Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.12 no.2 Lisboa jun. 2016
https://doi.org/10.1016/j.ancv.2016.01.007
CASE REPORT
Blue finger syndrome - case report*
Blue finger syndrome - a propósito de um caso clínico
Joana Ferreira a,*, Rui Ramosb, Pedro Sousab
a Angiologia e Cirurgia Vascular, Centro Hospitalar de Trás-os-Montes e Alto Douro/EPE, Portugal
b Radiologia, Centro Hospitalar de Trás-os-Montes e Alto Douro/EPE, Portugal
ABSTRACT
Blue Finger Syndrome is a manifestation of atheromatous embolization at the upper limb. It's a rare pathology, with risk of recurrence and tissue lose, which could be particular troublesome at the upper limb. The authors present a case of a Blue Finger Syndrome secondary to an atherosclerotic plaque in the right subclavian artery (which is an unusual location), cor-rected with a stent. The majority of authors consider that the embolization source should be corrected. If it is not corrected, there is a risk of re-embolization, which may threaten the limb viability. Endovascular treatment is safe and efficacious. Direct stenting, especially with closed stents design appear to be the safest technique to trap thrombi and prevent distal thrombus embolization.
Keywords: Blue finger syndrome; Endovascular treatment; Right subclavian artery
RESUMO
O Blue Finger Syndrome é uma manifestac¸ão da embolizac¸ão distal nos membros superiores. É uma patologia rara, com risco de recorrência e de perda tecidular, o que poderá ser particularmente grave no membro superior. Os autores apresentam um caso de um Blue Finger Syndrome, secundário a uma placa de aterosclerose na artéria subclávia direita (localizac¸ão esta particularmente rara) corrigida através da colocac¸ão de stent. A maioria dos autores considera que a fonte embólica deverá ser corrigida. A sua não correc¸ão poderá significar a recorrência do fenómeno, com risco de perda de membro. O tratamento endovascular tem-se mostrado seguro e eficaz. A colocac¸ão de stent (em particular de malhas fechadas) aprisiona a placa de aterosclerose, prevenindo a embolizac¸ão distal.
Palavras-chave : Blue finger syndrome; Tratamento endovascular; Artéria subclávia direita
Introduction
Blue finger syndrome (BFS) describes acute digital cyanosis secondary to microembolism from a proximal atheromatous source.1-3 Due to its lethality, the diagnosis should be promptly established and an aggressive treatment immediately initiated, in order to prevent recurrences.1-3 The authors present a case of a BFS secondary to an atherosclerotic plaque in the right subclavian artery.
Case report
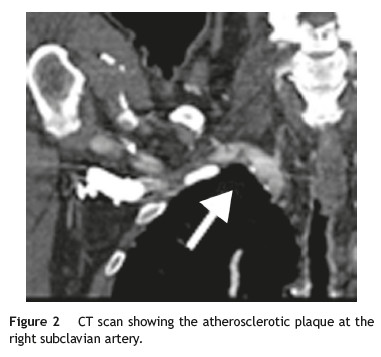
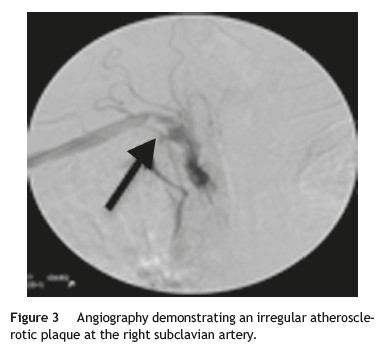
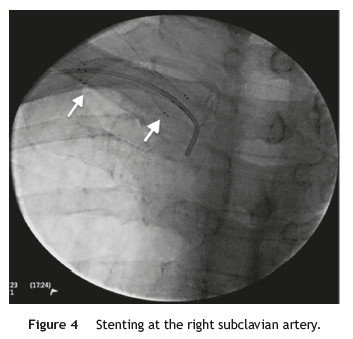
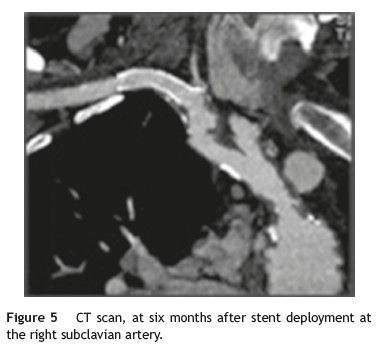
Male, 79 years old, smoker, was admitted with bluish discoloration of the distal phalanges in the right hand (Fig. 1). He denies any history of trauma, cold exposition, previous episodes of fingers color changes, weight loose and other constitutional symptoms. The humeral, radial and cubital pulses were present bilaterally with normal characteristics. No murmurs or bruits were audible. No neurologic sign or symptoms were recorded. There were no differences in the arterial pressure between the right and left upper limbs. He underwent a Doppler ultrasound which revealed an atherosclerotic plaque in the right subclavian artery. This result was confirmed with CT scan (Fig. 2). The CT scan did not show any skeletal or muscle anomaly. He also performed an electrocardiogram and posteriorly a transthoracic and transesophageal echocardiograms which were normal. No hematologic or prothrombotic abnormality was found. The patient was submitted to endovascular repair. Under local anesthesia, using a right humeral approach, a 7Fr Boston Scientific sheath, with 11 cm length was used in the right humeral artery. The plaque was crossed by a 0.035 J hydrophilic guide wire, then using a 0.035 stiff guide wire a self-expandable stent Cordis S.M.A.R.T.®CONTROL® (9 mm × 30 mm) was deployed (Figs. 3 and 4). The stent was posteriorly dilated. The patient was on double antiplatelet therapy during two months and chronically on aspirin and statin. Six months of the follow-up the patient is asymptomatic, without recurrences and the CT scan performed showed that the stent is patent without fractures (Fig. 5).

Discussion
BFS is a manifestation of atheromatous embolization at the upper limb.1,2 The embolization source could be central (which was excluded in this case) or peripheral (which is the consistent hypothesis in this report). Embolization can occur spontaneously, as in this case, or after an invasive vascular procedure.2,3 The majority of plaques associated with embolization is localized at the abdominal aorta and the iliofemoral arteries.2 The subclavian artery, particularly the right subclavian artery, is a rare source of embolization.1,2 Beside this, the embolization plaque is typically located at the ostium.4 However, in this case, the lesion was at the second part of the subclavian artery, which is quite unusual.
The underlying atheromatous lesion can be recognized as an area of intimal irregularity, which in some occasions may not, be hemodynamically significant.1 So, the patient may not complain of arm claudication and the only clinical manifestation of the atherosclerosis plaque could be skin changes.1 In this particular case, the lesion was not hemodynamically significant (there were no differences in the arterial pressure in the upper limbs, neither claudication complaints). The patient just complained about bluish discoloration in the distal phalanges. This clinical presentation could be explained by the morphologic characteristics of the atherosclerotic plaque which is irregular and hypodense, with embolization risk.
Beyond this, skin findings, in the BFS includes livedo reticularis, gangrene and ulceration.2
Skin changes are a reflection of microvascular ischemia, due to embolization. The embolic material occludes the small arteries and arterioles rather than the large superficial arteries, so distal pulses remain frequently palpable.2
Apart from this, clinical manifestations of embolization include constitutional symptoms (fever, anorexia, weight loss, fatigue and myalgias), signs of systemic inflammation (anemia, thrombocytopenia, leukocytosis, high erythrocyte sedimentation rate, elevated levels of C-reactive protein), which were not present in the case.2
As BFS is a manifestation of atherosclerosis, patients should be submitted to an aggressive medical therapy that includes smoking cessation, life style modification, blood pressure and diabetes control, hyperlipidemia management, aspirin, β-blockers, angiotensin converting enzyme inhibitors and statins.2
The treatment with thrombolytic or anticoagulation is not consensual, because they can precipitate distal embolization.2
In addition to these measures, it seems reasonable to correct the source of embolism, although there are no randomized trials comparing the medical treatment with invasive interventions (surgically or percutaneously) to eliminate the cause of embolism.1-3 Although, if the embolic source is not corrected, there is a risk of re-embolization, which may threaten the limb viability.1,2 The correction could be surgically or percutaneously.1,2
In this case reported, we decide to perform it percutaneously due to its less invasiveness when comparing to the surgical treatment.
Direct stenting, especially with closed stents design appear to be the safest technique to trap thrombi and prevent distal thrombus migration.4 It also stimulate the formation of a stable neointima and establish a normal flow.1 In this case we deployed the stent in the irregular and hypodense atherosclerotic plaque. We used a right brachial approach, which provides a greater stability and also a straightforward route which aids stent deployment.
Some authors suggest the use of a balloon to protect the vertebral artery and avoiding embolization or occlusion, which is really useful if the atherosclerosis lesion is close to the origin of the vertebral artery.1 In this particular case, we did not use it due to the location of the plaque, which was not near the vertebral artery origin.
Surgery to correct the proximal underlying source includes subclavian carotid transposition and carotid subclavian bypass with proximal ligation.1 This carry a perioperative death rate of 0-2% and a stroke rate of 1.0-3.0%.1 In addition, 1.0-2.0% of grafts become infected.1 Other complications reported are phrenic nerve injury, thoracic duct laceration and Horners syndrome.1
References
1. Gaines PA, Swarbrick MJ, Lopez AJ, et al. The endovascular management of blue finger syndrome. Eur J Vasc Endovasc Surg. 1999;17:106-10. [ Links ]
2. Saric M, Kronzon I. Cholesterol embolization syndrome. Curr Opin Cardiol. 2011;26:472-9. [ Links ]
3. Renshaw A, McCowen T, Waltke A, et al. Angioplasty with stenting is effective in treating blue toe syndrome. Vasc Endovasc Surg. 2002;36:155-9. [ Links ]
4. Pellerin O, Delorme L, Bellmann L, et al. Clinical presentation and percutaneous endovascular management of acute left subclavian artery thrombosis: report of two cases. Diag Interv Imaging. 2014;95:95-9. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflicts of interest
The authors have no conflicts of interest to declare.
Rua do Bolhão no. 268, 4505-314 Fiães VFR, Portugal. Tel.: +351 962 958 421.
E-mail address: joana222@hotmail.com (J. Ferreira).
Available online 31 March 2016
Notes
*Presented at the XV Congress of the SPACV 11 June 13, 2015














