Image report
A 91-year-old woman with Alzheimer’s dementia, arterial hypertension, dyslipidemia, and diabetes mellitus type 2, without surgical history, who has undergone a previous vaginal hysterectomy 8 years ago, performed for symptomatic hysterocele. Both the surgery and the postoperative period were uneventful. She was brought to the gynecology emergency department due to a large vulvar swelling, after an unattended fall. At admission, the woman was disoriented and non-cooperative (no different from her usual), with abnormal flexor response to painful stimuli, apyretic and hemodynamically stable. Gynecological examination revealed evisceration of intestinal loops through the vagina, swollen and soiled with feces (due to fecal incontinence). There wasn’t macroscopic intestinal damage and it was not possible to identify the vaginal mucosa, due to the interposition of intestinal loops (Figure 1).
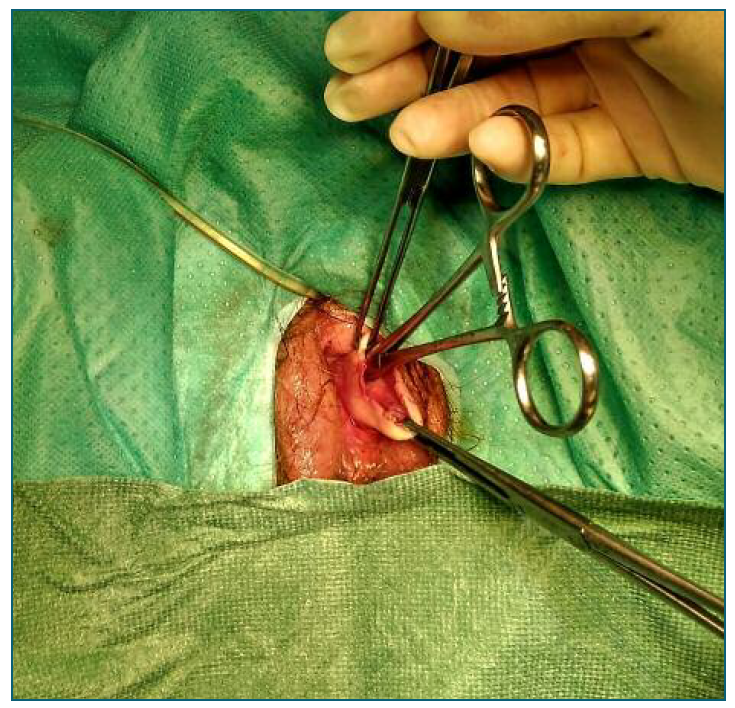
In the operating room, the surgical team promptly underwent manual reduction of the evisceration in collaboration with general surgery, once exposed intestinal loops appeared viable. VCD was identified, with no lacerated or bleeding edges and no pathological vaginal or peritoneal exudates were observed. Cuff closure was performed by the gynecology team (Figure 2). The granulation tissues at the vaginal cuff’s edge were excised and dehiscence correction was carried out using tobacco pouch suture and invaginating suture of the closed orifice. Broad-spectrum intravenous antibiotics (cefuroxime and metronidazole) were administered.
Three days after, her intestinal transit was regularized, without signs of peritoneal irritation. Analytically there was mild hypokalemia (K+ 3.2 g/dl) and C-reactive protein in descending profile (194 mg/L in 1st postoperative day to 127 mg/L in 3rd postoperative day).
Between the 3rd and the 6th postoperative day, the patient completed a cycle of IV antibiotic therapy and hypokalemia correction. On the 7th postoperative day, after an episode of food aspiration, she developed acute pulmonary edema, with the need for ventilation support. Considering the patient’s age and her dependence on activities of daily living, it was decided to implement comfort measures. The patient died 6 hours later.
After a hysterectomy, a vaginal incision is typically closed by suturing the anterior and posterior edges together. VCD, which consists of the separation of the vaginal edges, is a rare gynecological surgical complication. Our patient missed the postoperative consultation, so it was not possible to evaluate the integrity of the vaginal vault after surgery. However, her daughter did not describe complications after the hysterectomy.
In the literature, VCD’s incidence is estimated between 0.032% and 1.25%1,2, depending on the mode of hysterectomy, surgical technique, suture utilized for cuff closure, and operator’s experience3. Most studies are underpowered and lack direct comparison groups within each mode of hysterectomy to be able to effectively assess the effect of these different variables4. Additionally, there is no consensus about the ideal method of surgical repair after VCD or evisceration3. In our case, the cold-cut colpotomy technique using scissors was performed and the suture of the vaginal cuff was executed with U-stitches with multifilament braided thread 1/0.
VCD can lead to a vaginal evisceration of abdominal viscera - an emerging surgical condition, whose incidence, with few cases reported in the literature, is difficult to determine. The median time reported for evisceration after pelvic surgery is 20 months5. Evisceration can occur spontaneously, but some risk factors have been reported following vaginal traumas caused by coitus, obstetric instrumentation, foreign body insertion, and direct trauma, as well as after pelvic surgery and in patients with enterocele4,6. Besides that, it could be associated with a sudden increase in intra-abdominal pressure such as cough, constipation, or fall in postmenopausal women4,6. This is in line with the characteristics of our patient - a postmenopausal woman with a previous hysterectomy and a history of falls, which cannot be excluded as a cause of evisceration.
The evisceration of the bowel through the VCD can be complicated with ischemia, perforation, deep thrombosis vein, intra-abdominal sepsis, peritonitis, and death, hence the need for brevity in its surgical resolution7.
The authors present this case to remind gynecologists of the importance of early diagnosis of this rare life-threatening condition, the multidisciplinary approach, and prompt surgical intervention to prevent necrosis, sepsis, and death.