Introduction
Non-Hodgkin’s lymphomas (NHL) are predominantly lymphatic organs neoplasms; however, they may arise in solid organs in 25-35% of cases1,2. Extranodal non-Hodgkin’s lymphomas often involve the gastrointestinal tract and central nervous system but may also affect other sites, such as the adrenal glands, breast, thyroid, bone, prostate and female genital tract1,3,4.
Primary involvement of the female gynecological tract is uncommon1,3,5,6,7. Clinical manifestations of gynecological tract lymphomas are nonspecific and may mimic the presentation of other gynecological neoplasms and include symptoms such as vaginal bleeding, abnormal discharges, abdominal distension, among others3,6,7.
We present three clinical cases of female genital tract lymphomas, in multiparous and post-menopausal women, whose first sign was abnormal uterine bleeding, a clinical presentation similar to other gynecological neoplasms.
Clinical cases
Case I
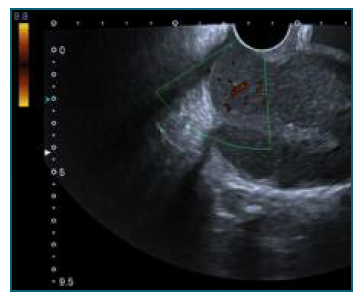
76 years old, obstetric index 3003, menopause at 58 years old, with history of arterial hypertension, obesity, type 2 diabetes mellitus, dyslipidemia, and pacemaker. She was admitted to the emergency department with complaints of vaginal bleeding since the previous day but was otherwise asymptomatic. Physical examination revealed the presence of abundant clots in the vagina and a very widened cervix was identified. It was not possible to visualize the external cervical os. On bimanual examination, the cervix was very hardened and enlarged. Transvaginal ultrasound showed a heterogeneous uterus, in an indifferent position, measuring 132x67x64 mm, an uterine cervix 49 mm long, widened and highly vascularized, and an endometrial thickening of 11 mm (Figure 1). An uterine curettage was performed and the material was sent for anatomopathological study. The histological examination revealed a non-Hodgkin B lymphoma, CD20+, whose morphology and immunohistochemical profile were compatible with a grade 1-2 follicular lymphoma with low ki67 proliferative index (15%). The patient was referred for a hematology oncology appointment. The additional investigation, which included a thoraco-abdominopelvic CT and positron emitting tomography (PET), showed a large heterogeneous lesion in the cervix with extension to the uterine body, multiple infradiaphragmatic adenopathies and subcutaneous/musculoskeletal and osteomedullary involvement, corresponding to a stage IV-A lymphoma (Ann Arbor classification). After 8 cycles of therapy with rituximab, cyclophosphamide, vincristine, and prednisone (R-CVP), a new PET scan was performed, which showed a complete metabolic response to therapy. The patient will start a 2 year maintenance immuno-chemotherapy with anti-CD20 antibody.
Case II
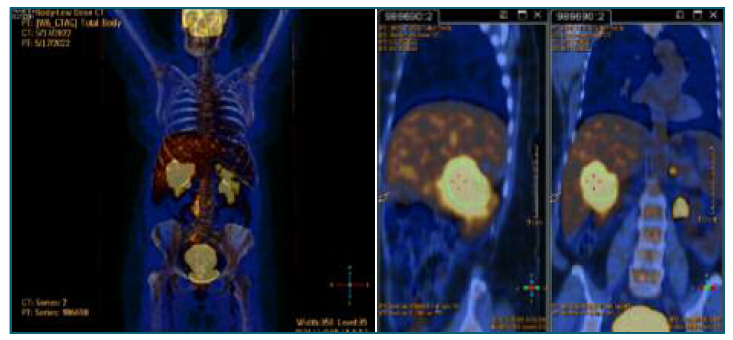
69 years old, obstetric index 3003, menopause at 51 years old, with a history of arterial hypertension. The patient was referred to the endometrial pathology appointment due to abnormal postmenopausal uterine bleeding and endometrial thickening of 7 mm associated with a 15 Kg weight loss in the last few months. The gynecological examination was unremarkable. The hysteroscopy revealed an intracavitary neoformation with suspicious vascularization, which was biopsied; the specimen was sent for anatomopathological study, which revealed a high-grade CD20+ non-Hodgkin B lymphoma, whose morphology and immunohistochemical profile were compatible with diffuse large B cell lymphoma, molecular subtype ABC (Hans algorithm); high ki67 proliferative index (about 80%). The patient was referred to the oncological hematology appointment. Complementary diagnostic tests (thoraco-abdominopelvic CT and PET) detected a lesion in the right kidney with hepatic, left adrenal and uterine infiltration, suggesting lymphoproliferative involvement in these locations - stage IV-B in the Ann Arbor classification (Figure 2). 6 cycles of therapy with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP) have been completed. The patient has a thoraco-abdominopelvic CT reevaluation scheduled.
Case III
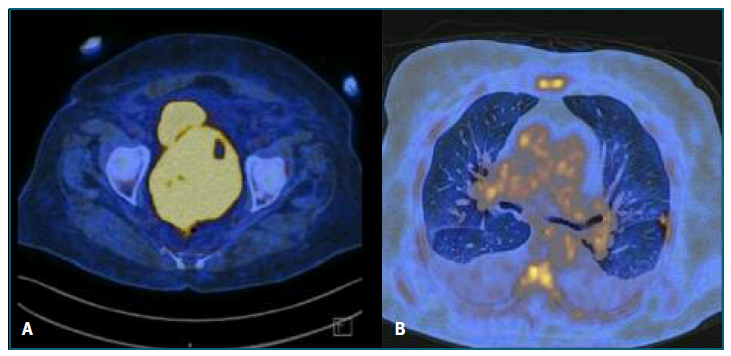
88 years old, obstetric index 3003, menopause at 58 years old, with a history of arterial hypertension, obesity, type 2 diabetes mellitus, dyslipidemia, and asthma. She was admitted to the emergency department with a 2 week vaginal blood loss. Physical examination revealed moderate quantity of blood in the vagina; an enlarged, globular, and hard elastic cervix, with exuberant vessels, one of which was bleeding; abdominal distention was also observed. Transvaginal ultrasound showed an anteverted uterus, increased in volume, with a well-defined vascularized mass in the isthmic region, measuring 6x4 cm. The endometrium was distorted, irregular with a thickness of about 8 mm. An uterine cervix biopsy was performed, revealing a high-grade CD20+ Non-Hodgkin B Lymphoma, with morphology and immunohistochemical profile compatible with diffuse large B cell lymphoma, molecular subtype GCB (Hans algorithm); high ki67 proliferative index (upper 80%). The patient was referred for a hematology oncology appointment. One week after the diagnosis, the patient was hospitalized for a new episode of abundant vaginal blood loss, requiring transfusional support (2 units of red blood cells). In an additional imaging study (PET), there was a large mass centered in the cervix region, with approximately 113x94 mm, multiple focal areas distributed throughout the uterine body and several nodular lesions in both lungs, suggestive of lymphomatous lesions - stage IV-A in the Ann Arbor classification (Figure 3). A combined chemoimmuno-therapy regimen was instituted, with rituximab, cyclo-phosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP). Were completed 6 cycles, with no fur-ther evidence of blood loss and good clinical response after 9 months of follow-up.
Discussion
The incidence of extranodal non-Hodgkin lymphomas, including those of the gynecological tract, has increased in recent decades6-8.
Non-Hodgkin’s lymphomas presentation varies according to the lymphoma’s type and the involvement of different areas. Involvement of the female genital tract can occur in three ways: incidental involvement in the context of generalized lymphoma (the most common), presentation of a previously unknown disseminated lymphoma, and, more rarely, as a primary lymphoma of the female genital organs9. Clinical presentation of these lymphomas is nonspecific, and may include vaginal blood loss, abnormal discharges, abdominal distension, among other symptoms3,6,7. B-symptoms like fever, night sweats, weight loss, and fatigue, which appear in more aggressive non-Hodgkin’s lymphomas are uncommon in extranodal lym-phomas5,10. All the cases described presented themselves in a similar way to other gynecological neoplasms, with the presence of B symptoms in only one of them10. So it is important to be aware of this disease and include it in the differential diagnosis of other gynecological neoplasms since their follow-up and treatment are conducted differently10.
Female genital tract lymphomas usually occur during the fifth decade of life; however, it depends on the histological subtype. The diffuse large B-cell lymphoma is more common between 35 and 45 years old, whereas follicular lymphoma is more frequent in people aged over 50. The Burkitt lymphoma affects children from five to ten years old7-9.
The definitive diagnosis is confirmed by pathological examination of the specimen. The immunohistochemical study has acquired a fundamental role in the characterization of antibodies and in the classification of the various subtypes1,3,7,9. The main histological subtype of non-Hodgkin’s lymphoma corresponds to diffuse large B-cell lymphoma, followed by follicular lymphoma, and at last by Burkitt’s lymphoma1,7,10,11.
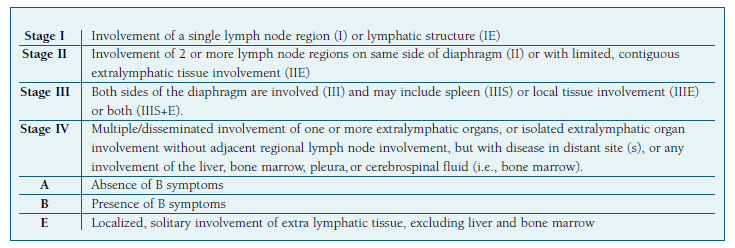
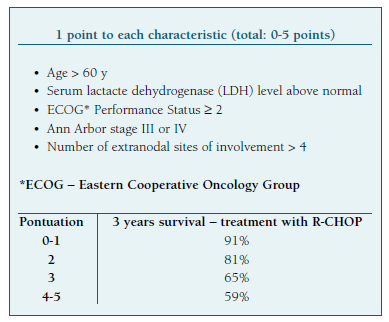
The prognosis is based on the Ann Arbor staging system (Table I), size and disease extension, age, number of nodes affected, LDH level and lymphomas grade - features included on the international prognosis index on Non-Hodgkin’s lymphomas (IPI) (Table II) 3,5,6,7,9. Immunohistochemical analysis also plays an important role as several biomarkers have been shown to be important in determining the behavior of diffuse large B-cell lymphomas3. It has been shown that high Ki-67 proliferation indexes are associated with poor prognosis3.
Genital tract lymphomas should be managed by multidisciplinary teams and individualized to each patient specificities7. Once the diagnosis is confirmed, a standard chemotherapy regimen for non-Hodgkin’s lymphomas is instituted. The most used regimen includes cyclophosphamide, hydroxydaunorubicin (doxorubicin), oncovin (vincristine), and prednisolone or prednisone (CHOP) 7,12. However, other regimens including cyclophosphamide, vincristine and prednisone (CVP) or fludarabine based regimens are also used12. Depending on the histological subtype of the tumor, extent of the disease and patient-related factors, radiotherapy may or may not be associated1,3. Rituximab is a monoclonal antibody that binds to the B-cell surface antigen CD20. It has been shown that this antibody induces apoptosis and sensitize chemo-therapy-resistant human lymphoma cell lines to cytotoxic chemotherapy. Therefore, trials combining rituximab with the standard chemotherapy regimen reported higher response rates compared to the use of chemotherapy regimens alone, showing the synergistic activity of rituximab9,10.
Subsequently, criteria for response to therapy are evaluated with thoraco-abdominopelvic CT and, more recently, PET-CT, being an asset for the follow-up of this pathology9,10. Response to therapy is then evaluated with a thoraco-abdominopelvic CT. More recently, PET-CT has shown to be a valuable asset in the follow-up of this condition as well.
Authors’ contributions
Mariana Solinho - revisão da literatura, colheita de dados clínicos, elaboração e revisão do artigo.
Ana Rolha - colaboração na colheita de dados clínicos e revisão do artigo.
Marta Beja Duarte - revisão do artigo.
Vera Santos Loureiro - revisão do artigo.
Paula Barroso - revisão do artigo.