Introduction
Lipschütz ulcer (LU) was first described in 1912 by Benjamin Lipschütz. It was identified as a rare cause of non-venereal vulvar ulcerations that usually affect young individuals and adolescents with no prior sexual contact1. Today it is known to occur more often in adolescent and young women but can affect individuals of any age group and sexual status2.
There is no consensus about the diagnosis criteria in the literature, and it is believed that this condition is underdiagnosed due to the lack of awareness among healthcare providers2,3.
LU is a non-sexually acquired disease, that manifests as sudden-onset, painful, acute vulvar ulcers, usually preceded by fever, malaise, and other unspecific symptoms like asthenia, headache, myalgias and adenopathy. The ulcers are typically deep and necrotic, wider than 1 cm and appear in a mirror distribution (“kissing lesions”), primarily affecting the middle region of the labia minora. However, assymmetric or unilateral and non-necrotic ulcers have also been described.
Symptomatic treatment options, such as pain relief with acetaminophen or ibuprofen, topical treatment with 2% lidocaine gel or benzocaine, and oral or topical steroid use to reduce inflammation (such as Clobetasol 0,05% ointment or prednisolone 40 mg per os 10 days), are the main options available. The use of colchicine (1 mg per os), pentoxifiline (400 mg per os) or topical silver nitrate for symptoms relief has also been described. The condition is usually self-limited, and relapses are rare1,2.
The mechanism behind the manifestation of LU is still unclear. It is thought to be triggered by an exacerbated immune response to agents such as Epstein-Barr virus (EBV), cytomegalovirus, Mycoplasma pneumoniae and toxoplasma gondii, although it is thought it may be associated with other agents as influenza virus and adenovirus1,3.
It is a diagnosis of exclusion and sexually transmitted infection, Behçet’s syndrome, Crohn’s disease and other specific ulcerative diseases must be ruled out.
We found, in recent literature, four cases of genital ulcers associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. 4,5,6,7 In this report, we present a case of a woman who developed acute-onset, painful vulvar ulcers during concurrent SARS-CoV-2 infection.
Case description
A 34 year old women resorted to emergency room complaining of vulvar pain. She was a non-smoker, with no personal or family history of autoimmune diseases or previous genital ulcer, and no regular use of medication. At the time she had no sexual partner and reported not having sexual intercourse several months prior.
The woman presented with a fever, myalgia and odynophagia and was diagnosed with COVID-19 two days prior of presenting with vulvar pain.
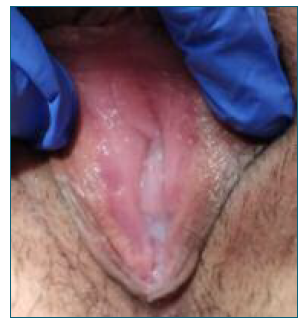
At the observation the patient had deep, bilateral symmetric painful ulcers with a central necrotic area (Figure 1). There were no cervical or vaginal abnormalities, and no ulcers in any other location, including the oral or anal area, and no lymphadenopathies were noted. There was no pathologic discharge.

Figure 1 Vulvar lesions at first examination. We can see symmetric ulcers in the labia minora, with a central necrotic area.
Blood tests showed mild leukocytosis (11800×109/L) and neutrophilia (8600×109/L) and C-reactive protein of 41 mg/L.
She had negative serologic tests for acute infection for Herpes simplex virus (positive immunoglobulin G and negative M (IgG+/IgM-), Treponema pallidum (IgG-/IgM), EBV (IgG+/IgM-) and HIV.
There were no clinic criteria of Behçet’s disease or symptoms related to Crohn’s disease.
Overall, the patient’s clinical presentation, characteristic lesions, negative serologic tests for common infectious causes of genital ulcers, and lack of other signs and symptoms suggestive of underlying autoimmune or inflammatory conditions, led us to conclude that Lipschütz’s ulcers related to COVID-19 was the most probable diagnosis.
Considering the patient’s complaints of pain, we prescribed topical corticosteroid treatment (hydrocortisone 10 mg/g) and lidocaine (gel, 20 mg/g). The topical corticosteroids were administered twice a day, while the lidocaine was used as needed for pain relief. The patient showed significant improvement of the lesions after one week of treatment (Figure 2), with no vulvar pain and complete remission of systemic symptoms associated with COVID-19. The treatment was continued for three weeks until there was complete remission of the ulcers.
Discussion
As described before, there are a few known infecions associated with Lipschütz ulcer and until recently COVID-19 was not one of them. The case report presented is of most importance as it highlights a rare manifestation of COVID-19 that can be easily misdiagnosed, with only four cases reported in the literature, so far. Lipschütz ulcer is a rare cause of vulvar ulcerations, mostly affecting young people and adolescents without prior sexual contact. However, it can manifest in patients of any age group and sexual status.
The presentation of acute vulvar ulcers, associated with fever and malaise, in the absence of sexually transmitted infections and other specific ulcerative diseases, is a hallmark of Lipschütz ulcer.
It is noteworthy that the diagnosis of Lipschütz ulcer is still challenging, and therefore, it is often underdiagnosed. Clinicians must be aware of this pathology, particularly when examining young patients with vulvar pain, and take the necessary steps to exclude other diagnoses.