Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Angiologia e Cirurgia Vascular
versión impresa ISSN 1646-706X
Angiol Cir Vasc vol.8 no.2 Lisboa jun. 2012
Popliteal Artery Adventitial Cyst: case report and literature review
Angelo Frankini*,**, Airton Delduque Frankini*,**, Tiago Frankini*,**
* School of Medicine Universidade Federal de Ciências da Saúde de Porto Alegre (University of Health Sciences of Porto Alegre)
** Service of Vascular Surgery, Santa Casa de Porto Alegre Hospital, Brazil.
|ABSTRACT|
The popliteal artery adventitial cyst is not a commonly studied pathology due to the rarity of its occurrence, however it is a disease that should always be considered as a differential diagnosis in the presence of a young patient who complains of claudication of the lower limbs. Because of its importance, the aim of this paper is to review some concepts about this disease based on a case report, analyzing its occurrence, etiopathology, clinical manifestations, diagnosis and treatment options.
Key words: cyst, popliteal artery, claudication
Cisto Adventicial de Artéria Poplítea: relato de caso e revisão da literatura
|RESUMO|
O cisto adventicial de artéria poplítea é uma patologia pouco estudada na literatura devido à raridade de sua ocorrência, porém é uma situação que serve como diagnóstico diferencial sempre que estivermos diante de um paciente jovem com claudicação. Em virtude da sua importância, este trabalho tem como objetivo revisar alguns aspectos acerca do assunto, baseado em um relato de caso, analisando sua ocorrência, etiopatogenia, manifestações clínicas, métodos de diagnóstico e opções de tratamento.
Palavras-chave: cisto, artéria poplítea, claudicação
INTRODUCTION
The popliteal artery adventitial cyst is a rare condition with low prevalence in the literature, however it is one of the causes of intermittent claudication of the lower limbs in younger patients. Due to its rarity, its pathology is not well defined, which can lead to a wrong diagnosis and therefore an inadequate treatment. The adventitial cyst is a non-atherosclerotic disease without an accurately known and still with a controversial etiology. It determines a compression of an arterial segment, usually in the lower limbs resulting in stenosis. The diagnosis can be mistaken for other pathologies, like popliteal artery entrapment syndrome, arteritis or Bakerís cyst. The definitive treatment is surgical and, to some authors, the endovascular treatment of the stenosis or occlusion is contraindicated.
CASE REPORT
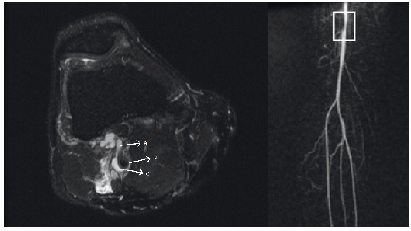
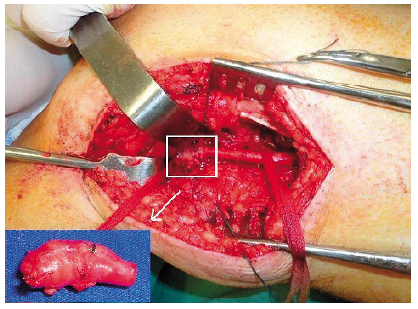
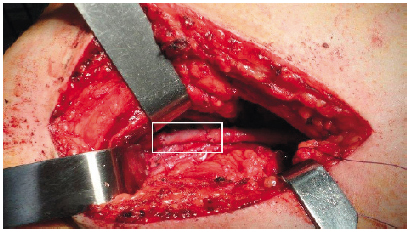
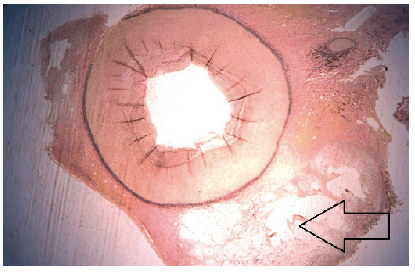
J.O.L., male, caucasian, 50 years old, with no comorbidities, no previous history of tobacco use or any other risk factor for atherosclerotic disease was referred to our institution. The patient presented with a two month onset of intermittent claudication for 70 meters in the right calf, which considerably limited his usual activities. At the physical examination he was euthrophic, had normal vital signs, with a diminished popliteal and tibial posterior pulses, no pulse in the dorsalis pedis artery and normal pulses in the left lower limb. He had a magnetic angioressonance that showed a cystic image with its geometrical center at the popliteal artery adventitia, 3.5 centimeters proximal to the articular line, with stenosis of the vessel and fistulous path to the articular cavity of the knee |Figure 1|. The patient underwent surgery with medial approach of the popliteal artery and resection of the segment that contained the adventitial cyst (about 3cm). |Figure 2| The reconstruction was made by interposition of a segment of the saphenous magna vein exerted from the right thigh |Figure 3|. The pathology presented a 2.3 cm segment of the popliteal artery with a medial bulging area. When cut, revealed a well delimited nodule, with mixoid content, within the vessel wall. The diagnosis was mucoid ganglionic cyst. |Figure 4| He was discharged on the fourth post-operative day with normal popliteal and posterior tibial pulses. He has 12 months of follow-up and remains asymptomatic, maintaining his regular activities.
| FIGURE 1 | MRI image showing the "scimitar sign" due to focal stenosis of the popliteal artery above the knee. A – fistulous path. B – Popliteal artery. C – Cyst.
| FIGURE 2 | Medial approach of the popliteal artery above the knee with identification of the cyst near the knee joint. Detail: anatomical piece of the popliteal artery with the adventitial cyst.
| FIGURE 3 | Arterial reconstruction of the popliteal artery with interposition of the saphenous magna vein with termino-terminal anastomosis.
| FIGURE 4 | Pathological exam with the cyst at the adventitial layer.
DISCUSSION
Etiopathology
The arterial adventitial cyst is not a frequent pathology. Worldwide literature by now presents about 400 cases, since 1947, when Atkins and Key[1] published one patient with ischemia of the lower limb caused by the presence of an adventitial cyst of the popliteal artery. Currently this is the 13th case report on the Brazilian literature, after an actualized review of the Medline database.
Various theories were postulated to explain the formation of cyst in the arterial wall, however none have unquestionable evidence. The ganglionar hypothesis, in which a growing synovial cyst chronically in contact with the adjacent artery implants itself in the adventitia of the vessel, is very accepted[2]. Another theory that is well accepted, although lacks in evidences, is that chronically repeated microtraumas could injure the adventitia leading to the formation of the cyst[3]. There is also the embrionary theory, one of the most accepted, in which due to a flaw in the development of some individuals, mucine secreting cells originated in the articular mesotelium would be present in the arterial wall leading to the formation of the cyst. Some authors suggest that the confirmation of this theory is the frequent identification, on image studies or intraoperative, of a communication of the cyst with the articular capsules close to itself[4]. Linquette et al suggested that the cyst was part of a systemic disease that altered the conjunctive tissue, however not proved in long term[5].
The most common location is the popliteal area, however there were cases in the upper limbs on arterial segments close to the shoulder, elbow or wrist articulations. There were also cases of the saphenous and femoral veins, close to the articulations. The cyst is characteristically unilateral[6].
An analysis of 374 reported cases, in 2005, showed 83% were in the popliteal artery[7]. The cyst contains a gelatinous, mucoid, thick, colorless secretion that sometimes can become reddish due to a minor bleeding. The external wall has fibrous tissue with small vessels and internal wall is lamellar fibrous tissue[8].
Diagnosis
The disease is more prevalent in men from 30 to 50 years old. Usually the patient has no risk factors for atherosclerotic disease. The most common complaint is the recent onset of intermittent claudication of the calf, progressive and unilateral. There can also be neurological symptoms, such as paresthesia of the extremity. The incidence of the disease is 0.01% of the claudicating patients[7]. Physical examination can show diminished or even absent popliteal and podal pulses. Palpation of a mass on the popliteal region, that can be mistaken as a popliteal aneurysm or Bakerís cyst, can be present, as well as murmur and fremitus[7,8]. The Ishikawa sign is a semiological test that is observed in the minority of cases, however can aid the diagnosis and consists in provoking ischemia of the affected limb and disappearance of the pulses by forcing complete flexion of the knee for five minutes, while the patient is in supine position[8].
The mandatory differential diagnosis are atherosclerotic arterial obstructive disease that usually presents in older patients, associated with comorbidities; Bakerís cyst, which is an extrinsic compression of the artery, palpable on the popliteal region, not related to the arterial wall; obliterans thromboangiitis, that occurs in young and tobacco use patients usually accompanied with ulcers, rarely claudicans and with migratory phlebitis; and popliteal artery entrapment syndrome (PAES), that also occurs in young patient, but with well developed muscles, in which podal pulses become impalpable when the patient maintains extension of the knee with forced flexion of the foot, while in the cystic disease the pulse disappears when the knee is flexed. It is also important that PAES on image studies does not have a cystic structure and deviates medially the popliteal artery[7].
Imaging studies
The best studies to confirm the diagnosis of popliteal artery adventitial cyst are the arterial duplex scan and magnetic angioresonance (angioMRI). The angio computerized tomography (angioCT) is also useful, however in some cases cannot exclude the differential diagnosis of popliteal aneurysm since it reveals mainly the cystic pattern of the lesion, which occurs in both pathologies. The angioMRI and duplex scan show clearly a cystic structure (anechoic or hipoechoic) in the arterial wall with no blood flow or atherosclerotic plaque in the interior, confirming the diagnosis. The later method has a better sensibility and is the only method used for some authors[9]. The use of angioMRI or angioCT reveals more details of the pericystic area, the cystic relation to adjacent structures and can exclude differential diagnosis such as PAES. The angioMRI to some authors is the most thorough study[10] since it can identify a connection of the cyst to the adjacent articulation, as registered in three cases by Tsilimparis et al in 2007 and referred by other authors[4]. The connection was present in our case |Figure 1|. Images from angioMRI[10], angioCT or even conventional arteriography aid the precise diagnosis and mainly the surgical plan for reconstruction which leads to better results in terms of recurrence. The arteriography can show from small stenosis to even the total occlusion of the vessel on the local or immediately below the cyst compression. On the remaining arterial segments minimum or no atherosclerotic lesion is visualized with poor collateral circulation[7,11]. The stenosis in various degrees is present in about 70% of the cases. On the reported case the scimitar sign was present, which is one of the most usual ones, as well as the hourglass sign[11]. The angiographic image varies according to the extension, the volume of the cyst and whether it compromises the entire arterial circumference or only part of it[10].
Treatment
The treatment of the intermittent claudication caused by the cyst differs from the usual treatment, since it is not an atherosclerotic lesion, but an extrinsic compression on the arterial wall with no certain ethiology. For this reason, even though the modifiable factors for atherosclerosis are treated (i.e. hypertension, diabetes mellitus, dyslipidemia, tobacco) when present, there will be no influence in the progression of the compression caused by the cyst. The use of peripheral vasodilators and antiplatelet drugs is just a palliative measure and will not have satisfactory results. With that in mind, the interventional treatment, with open surgery as the best option, although recently there have been more frequent and controversial attempts to treat with endovascular technique, should be performed. Simpler and more conservative treatments, such as aspiration of the cystís content guided by duplex scan, magnetic resonance image or computed tomography can be performed, but with a significantly high recurrence rate (up to 22%) and should be reserved only for patients that do not have arterial occlusion and with healthy arterial wall[12]. The medium term follow-up shows disappointing results, presumably because this technique maintains the causal factor, which is the secreting tissue within the arterial wall[12]. The excision of the cyst alone, preferred by some centers, can be performed when there is no occlusion of the vessel, but with a significantly high recurrence rate (10.7%), mainly when the adventitial communication with the articular capsule is not identified and interrupted[4]. Considering that the great majority of the patients are young, with low surgical risk and with these higher recurrence rates, those options do not seem to be the best ones, although there are no studies that evaluate the best therapeutic alternative due to the small numbers of patients treated with this condition.
The definitive treatment of the lesion seems to be the conventional surgery, as performed at this case report, which consists in the removal of the stenosed segment as well as the cyst, followed by the interposition of a vein segment, preferably, for the arterial reconstruction. This procedure is fundamental on the presence of arterial occlusion or if there is macroscopic alteration of the arterial wall after the resection or emptying of the cyst[7,13]. This alternative has been preferred by the majority of the surgeons in order to treat this pathology[7], however there are some surgeons that defend the cystostomy as the best approach for non-occluded arteries[12]. The access to the popliteal artery depends on the location of the lesion (medial approach for distal and proximal segments of the artery and posterior approach for the medium segment). The interposition of a venous graft (short bypass), preferably of the saphenous magna vein, or the use of a vascular prosthesis (if the reconstruction is above the knee) has shown excellent results in long term follow-up, specially when used autogenous graft[13].
A review of 215 procedures of popliteal artery adventitial cyst correction reported a failure rate of 2.0% when venous graft was used and up to 18.2% when synthetic material was used[14]. In a recent publication of 2011, Rutt et al compiled 68 popliteal artery procedures in 61 patients since 1979 and observed that the most used technique was the arterial resection with venous interposition (20 cases – 1 failure), followed by resection of the cyst (13 cases – 2 failures), needle aspiration (8 cases – 1 failures), resection of the adventitia (8 cases), angioplasty (4 cases – 2 failures), arterial resection with prosthesis graft interposition (2 cases) and other less common techniques[15]. Another compilation of 2011 reviewed the two most used types of treatment in popliteal arteries from 1976 to 2009 and showed the best success (96%) is obtained when there is resection of the lesion followed by autogenous graft bypass. The cyst aspiration had a success rate of 85% while endovascular treatment of the three patients treated failed[13]. There are authors that defend that the endovascular treatment with or without stenting is not adequate in this circumstance. That premise is supported by the fact that it is an extrinsic arterial compression, with no intimal lesion, and that the cause of the stenosis or arterial occlusion would not be treated, resulting in a high rate of failure represented by restenosis or persistence of symptoms[7,13-15].
CONCLUSION
The popliteal artery adventitial cyst is a rare and therefore not much studied non-atherosclerotic disease, with a not well established etiopathology, but it should be always considered as a differential diagnosis for a recent onset intermittent claudication in young patients. To confirm the disease it is necessary to obtain an image study (MRI or duplex scan preferably) and it must be treated with interventional therapy. The open surgery approach with the resection of the cyst and bypass using an autologous conduit has excellent post-operative long term results, thus being the best option. For those reasons we presented and discussed one case with the classical presentation of this pathology, reviewing the disease concepts, that was managed with the conventional and most used surgical approach with an optimum outcome.
REFERENCES
[1] ATKINS, HJB; KEY, JA. A case of myxomatous tumor arising in the adventitia of the left external iliac artery. Br J Surg. 1947; 34: 246. [ Links ]
[2] LASSONDE J, LAURENDEAU F. Cystic adventitial disease of the popliteal artery. Am Surg 48:341, 1982. [ Links ]
[3] STALLWORTH JM, BROWN AG, BURGES GE, HORNE JB. Cystic adventitial disease of the popliteal artery. Am Surg. 1985; 5: 455ñ9. [ Links ]
[4] TSILIMPARIS, N; HANACK, U; YOUSEFI, S; et al. Cystic adventitial disease of the popliteal artery: An argument for the developmental theory. J Vasc Surg. 2007; 45: 1249-52. [ Links ]
[5] LINQUETTE M, MESMACQUE R, BEGHIN B, et al. Dégénérescence colloide de líadventice de líartère poplitée. Semaine Hôp (Paris) 43:3005, 1967. [ Links ]
[6] PATY, PSK; KAUFMAN, JL; KOSLOW, AR; CHANG, BB; et al. Adventitial cystic disease of the femoral vein: a case report and review of the literature. J Vasc Surg. 1992; 15: 214ñ7. [ Links ]
[7] LEVIEN, LJ. Nonatheromatous Causes of Popliteal Artery Disease. In Rutherford, RB. Rutherford: Vascular Surgery. Philadelphia. Elsevier. 6th ed. 2005. p. 1236-55. [ Links ]
[8] ISHIKAWA K, MISHIMA Y, KOBAYASHI S. Cystic adventitial disease of the popliteal artery. Angiology. 1961; 12: 357. [ Links ]
[9] MILLER A, SALENIUS JP, SACKS BA, GUPTA SK, SHOUKIMAS GM. Noninvasive vascular imaging in the diagnosis and treatment of adventitial cystic disease of the popliteal artery. J Vasc Surg 1997;26:715-20. [ Links ]
[10] LOFFROY, R; RAO, P; KRAUS, D; STEINMETZ, E. Use of 3.0-Tesla High Spatial Resolution Magnetic Resonance Imaging for Diagnosis and Treatment of Cystic Adventitial Disease of the Popliteal Artery. Ann Vasc Surg. 2011; 25: 385.e5-385.e10. [ Links ]
[11] ISHIKAWA K: Cystic adventitial disease of the popliteal artery and of other stem vessels in the extremities. Jpn Surg. 1987; 17: 221. [ Links ]
[12] DO DD, BRAUNSCHWEIG M, BAUMGARTNER I, FURRER M, MAHLER F. Adventitial cystic disease of the popliteal artery: percutaneous US-guided aspiration. Radiology 1997;203:743-6. [ Links ]
[13] BAXTER, AR; GARG, K; LAMPARELLO, PJ; MUSSA, FF; CAYNE, NS; BERLAND, T. Cystic adventitial disease of the popliteal artery: is there a consensus in management? Vascular. 2011; 19(3): 163ñ66. [ Links ]
[14] KHOURY, M. Failed Angioplasty of a popliteal artery stenosis secondary to cystic adventitial disease: a case report. Vasc Endovasc Surg. 2004; 38: 277-80. [ Links ]
[15] VAN RUTTE, PWJ; ROUWET, EV; BELGERS, EHJ; LIM, RF; TEIJINK, JAW. In Treatment of Popliteal Artery Cystic Adventitial Disease, Primary Bypass Graft not Always First Choice: Two Case Reports and a Review of the Literature. Eur J Vasc Endovasc Surg. 2011, 42: 347-54. [ Links ]
Author: Angelo Frankini, MD
24 de Outubro st, 838/611.
90510000, Porto Alegre, RS, Brazil.
Phone/fax number: (55) 51 3222.2716.
Cell number: (55) 51 9981.5528.
E-mail: angelofffcmpa@hotmail.com
Co-authors: Airton Delduque Frankini, MD, PhD
Email: frankini@terra.com.br
Tiago Frankini, MD
Email: tiagofrankini@terra.com.br














