Issue Image/Imagem do Trimestre
Laparoscopic excision of functional rudimentar cavity for chronic pelvic pain in adolescence
Excisão laparoscópica de cavidade uterina rudimentar funcional em adolescente com dor pélvica crónica
1. Hospital Divino Espirito Santo, Ponta Delgada, Portugal.
2. Centro Hospitalar Universitário São João, Porto, Portugal.
Abstract
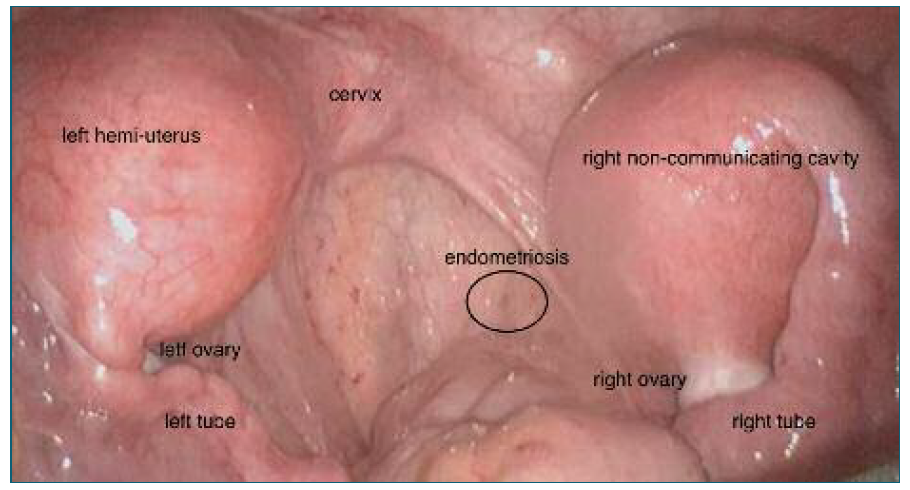
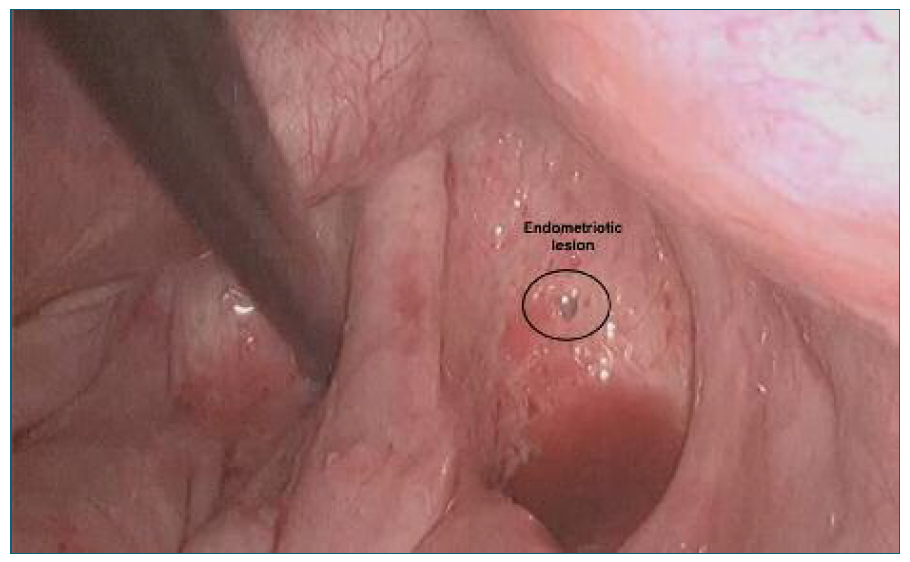
A female adolescent presented with recurrent pelvic pain, severe dysmenorrhea, and catamenial diarrhea for 2 years. Ultrasound and magnetic resonance imaging suggested a hemi-uterus with a non-communicating rudimentary cavity. Hysteroscopy revealed a normal vagina and cervix, and one tubular uterine cavity with only the left tubal ostium. During laparoscopy, a left hemi-uterus was observed with a normal left ovary and tube, and a non-communicating rudimentary cavity on the right side with normal adnexa (ESHRE/ESGE U4aC0V0). Blood and endometriotic lesions were present at the pouch of Douglas. Excision of the rudimentary cavity, tube, and endometriotic lesions was performed.
Keywords: Mullerian malformatian; Chronic pelvic pain; Adolescence; Functional rudimentary cavity
Resumo
Adolescente do sexo feminino observada na urgência de ginecologia por dor pélvica crónica, dismenorreia grave e diarreia catamenial desde há 2 anos. Realizou ecografia e ressonância magnética com visualização de hemi-útero com uma cavidade rudimentar não comunicante. À histeroscopia com vagina e colo normais, uma cavidade uterina tubular com um único óstio tubário esquerdo. Na laparoscopia, observado hemi-útero esquerdo com ovário e trompa esquerdos normais e uma cavidade rudimentar não comunicante à direita com anexos normais (ESHRE/ESGE U4aC0V0). Apresentava também sangue no fundo de saco de Douglas e lesões endometrióticas. Foi realizada a excisão da cavidade rudimentar, da trompa e das lesões endometrióticas por via laparoscópica.
Palavras-chave: Malformação mulleriana; Dor pélvica crónica; Cavidade rudimentar funcional
A 17-year-old female virgin presented to the emergency department with complaints of severe spasmodic pain in the lower abdomen. She reported recurrent pelvic pain, severe dysmenorrhea and catamenial diarrhea for the last 2 years. No cause was found for the diarrhea and a right renal agenesia was diagnosed in the meantime.
On observation, she had abdominal tenderness in the inferior quadrants with no signs of peritoneal irritation. Full gynecological examination was not possible to perform due to normal intact hymen. Ultrasound was suggestive of uterine malformation with hematometra.
The patient was prescribed oral continuous combined pill and a follow-up appointment was scheduled.
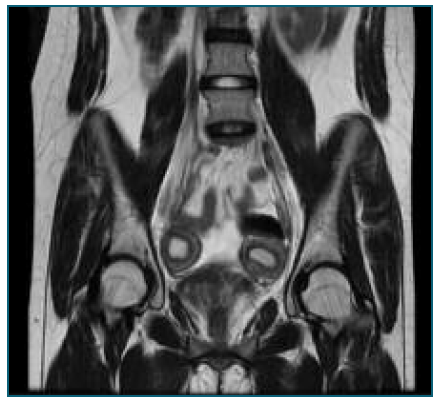
A transrectal and abdominal ultrasound and a magnetic resonance imaging (MRI) were conducted and indicated the presence of a hemi-uterus with a non-communicating functional rudimentary cavity. However, the evaluation of the vagina was inconclusive.
After discussing with the patient and her parents, she was proposed for diagnostic hysteroscopy and laparoscopic removal of the rudimentary cavity.
Hysteroscopy revealed a normal vagina and cervix and one tubular uterine cavity with a single left tubal ostium. On laparoscopy a left hemi-uterus was noticed with normal left ovary and tube and a non- communicating right rudimentary cavity with normal adnexa (ESHRE/ESGE U4aC0V0) (Figure 1).
A significant amount of blood was found in the pouch of Douglas, and two superficial endometriotic lesions were also detected. Excision of the right rudimentary cavity, right salpingectomy and excision of endometriotic lesions was performed. (Figure 2)
The procedure and post-operative period were uneventful.
The patient was observed one month later with no complaints and was discharged home.
Congenital malformations of the female genital tract are deviations from normal anatomy resulting from embryological maldevelopment of the Mullerian or paramesonephric ducts. They are a common benign condition, with a prevalence of 4-7%1. Renal tract anomalies are associated with congenital malformations of the female genital tract in up to 30% of cases due to the embryologic relationship between the paramesonephric and mesonephric ducts2. The most common renal tract anomaly associated is renal agenesis3.
Diagnosis of a uterine malformation can be challenging due to its multiplicity, multivariate and sometimes unspecific symptoms. The presence of a functional endometrial cavity in the non-communicating horn explains the findings of severe dysmenorrhea, hematometra, and endometriosis. Diarrhea can likely be attributed to endometriosis due to the associated inflammatory activity and local prostaglandin release, which can alter bowel function4.
2D and 3D transvaginal gynecologic ultrasound are the first-line imaging modalities to assess these women. However, MRI is a non-invasive exam, making it particularly useful in pediatric and virgin patients5 (Figure 3).
A functional non-communicating uterine cavity typically leads to blood retention and retrograde blood flow, increasing the risk of hematometra, infection, endometriosis, and infertility. Accurate diagnosis is crucial to establish an appropriate treatment and surgical approach.
The prognosis is favorable when diagnosed and treated promptly. In the absence of complications, the vast majority of the patients achieve successful pregnancies in the future6.
Author’s contribution
Sara Dias Leite - Writing of the article. Ana Sofia Fernandes - Critical review of the intelectual content and Final approval of the version to be published.
Conflicts of interest
No conflicts of interest.
Informed consent
Informed consent was obtained.
References
1. Grimbizis GF, Gordts S, Di Spiezio Sardo A, et al. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod. Aug 2013;28(8):2032-44. doi: https://doi.org/10.1093/humrep/det098
[ Links ]
2. Del Vescovo R, Battisti S, Di Paola V, et al. Herlyn-Werner-Wunderlich syndrome: MRI findings, radiological guide (two cases and literature review), and differential diagnosis. BMC Med Imaging. Mar 9 2012;12:4. doi: https://doi.org/10.1186/1471-2342-12-4
[ Links ]
3. Gholoum S, Puligandla PS, Hui T, Su W, Quiros E, Laberge JM. Management and outcome of patients with combined vaginal septum, bifid uterus, and ipsilateral renal agenesis (Herlyn-Werner-Wunderlich syndrome). J Pediatr Surg. May 2006;41(5):987-92. doi: https://doi.org/10.1016/j.jpedsurg.2006.01.021
[ Links ]
4. Ek M, Roth B, Ekström P, et al. Gastrointestinal symptoms among endometriosis patients - A case-cohort study. BMC Womens Health. 2015 Aug 13;15:59. doi: https://doi.org/10.1186/s12905-015-0213-2. PMID: 26272803; PMCID: PMC4535676.
[ Links ]
5. Maciel C, Bharwani N, Kubik-Huch RA, et al. MRI of female genital tract congenital anomalies: European Society of Urogenital Radiology (ESUR) guidelines. Eur Radiol. 2020 Aug;30(8):4272-4283. doi: https://doi.org/10.1007/s00330-020-06750-8. Epub 2020 Mar 27. PMID: 32221681; PMCID: PMC7338830.
[ Links ]
6. Candiani GB, Fedele L, Candiani M. Double uterus, blind hemivagina, and ipsilateral renal agenesis: 36 cases and long-term follow-up. Obstet Gynecol. Jul 1997;90(1):26-32. doi: https://doi.org/10.1016/s0029-7844(97)83836-7
[ Links ]