Introduction
Human papillomavirus (HPV) is the most prevalent sexually transmitted infection, although, regardless of genotype, most infections are transient1. However, persistence of high-risk HPV infection is associated with approximately 90% of cervical cancers (CC)1. Beyond HPV infection, other cofactors are required for the development of invasive disease. It has been described associations with smoking habits, long-term use of hormonal contraceptives, multiparity and immunosuppression2.
Cervical cancer screening (CCS) guidelines were updated in 2017 by the Portuguese Ministry of Health and implemented in 2019 in the Central Region of Portugal. The cytological screening program was replaced by primary HPV testing, which is performed with clinical validated Cobas® HPV test, that detects 14 high risk oncogenic HPV types: HPV 16, HPV 18, and other HR-HPV (31/33/35/39/45/51/52/56/58/59/66/68). The 16/18 genotyping works as a triage test for direct colposcopy and pap cytology as a triage for other 12 HR-HPV types3,4. If reflex pap test has alterations of equal or greater than atypical squamous cells of undetermined significance (ASCUS), it has indication to colposcopy. All women aged 25 to 60 years, are screened every five years3,4.
In 2020, the onset of COVID-19 pandemic led to a reorganization of healthcare, with direct impact on “non-priority” activity, which culminated in the suspension of screenings between March and July, in all Portuguese Regional Health Administrations (RHA). Therefore, compared to 2019, 55% fewer women were screened for CC5,6.
At this stage, recommendations were drawn up by Central RHA to guide women with altered screening tests. According to these, women with positive HPV test for types other than 16 and 18 (HR-HPV) and reflex cytology ASC-US/ LSIL, should be addressed to repeat screening within one year in primary healthcare5.
Thus, the aim of this study is to assess the impact of the guidance of women with HR-HPV positive/reflex cytology-ASCUS or LSIL, referred to the Gynaecology department of the Portuguese Institute of Oncology of Coimbra (IPOC), in the initial phase of the pandemic. We sought to assess the prevalence of transient infections and which risk factors are associated with the persistence or elimination, and secondarily, we sought to assess the prevalence of high grade squamous intraepithelial lesions -HSIL/CIN2+.
Material and Methods
We conducted a nested case-control study of a cohort of women with HR-HPV and ASCUS or LSIL reflex cytology. The initial cohort included 215 women, screened from 27 March 2019 to 30 March 2020 and referred to the Gynaecology department of IPOC. The data were obtained during the month of March 2022, by consulting the Siima platform and the hospital clinical files.
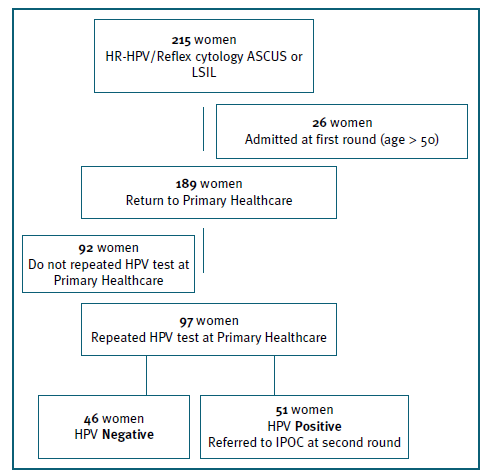
This sample was evaluated through two rounds. At first round, 26 women, older than 50 years, remained at the department and 189 were sent back to primary healthcare. The option to not return older women, was taken based on the higher risk of persistence and progression of HPV, at these ages7. At second round, 51 were readmitted, based on a second positive HPV test. (Figure 1)
Based on this, the cohort analysis was then stratified by three groups: 1) the first group comprised 189 women referred to repeat HPV test at primary healthcare. Ninety-two women were excluded for not having repeated the test, so this group included 97 women; (Figure 1); 2) the second group consisted of the 77 women referred to the department, 26 women admitted in a first round and 51 in a second round, after a second positive HPV test. The evaluation of this group allows the assessment of HSIL/CIN2+ prevalence and the identification of cofactors connected with HPV persistent; 3) finally, the third group, included those women who repeated the HPV test (97 at primary healthcare and 14 at the department). From this third group, 15 women readmitted because of a second positive HPV test, where retested at the department. Thereby, a total of 126 HPV tests were performed. This allows us to assess elimination/persistence rates and to identify potential associated cofactors.
Within the study, women with persistent HR-HPV infection were considered as cases and those who eliminated it were considered as controls.
The following variables were analyzed: age at diagnosis, contraceptive method, parity, smoking habits, menopause, HPV vaccination, history of lower genital tract treatments, first CCS, date of first collection, reflex cytology result, date of second collection, HPV typing (Cobas test®), referral to IPOC, colposcopy findings (according to 2011 International Federation of Cervical Pathology and Colposcopy nomenclature), 8 treatments performed, histology and time to HR-HPV clearance.
Statistical analysis was performed using the STATA program (version 13.1), with statistically significant results if p≤0.05 and 95% confidence level. Fisher’s exact or chi-square test were applied to assess the relationship between nominal variables, and Student t-test or Wilcoxon’s test were applied for comparison between measures of central tendency (according to the presence or absence of normal distribution). Adjustment for confounding factors (such as age, smoking, reproductive status, parity, contraception, or vaccination) was made by applying logistic regression. Kaplan-Meier curves were used to describe the distribution of elimination time and the log-rank test was used for comparison.
The study was approved by the ethics committee of IPOC and it has been conducted in accordance with the principles set forth in the Helsinki Declaration.
Results
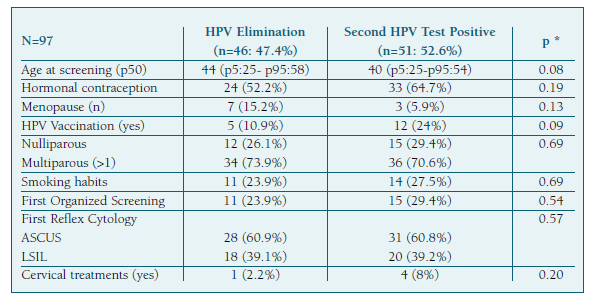
We initially assessed data from 215 women with HR-HPV infection and reflex cytology: ASCUS/LSIL. (Figure 1) Of those 97 women who repeated the HPV test at primary healthcare, approximately 47% cleared the infection. From this, five were older than 50 years, and all eliminated the infection. HPV clearance was not statistically associated with any of the analyzed cofactors, namely age, smoking habit, or vaccination status. (Table I) Within the cohort that cleared HR-HPV infection, the median time to clearance was 14.5 months [10.1-22.9].
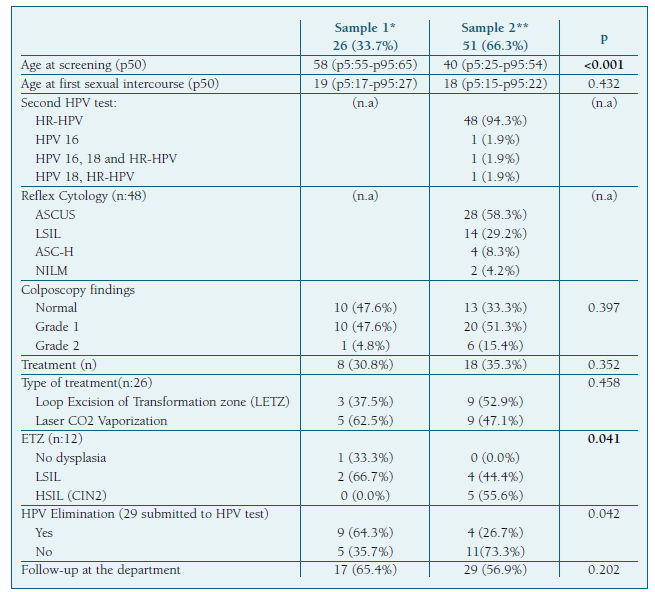
In the second group of women (n:77), we found that, of the 51 women admitted to the gynecology department after a second positive HPV test, 94% had persistent infection with the same high-risk group, while 6% had other genotypes (one with HPV 16 and two with multiple infections). (Table II) In this group, it was possible to evaluate the histological findings (by biopsy and/or loop excision of the transformation zone-LETZ) in 34 cases, with low-grade intraepithelial lesions identified in 74%, high grade intraepithelial lesions (HSIL/CIN2) in 15% and absence of dysplasia in the remaining. All HSIL/CIN2 lesions were identified in the group of women referred with a repeated positive HPV test. (Table II) We didn’t find any statistically significant association between the severity of dysplastic lesions and the HPV genotype. Virus clearance was higher in women observed in the first round. (Table II ) Per multivariate analysis, no significant association was observed with any of the risk factors analyzed (e.g., smoking habits, reproductive status, parity, vaccination status or reflex cytology result). Within the cohort referred to IPOC, the median time to clear the infection was 19.5 months [13.5-24.5].
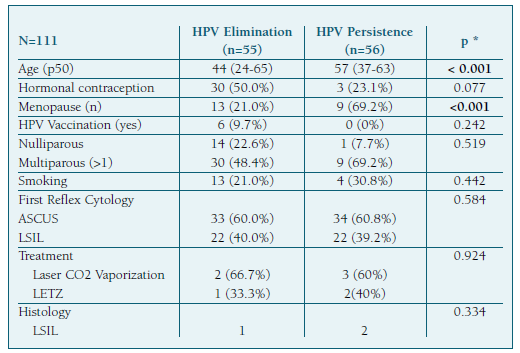
Finally, when assessing the group of women who repeated the HPV test, we found that clearance and persistence were very similar. Per univariate analysis, it was possible to verify that, within the assessed risk factors, only age and menopausal status had a statistically significant difference (p<0.001). (Table III) When adjusting for confounding factors such as smoking habits, parity, contraception or vaccination, no significant differences between groups could be identified. However, smoking was associated with a higher risk of persistence (OR: 2.62 (p: 0.244; 95% CI (0.52-13.28)), as well as menopausal status (OR: 6.06 (p: 0.156; 95% CI (0.50-72.97). We also found that, among women submitted to a third HPV test, about 75% had persistence, regardless of the treatment or other cofactors.
Discussion
According to the literature, the transition to HPV screening program, although associated with more clinically relevant findings, entails a significant increase in referrals for colposcopy and an inherent higher burden of colposcopic units. Most of these referrals are mainly caused by HR-HPV infection with low grade reflex cytology (ASCUS and LSIL), rarely associated with high-grade lesions9-10.
In evaluating a sample of women with HR-HPV and low-grade (ASCUS/LSIL) reflex cytology, we demonstrated that it was possible to avoid the referral of 46 women without compromising safety.
Recently, different societies have updated the CCS guidelines, based on an individualized risk stratification of developing HSIL/CIN3+ lesions (“equal risk, equal approach”) 11.
The Australian National CCS Program, published in January 2022, is based on a partial genotyping HPV test (16/18 and others), every five years, as it happens with the Portuguese CCS program12. However, risk is stratified into three levels: low, intermediate, and high. The intermediate risk includes HR-HPV infection and low-grade reflex cytology (NILM, ASCUS or LSIL). These women repeated the test after 12 months. These guidelines were based on the study of 8425 women (NILM:5825; ASCUS/LSIL:2600) aged 25 to 74 years, in which a high prevalence of transient infections was observed13. This triage strategy was also adopted by other programs14.
Like the Australian program, the recently updated Portuguese guidelines also mention the HSIL/CIN3+ risk. According to this consensus, women with HR-HPV and ASCUS or LSIL reflex cytology, have indication for colposcopy, based on the risk for HSIL/CIN3+, higher than 4%15.
Through our study, we observed that smokers had almost three times the odds of having HPV persistence than non-smokers, and postmenopausal women had six times the odds of having HPV persistence than premenopausal women, as previously reported7. We also verified that only five cases of HSIL (CIN2) were detected, all in women referred for persistence (second HPV positive test) regardless of the initial result of reflex cytology. Also, Gage J. et al. had demonstrated that the risk of CIN2+ lesions is similar in the group of HR-HPV infections, despite the reflex cytology findings (logistic-Weibull model: 3-year CIN2+ risk: 15.7% (HPV/ASCUS) vs. 15.2% ((HPV/LSIL)), p = 0.5) 16.
Concerning the older women (age 50+), we observed that, despite higher persistence of HPV infection, this was not associated with high-grade lesions development in these age groups. Similarly, Plummer et al, found that, in 4504 women with HR-HPV infection and ASCUS/LSIL cytology, those aged 50 years or older had the highest persistence rate at 24 months (OR: 1.47 (1.11-1.94)) 17. Instead, Gage J. and collaborators, verified that among a cohort of 972,029 women aged 30-64, the rates of both prevalent and incident HPV infections declined dramatically by age, while the associated 5-year CIN3+ risk did not increase with age18. Therefore, based on this and on our results, we could suggest that there is no need to enact a different approach for older women.
Plummer et al, also found that regardless of age, when the HPV infection persisted at 12 months, is expected to continue at 18 and 24 months. 17 These outcomes are in accordance with our findings in the group of women referred to the institution, i.e., the rate of HPV clearance was lower in those who had a second HPV positive test.
The strengths we identified in our study are its simplicity of execution and the adjustment for potential confounding factors.
The limitations identified are the retrospective nature, the size of the sample and the inclusion of only one center. Another limitation is related to the group of women who did not repeat the test at primary healthcare - it represents a high proportion of missing data, compromising the effectiveness of our study. However, as a result of this research, they were recalled for repetition of the test in primary healthcare. Finally, it should be noted that the Cobas test® does not distinguish HR-HPV other than HPV16 or 18, so it is not possible to know whether a persistent positive HR-HPV test is a true persistence or reinfection with another HR-HPV genotypes.
With this study, we demonstrated that this approach would enable better resource management (unnecessary medical appointments, exams, and treatments) without losing the safety and quality of the care.
As a final remark, we consider that larger studies would be useful, to provide stronger and more reliable results, for the purpose of reassessing women with HR-HPV infection and reflex cytology ASCUS or LSIL at primary healthcare, 12 months after the initial sample.