Introduction
Ectopic pregnancy is known to be the leading cause of maternal death in the first trimester of gestation and represents 1.5-2% of all pregnancies1. There are several risk factors associated with extrauterine pregnancy such as prior pelvic surgery, altered tubal motility, tubal scarring, history of secondary infertility, pelvic inflammatory disease, and hormonal variation. However, approximately half of the ectopic pregnancies occur in women with no identified risk factors2. Ectopic pregnancies are most commonly implanted in the fallopian tubes, although nearly 10% are implanted in non-tubal locations, including the uterine cornua, wi-thin a caesarean section scar, the broad ligament, abdominal cavity, ovary, or in the cervix3. Non-tubal ectopic pregnancy are likely to present later than the tubal ones, since they are able to grow larger before becoming symptomatic. As such, they have greater maternal morbidity and mortality, with reported rates as high as 20%4. Thus, early detection and timely initiation of therapy remain the foundations for reducing this ratio. Broad ligament pregnancy is a rare, life-threatening form of ectopic abdominal pregnancy and accounts for approximately 1% of all the ectopic pregnancies5. It is a retroperitoneal pregnancy that develops within the leaves of the broad ligament6. As reported by Champion et al it has an incidence of 1 in 183,900 pregnancies7. The diagnosis is rarely established before surgery, although Phupong et al reported a case where it was diagnosed preoperatively8. Symptoms of broad ligament pregnancy include abdominal pain and vaginal bleeding9. Intraoperative diagnosis can be made when the pregnancy is noted to be lateral to the uterus, medial to the pelvic side walls, superior to the pelvic floor and inferior to the fallopian tube. Although an effective laparoscopic approach has been described, traditionally is managed via laparotomy10. We report a case of a woman diagnosed with broad ligament pregnancy at 21 weeks. The diagnostic and clinical management of a broad ligament pregnancy was discussed and incorporated prevention, surgical treatment, and prognosis.
Case Report
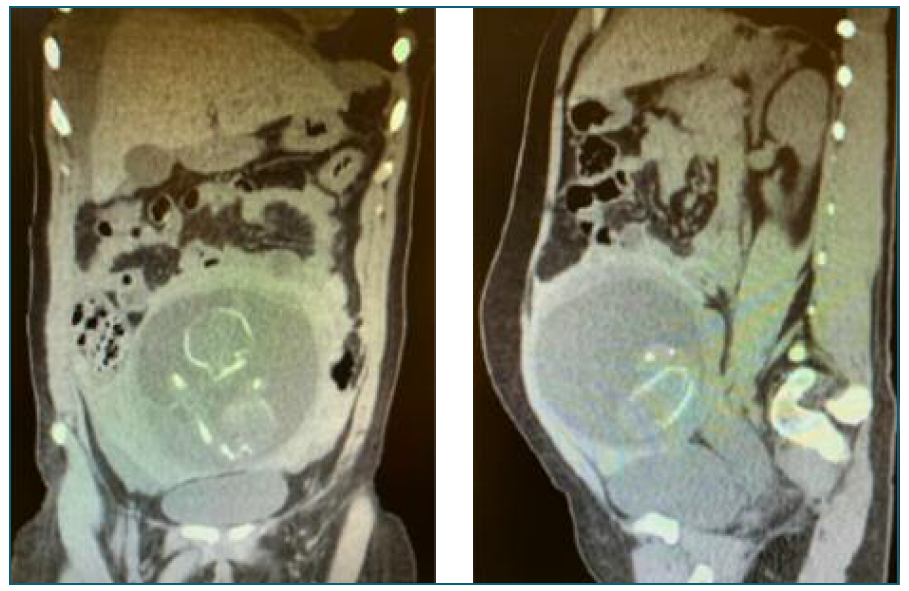
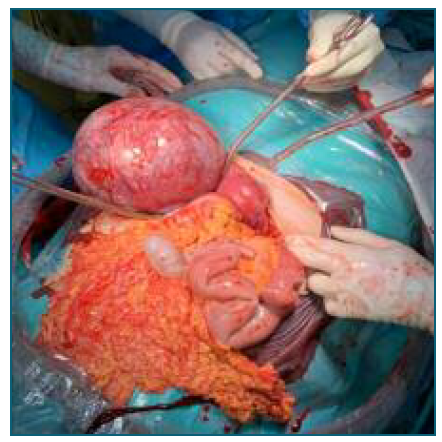
A 29-year-old nulliparous with a previous spontaneous miscarriage, was admitted to the emergency room at 21 weeks presenting middle abdominal pain, nausea and vomiting that had started that day. Her past clinical and family history were unremarkable. The patient had undergone two previous obstetrics ultrasounds, at 12th and 20th weeks of gestation, describing a normal intrauterine pregnancy. During pregnancy she presented three times to the emergency room, with abdominal pain and was discharged with diagnosis of normal pregnancy symptoms. During the latter visit physical examination revealed mild pallor, normal blood pressure and heart rate. She had lower abdomen pain at palpation with no signs of acute abdomen. An ultrasound was conducted and showed a normocardic fetus in pelvic presentation with low-lying placenta. Transvaginal ultrasound showed a stranger cervix with more than 40 mm. Retro uterine cul-de-sac was fluid free. Blood tests were performed. Haemoglobin - 12.5 g/dl and leukocytes - 18.87, all other haematological and biochemical parameters were within normal range. While in the emergency room, she experienced a sudden onset of severe abdominal pain, pallor, and hypotension. For this reason, an abdominal and pelvic computerized tomography (CT scan) was performed which showed peritoneal effusion in all abdominal quadrants which was indicative of hemoperitoneum (Figure 1). After further review of the CT scan, it was not possible to confirm or exclude the integrity of the uterine wall. Considering the patient’s symptoms and the CT scan findings, the decision was made to repeat the obstetric ultrasound. At this point, the exam showed a great amount of hypoechoic fluid, suggestive of hemoperitoneum. To exclude a possible ovarian cyst rupture, a second meticulous observation of the adnexal areas was performed and revealed an extra-uterine sac with a fetus moving, lateral to an empty and small uterus. Her haemoglobin had dropped to 8.8 g/dL, and she became clinically unstable with a decreased consciousness state. It was decided to perform an emergency laparotomy. A ruptured ectopic pregnancy with approximately 9 cm in the left broad ligament was found below the left ovary (Figure 2). The rupture caused a large hemoperitoneum with a decrease in haemoglobin up to 6 gr/dL. Left salpingectomy with surgical removal of ectopic pregnancy was performed (Figure 3), while blood transfusion was being administer. Right adnexa was normal. Patient had an uneventful recovery and was discharged on the 3rd post-operative day. Pathological report described a broad ligament mass with 13,5×13×9 cm; a fetus with normal development expected at 21 weeks of gestation and a placenta inside. (Figure 4).
Discussion
Broad ligament ectopic pregnancy is a rare but serious condition due to its late presentation and challenging diagnosis. Traditionally has been associated with significant maternal morbidity and mortality6,11. One explanation for a broad ligament pregnancy is that it results from trophoblastic penetration of tubal pregnancy through the tubal serosa and into the mesosalpinx, with secondary implantation between the leaves of broad ligament. Another possible explanation is the occurrence of a uterine fistula between the endometrial cavity and the retroperitoneal space12. Regarding risk factors, this patient supposedly did not present with the commonly associated ones: no history of pelvic inflammatory disease, use of intrauterine devices or previous history of ectopic pregnancy. There are various clinical presentations for broad ligament pregnancy reported in the literature, the most common being lower abdominal pain during early gestation, such as reported by this clinical case patient13. Diagnosis of broad ligament pregnancy requires high degree of suspicion, and it is often made intra operatively. Despite improvements in ultrasound technology, correct initial diagnosis is still missed on most occasions. Our patient had three ultrasound reports and none of them were suggestive of extra uterine pregnancy. She had a pregnancy without apparent complications, with two previous visits to the hospital due to mild abdominal pain. When we thought that the cervix was strange, we should have paid more attention to the ultrasound, and try to understand what was wrong . In fact, we were looking for the uterus itself. But at 21 weeks, you really didn’t think that it was an ectopic pregnancy, especially one that was being followed regularly. But from this, we learn that we always need to confirm the intrauterine location of every pregnancy coming into our attention for the first time. Intra-ligamentous pregnancy has been reported to be associated with maternal mortality as high as 20%, perinatal mortality ranging between 40 and 90% and foetal deformities of around 21.4%14. As we have seen in this case report, this condition can abruptly develop into a life-threatening situation. It is important to be aware of this diagnosis to promptly treat, consequently decrease mortality and potentially increase fertility preservation.
Author Contribution Statement
Ana Rita Silva: Conceptualization; Data curation; Investigation; Methodology; Resources; Visualization; Writing - Original draft. Mariana Veiga: Conceptualization; Methodology; Resources; Visualization; Writing - review & editing. Ana Brandão: Supervision; Visualization; Writing - review & editing. Filomena Nunes: Supervision; Visualization; Writing - review & editing.
Ethical considerations
The patient had provided written informed consent for publication of their data.