the process is to perform an ultrasound evaluation to check pregnancy location, viability, and calculate gestational age through the crown-rump length. If there is a viable intrauterine pregnancy with less than 10 weeks and 3 days, the abortion is legally possible in our hospital. After clarification about the procedure, the patient is obliged to a three days reflection period before the final decision of pregnancy termination. Abortive medication is given to the patient - oral mifepristone 200 mg followed (24 hours) by oral misoprostol 200 µg, one pill every hour until a maximum of eight doses. About one week later, there is a clinical and ultrasound follow up to confirm the success (absence of gestational sac). During the process the women have access to contraceptive counselling.
The recruitment for this study took place after ultrasound confirmation of a viable pregnancy that fulfills previously mentioned ultrasound criteria to terminate the pregnancy. Every ultrasound was performed transvaginally by the same operator. We located the corpus luteum, applied color Doppler to identify its characteristic peripheral ring of vascularity, measured it in three orthogonal planes and calculated its volume through Astraia® software.
We collected patients’ general and clinical data by interview, including age, height, weight and obstetric history. The presence or absence of an intrauterine gestational sac was documented by ultrasound.
The primary outcome was unsuccessful termination of pregnancy, defined as the visualization of an intrauterine gestational at the re-evaluation visit.
We divided the sample into two groups - successful and unsuccessful termination of pregnancy - to compare its characteristics.
We performed descriptive and analytical statistics, using Student’s t-tests to compare means between successful and unsuccessful termination of pregnancy groups. P value < .05 was considered statistically significant.
Results
A total of 200 women were recruited, but only 176 were included in the analysis. Between the excluded, 20 decided not to terminate their pregnancy, and 4 had no record of the corpus luteum volume. The follow up rate was 100%.
In our sample of 176 medical abortions, a total of 8 (4.5%) were unsuccessful, which means the success rate was 95.5%.
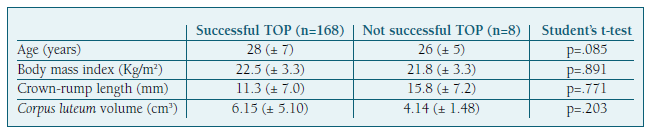
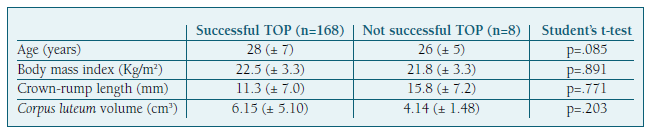
There were no statistically significant differences between the two groups regarding any of the variables studied, including the corpus luteum volume (Table I).
Table I Comparison between the two study groups.
Discussion
Progesterone secretion by the corpus luteum is very important for initial pregnancy maintenance. As such, pharmacological termination of pregnancy with mifepristone, a progesterone antagonist, is very common in clinical practice, with high success rates.
Corpus luteum size can be accurately measured by ultrasound, and although its meaning remains controversial14, it has been hypothesized that ultrasound parameters of the corpus luteum may be associated with its endocrine function15.
To our knowledge, this is the first study evaluating the association between corpus luteum volume, measured by ultrasound, and the success rate of initial pregnancy termination with mifepristone and misoprostol.
Medical termination of pregnancy with mifepristone and misoprostol in our sample had a success rate of 95.5%, similar to that described in the literature4,5,13.
Although we did not find a significant difference in the corpus luteum volume between successful and unsuccessful termination of pregnancy groups, our sample was not large enough to detect such a difference, due to the high success rate of this procedure.
For instance, if there is a true difference in the corpus luteum volume between the groups at the absolute values shown in this study, a total sample size of 1226 cases (with 53 unsuccessful cases) would have to be studied for such a difference to be found (alpha .05 and power 80%).
The main strengths of our study are its prospective nature and high follow up rate.
Besides the already mentioned sample size, the gestational age may also influence the results, because we included pregnancies until 10 weeks and 3 days, but the luteoplacental shift in progesterone secretion during pregnancy occurs around the 7-8th week3.
In conclusion, we did not find an association between corpus luteum volume and the success of termination of pregnancy with mifepristone, but our results can be used as preliminary data for future research in this area.
Authors’ contribution
Conceptualization: Susana Rego, Catarina Reis-de-Carvalho, Rui Carvalho
Methodology: Susana Rego, Joaquim Neves
Formal analysis: Susana Rego
Writing - Original Draft: Susana Rego
Writing - Review: Catarina Reis-de-Carvalho, Rui Carvalho
Conflicts of interest
The authors declare that they have no conflict of interest.
References
1. Say L, Brahmi D, Kulier R, Campana A, Gülmezoglu AM. Medical versus surgical methods for first trimester termination of pregnancy. Cochrane Database Syst Rev. 2002;(4). DOI: https://doi.org/ https://doi.org/10.1002/14651858.cd003037.pub2
[ Links ]
2. Moreno-Ruiz NL, Borgatta L, Yanow S, Kapp N, Wiebe ER, Winikoff B. Alternatives to mifepristone for early medical abortion. Int J Gynecol Obstet. 2007;96(3):212-218. DOI: https://doi.org/10.1016/j.ijgo.2006.09.009
[ Links ]
3. Aki MN, Tapanainen JS, Arvel IYJ. Effect of mifepristone on the corpus luteum in early pregnancy. 2009;(February):448-453. DOI: https://doi.org/10.1002/uog.6418
[ Links ]
4. Kahn JG, Becker BJ, MacIsaa L, Amory JK, Neuhaus J, Olkin I, Creinin MD. The efficacy of medical abortion: A meta-analysis. Contraception. 2000;61(1):29-40. DOI: https://doi.org/10.1016/S0010-7824(99)00115-8
[ Links ]
5. Jiang W, He F, Shen Q, Tao X, Zhao C, Shen Z, Zhu X. ScienceDirect Factors related to completeness of medical abortion with mifepristone and misoprostol. J Chinese Med Assoc. Published online 2016:1-7. DOI: https://doi.org/10.1016/j.jcma.2016.03.011
[ Links ]
6. Stouffer RL. Progesterone as a mediator of gonadotrophin action in the corpus luteum: Beyond steroidogenesis. Hum Reprod Update. 2003;9(2):99-117. DOI: https://doi.org/10.1093/humupd/dmg016
[ Links ]
7. Csapo AI, Pulkkinen MO, Ruttner B, Sauvage JP, Wiest WG. The significance of the human corpus luteum in pregnancy maintenance. I. Preliminary studies. Am J Obstet Gynecol. 1972;112(8):1061-1067. DOI: https://doi.org/10.1016/0002-9378(72)90181-0
[ Links ]
8. Makrigiannakis A, Coukos G, Christofidou-Solomidou M, Montas S, Coutifaris C. Progesterone Is an Autocrine/Paracrine Regulator of Human Granulosa Cell Survival in Vitro. Ann N Y Acad Sci. 2006;900(1):16-25. DOI: https://doi.org/10.1111/j.1749-6632.2000.tb06212.x
[ Links ]
9. Svensson EC, Markström E, Shao R, Andersson M, Billig H. Progesterone receptor antagonists Org 31710 and RU 486 increase apoptosis in human periovulatory granulosa cells. Fertil Steril. 2001;76(6):1225-1231. DOI: https://doi.org/10.1016/S0015-0282(01)02891-6
[ Links ]
10. Baerwald AR, Adams GP, Pierson RA. Form and function of the corpus luteum during the human menstrual cycle. Ultrasound Obstet Gynecol. 2005;25(5):498-507. DOI: https://doi.org/10.1002/uog.1891
[ Links ]
11. Griffin PG, Ginther OJ. Research applications of ultrasonic imaging in reproductive biology. J Anim Sci. 1992;70(3):953-972. DOI: https://doi.org/10.2527/1992.703953x
[ Links ]
12. Miyamoto A, Shirasuna K, Hayashi KG, Kamada D, Kawashima C, Kaneko E, Acosta TJ, Matsui M. A potential use of color ultrasound as a tool for reproductive management: New observations using color ultrasound scanning that were not possible with imaging only in black and white. J Reprod Dev. 2006;52(1):153-160. DOI: https://doi.org/10.1262/jrd.17087
[ Links ]
13. Hsia JK, Lohr PA, Taylor J, Creinin MD. Medical abortion with mifepristone and vaginal misoprostol between 64 and 70 days' gestation. Contraception. 2019;100(3):178-181. DOI: https://doi.org/10.1016/j.contraception.2019.05.006
[ Links ]
14. Doppler U. Características ecográficas do corpo lúteo em gestações iniciais : morfologia e vascularização. Published online 2010.
[ Links ]
15. Valentin L. Imaging in gynecology. Best Pract Res Clin Obstet Gynaecol. 2006;20(6):881-906. DOI: https://doi.org/10.1016/j.bpobgyn.2006.06.001
[ Links ]