Serviços Personalizados
Journal
Artigo
Indicadores
Links relacionados
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.13 no.3 Lisboa dez. 2017
ARTIGO ORIGINAL
Expanding the infrarenal aortic aneurysm repair to nonagenarians: the role of evar
Expandir o tratamento dos aneurismas da aorta abdominal infra-renal aos nonagenários: o papel do tratamento endovascular
Sérgio Teixeira1, Rui Machado1,2, Pedro Sá Pinto1, Rui Almeida1,2
1 Centro Hospitalar do Porto - Hospital Santo António
2 Instituto de Ciências Biomédicas Abel Salazar - ICBAS
Autor para correspondência
ABSTRACT
Introduction: Advanced age negatively impacts the outcomes of abdominal aortic aneurysm (AAA) repair. Nowadays, endovascular procedures enable vascular surgeons to treat elderly patients who cannot be submitted to open surgery.
Aims: We report our experience with endovascular aneurysm repair (EVAR) in nonagenarians.
Methods: We retrospectively reviewed our prospectively maintained aneurysm database in order to obtain records of all patients more than 90 years-old, who were submitted to EVAR over a 12 years period at our institution. Patients' comorbidities, functional status, aneurysm size, perioperative complications, endoleaks, reinterventions and long-term survival were recorded.
Results: 171 EVAR procedures were performed. Three (1,75%) nonagenarians underwent aneurysm repair (3 male; mean age 91.3 ± 1.25 years). Mean aneurysm diameter was 8.2 ± 1.68 cm with a median size of 8.1 cm (range 6.2–10.3 cm). There were 1.7 mean comorbidities per patient. Technical success rate was 100%. Mean hospital length of stay was 4.3 ± 0.47 days with a median of 4 days (range 4–5 days). Thirty-day mortality was 0%. Mean follow-up and mean survival were 28 months. There were no complications and all patients returned to their preoperative functional status. No endoleaks were identified on the follow-up imaging.
Conclusions: We have shown, in a small and carefully selected group, that EVAR is associated with good outcomes in nonagenarian patients.
EVAR is, in our opinion, the best treatment option for AAA in nonagenarians with good functional status.
Keywords: EVAR; abdominal aortic aneurysm; nonagenarians
RESUMO
Introdução: A idade avançada afeta negativamente os resultados do tratamento dos aneurismas da aorta abdominal (AAA). Atualmente, os procedimentos endovasculares permitem o tratamento de doentes idosos incapazes de suportar uma intervenção cirúrgica por via aberta.
Objetivos: Apresentar a experiência no tratamento endovascular dos aneurismas da aorta abdominal (EVAR) em doentes nonagenários.
Métodos: Realizou-se uma revisão retrospetiva, na nossa base de dados prospetiva de aneurismas, de todos os doentes com idade >90 anos submetidos a EVAR, na nossa instituição, num período de 12 anos. Foram estudadas as comorbilidades dos doentes, o estado funcional, o tamanho do aneurisma, as complicações peri-operatórias, as endofugas, as reintervenções e a sobrevivência a longo prazo.
Resultados: Dos 171 EVAR realizados, 3 (1,75%) foram em nonagenários (3 homens; idade média 91.3±1.25 anos). O diâmetro médio dos aneurismas foi 8.2±1.68 cm e a mediana 8.1 cm (6.2–10.3 cm). A média do número de comorbilidades por doente foi 1.7. A taxa de sucesso técnico foi de 100%. A duração média do internamento foi 4.3±0.47 dias e a mediana 4 dias (4–5 dias). A mortalidade aos 30 dias foi de 0%. Os períodos de seguimento/sobrevivência médios foram de 28 meses. Não se verificaram complicações e todos os doentes retornaram ao seu estado funcional prévio. Nos estudos imagiológicos de seguimento não foram identificadas endofugas.
Conclusões: Mostrámos, num pequeno grupo cuidadosamente selecionado de doentes nonagenários, que o EVAR se encontra associado a bons resultados.
Na nossa opinião, o EVAR é a melhor opção para o tratamento dos AAA em nonagenários com um bom estado funcional.
Palavras-chave: EVAR; aneurisma aorta abdominal; nonagenários
INTRODUCTION
Modern medicine has enabled us to live longer, healthier and more productive lives than ever before.(1) In Portugal, as in other developed countries, elderlies constitute the fastest growing segment of the population.
Cardiovascular disease is one of the most common causes of morbidity and mortality in the elderly population.(2) With increasing life expectancy, the number of nonagenarians with abdominal aortic aneurysms (AAA) that will potentially need intervention can be expected to rise.(3) Advanced age has been identified as one of the risk factors that negatively impacts the outcomes of AAA repair.(4)
Nowadays, endovascular procedures enable vascular surgeons to treat elderly patients who cannot be submitted to open surgery.(5) Over the last years, several studies on abdominal aortic aneurysm repair in nonagenarians have been published.(6–8) This less invasive approach to aortic aneurysmal disease has been associated with a substantial decrease in mortality and morbidity in this singular group of patients.(9)
In this work, we sought to analyze the results of our institution on endovascular aortoiliac aneurysm repair (EVAR) in a population more than 90 years-old, over a 12 years period.
METHODS
We retrospectively reviewed our prospectively maintained aneurysm database at Santo António Hospital in order to obtain records of all patients more than 90 years-old, who underwent elective AAA repair (EVAR and open repair) between December 2001 and December 2013.
Patients' comorbidities, preoperative and postoperative functional status, aneurysm size and technical success were recorded according to reporting guidelines from the Society of Vascular Surgery.(10)
Recorded comorbidities were: arterial hypertension — HTA; coronary artery disease — CAD; chronic kidney disease — CKD; chronic obstructive pulmonary disease — COPD; peripheral artery disease — PAD; hypercholesterolemia — HCL; malignancy; previous cerebrovascular accident — CVA.
Postoperative variables reviewed were: length of stay in intensive care unit (ICU); total hospital length of stay; perioperative complications; need for reintervention; aneurysm related need for readmission; 30-day morbidity and mortality. Follow-up was conducted at 30 days, 3 months, 6 months, 12 months and then annual visits, unless more frequent visits was indicated.
Categorical data was described using absolute numbers and percentages. Means (± standard deviation) and medians were used to analyze continuous variables.
RESULTS
During this study's period, 291 patients underwent elective infrarenal AAA repair at our institution. A total of 171 patients (58.8%) were submitted to EVAR. Regarding EVAR, patients' mean age was 74.1±8.9 years (range 38–93) and the mean maximum aneurysm diameter was 6.2±1.48 cm (range 2.5–1.06; median 6.0). Mean postoperative length of stay was 6.3±7.1 days and the overall 30-day mortality was 1.2%.
We identified 3 nonagenarians (1.75% of total treated patients) who underwent elective AAA repair. All cases were treated by EVAR (Table 1). All patients were male, with a mean age of 91.3±1.25 years-old. Mean aneurysm diameter was 8.2±1.68 cm with a median size of 8.1 cm (range 6.2 –10.3).
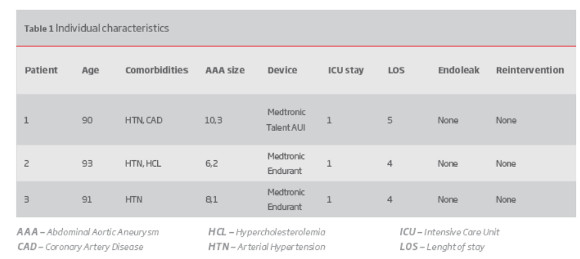
Patients had a good to excellent preoperative functional status, defined as performing all activities of daily living independently, and participating in daily exercise regimens. The average number of comorbidities per patient was 1.7 (range 1–2) and all patients classified III on American Society of Anesthesiologists physical status classification system.
In what concerns to technical aspects of the operative interventions, two patients were treated with a bifurcated device (Endurant; Medtronic AVE) and one patient was treated with an aorto-uni-iliac device (Talent; Medtronic AVE) and femoral-femoral bypass. Femoral access was obtained surgically in all patients, irrespective of arterial calcification. The type of endograft was chosen based on surgeon's preference and anatomic considerations. The aorto-uni-iliac device was used due to aortic tortuosity that contraindicated the use of a bifurcated device.
All the procedures were performed under spinal anesthesia.
Technical success rate was 100%. All patients stayed for 1 day on the ICU. Average hospital length of stay was 4.3±0.47 days with a median of 4 days (range 4–5). Thirty-day mortality was 0%. Mean follow-up and mean survival were 28 months (range 24–34). One patient died at 34 months after EVAR from cardiac causes. There were no complications and all the patients returned to their preoperative functional status after discharge. No endoleaks were identified on the follow-up angio-CT scan. Renal function remained stable in all patients during follow-up.
DISCUSSION
Abdominal aortic aneurysms repair remains a significant cause of morbidity and mortality among general population.(11) Over the past decade, technological advances have resulted in a shift towards EVAR as a safe and effective alternative to open aneurysm repair.(5)
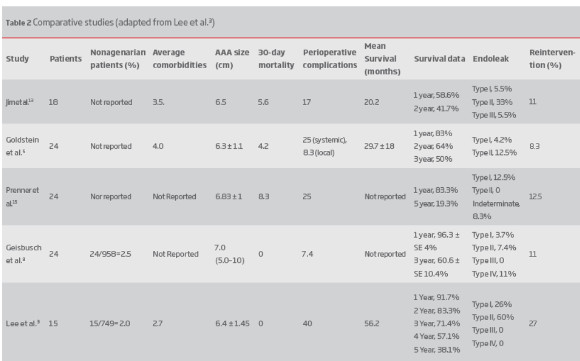
Several studies with a small number of patients, regarding EVAR in the nonagenarian population, have been published over the last years in the literature (Table 2).(3,5–8,12–15)
Here we report a small series of nonagenarian patients who underwent elective EVAR. A total of 3 highly selected patients with good functional status were treated. Technical success was 100% and 30-day mortality was 0%. We didn't register any post-operative complications or deaths.
Complication rates are higher in elderly patients. In the literature, local and systemic complication rates, after EVAR and among nonagenarian patients, are 8.3 to 22% and 17 to 25%, respectively.(5,13,14) A report by Lee et al. documented 40% of morbidity, mainly due to access site complications with the use of early generation endografts.(3)
Tsilimparis et al. showed a substantial difference in 30-day post procedure survival of patients according to their age. Thirty day mortality in elective AAA repair was 5,5% (open repair: 18.8%; endovascular: 3.8%) for nonagenarians compared with 3.1% (open repair: 7.4%; endovascular: 2.0%) for octogenarians, and 2.1% (open repair: 3.9%; endovascular: 1.2%) and 1.1% (open repair: 1.9%; endovascular: 0.5%) for patients 65 to 79 years and younger than 65 years, respectively. The increased risk of death with advanced age persisted when comparing endovascular and open repair.(12)
Angio-CT is the preferred imaging technique for the follow-up in our institution, irrespective of the patient's age. We detected no endoleaks during the follow-up period in the present series. Literature reports an incidence of 4.2 to 26% and 11% to 60% for type 1 and type 2 endoleaks, respectively.(3,5,13,14) The relatively high type 1 and type 2 endoleak's rate described in the literature can be explained by the use of older generation devices (in earlier series) and by elderly aortic anatomy (tortuous aorta with larger neck sizes and/or greater neck angulation).(3,5,8,15)
Comorbidities analysis revealed that our patients were healthier when compared to patients from previous studies. Our group of nonagenarians had an average of 1.7 comorbidities per patient when compared with previously reported averages of 2.7, 3.5 and 4.(3,5,13)
Goldstein et al. showed an inverse correlation between the number of perioperative comorbidities and long-term postoperative survival. This correlation was particularly
important in patients with more than 5 comorbidities.(5) Timaran et al. reported a higher in-hospital mortality rate among patients with “the most severe comorbidities”.(16) All of our patients had <3 comorbidities and this may explain the favourable outcomes presented in this series.
Another contributing factor for the positive outcomes was the use of loco-regional anesthesia. Although local anesthesia is simple and safe, loco-regional anesthesia, according to our experience, is preferable because it allows better pain control.(17) Consideration must be given to the use of general anesthesia in older patients.(5)
There are several limitations to our study. The small sample (3 patients) restricts us to a descriptive analysis. As a retrospective study, a sample selection bias may occur, as we don't know the number of nonagenarian patients, with AAA, who were not treated. Our cohort may represent a preselected group, which is healthier and more suitable for EVAR than the overall group of nonagenarians presenting with AAA.
New available low profile devices on the market might make EVAR safer. Percutaneous route for EVAR with local anesthesia protocols may also contribute for better results in elderly patients.(17,18)
We have shown, in a small and carefully selected group of nonagenarian patients, that EVAR is associated with good outcomes.
In our opinion, EVAR is the best option for the treatment of AAA in nonagenarians with good functional status.
REFERENCES
1. Manton KG. Recent declines in chronic disability in the elderly U.S. population: risk factors and future dynamics. Annu Rev Public Health. 2008;29:91–113. [ Links ]
2. Heron M, Hoyert DL, Murphy SL, et al. Deaths: final data for 2006. Natl Vital Stat Rep 2009. 2009;57(14):1–134. [ Links ]
3. Lee GK, Ullery BW, Lee JT. Elective EVAR in nonagenarians is safe in carefully selected patients. Ann Vasc Surg. 2014;28(6):1402–8. [ Links ]
4. Norman PE, Semmens JB, Lawrence-Brown MM, Holman CD. Long term relative survival after surgery for abdominal aortic aneurysm in western Australia: population based study. BMJ. 1998;317(7162):852–6. [ Links ]
5. Goldstein LJ, Halpern JA, Rezayat C, et al. Endovascular aneurysm repair in nonagenarians is safe and effective. J Vasc Surg. 2010;52(5):1140–6. [ Links ]
Correio eletrónico: sergiodavide@hotmail.com (S.Teixeira).
Recebido a 08-08-2017;
Aceite a 25-10-2017;














