Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Angiologia e Cirurgia Vascular
Print version ISSN 1646-706X
Angiol Cir Vasc vol.14 no.3 Lisboa Sept. 2018
ARTIGO ORIGINAL
Helicobacter pylori and the atherogenic process in cardiovasculardisease
Helicobacter pylori e o processo aterogénico na doença cardiovascular
Nuno Carvalho1,2, Ana Cóias3, Hélder Coelho3, Gisela Marcelino4, Diogo Albergaria1,2, Maria José Ferreira5, Maria José Brito3, João Corte Real1,2, Paulo Matos Costa1,2
1 General Surgery Department, Hospital Garcia de Orta, Almada, Portugal
2 Surgery 1, Curricular Unity , Lisbon Medical School, Lisbon, Portugal
3 Pathology Department, Hospital Garcia de Orta, Almada, Portugal
4 Medical office of Dr. Eichenberger, general practitioner, Marly, Switzerland
5 Angiology and Vascular Surgery, Hospital Garcia de Orta, Almada
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Background: Conventional risk factors do not explain completely the atherogenic process. Chronic Helicobacter pylori (HP) infection may cause arterial inflammation and has been epidemiologically linked to the occurrence of atherosclerosis. Studies about the association of HP infection with peripheral arterial disease are limited.
Objective: Evaluate the presence of HP using a monoclonal antibody anti-HP in the atherosclerotic plaques of the superficial femoral artery in patients submitted to amputation above-knee.
Material and methods: We searched for the presence of HP in 29 non-consecutive patients with Leriche-Fontaine grade IV lower limb ischemia, submitted to amputation above-knee. Femoral artery was isolated and an atherosclerotic plaque specimen immediately distal to the amputation level, was removed, fixed in formalin and evaluated for HP, using a mono clonal antibody, anti-HP.
Results: The mean age of the 29 patients was 82 years. 18 were men (62.1 %). Risk factors for cardiovascular disease were present in the majority of patients. Only one patient had known history of HP infection in the past. Morbidity rate was 30%. The mortality rate was 13.8 % (4 cases). In all cases, anti-HP showed no evidence of HP at the atherosclerotic plaque.
DiscussionlConclusion: HP infection has been associated both epidemiologically and pathogenetically with atherosclerosis. However, HP was not found in this study at the atherosclerotic plaques of the superficial femoral artery.
Keywords: Helicobacter pylori, atherosclerosis, arterial inflammation, cardiovascular risk factors
RESUMO
Introdução: Os factores de risco cardiovasculares não explicam completamente o processo aterogénico. A infecção crónica a Helicobacter pylori (HP) poderá provocar inflamação arterial e está epidemiologicamente ligada ao processo de aterosclerose. Pouco se sabe sobre o papel do HP no processo de aterosclerose, os estudos sobre a associação entre a infecção a HP e doença arterial periférica são limitados.
Objetivo: avaliar a presença de HP através de anticorpo monoclonal anti-HP em placas de aterosclerose da artéria femoral superficial de doentes submetidos a amputação acima do joelho.
Material e métodos: Foi avaliada a presença de HP em 29 doentes não consecutivos com isquémia do membro inferior Leriche-Fontaine grau IV submetidos a amputação acima do joelho. Isolou-se a artéria femoral superficial e recolheu-se um fragmento de placa aterosclerótica imediatamente distal ao nível de amputação. O espécimen foi fixo em formol e avaliada a presença de HP utilizando um anticorpo monoclocal anti-HP.
Resultados: A mediana da idade dos 29 doentes é 82 anos. 18 são do sexo masculino (62,1%). A maioria dos doentes apresentava factores de risco cardiovasculares. Apenas um doente tinha história pessoal de infecção a HP. A morbilidade foi de 30% e a mortalidade 13,8% (n=4). Não se verificou a presença de HP na placa aterosclerótica através do anticorpo monoclocal anti-HP.
Discussãol Conclusão: A infecção a HP tem sido associada epidemiologicamente ao processo de aterosclerose. Contudo, neste estudo, não se identificou a presença de HP na placa de aterosclerose na artéria femoral superficial.
Palavras-chave: Helicobacter pylori, aterosclerose, inflamação arterial, factores de risco cardiovasculares
Introduction
Atherosclerosis is a highly prevalent chronic inflammatory condition and is currently the chief cause of morbidity and mortality in developed countries(1). Many risk factors are involved in its development, including hyperlipidemia, hypertension, diabetes mellitus and smoking(1). These risk factors cannot completely explain formation, progression and stabilization of atherosclerotic plaques, but only clarify some of its aspects(2). In fact, in about half of the patients with atherosclerosis, conventional risk factors cannot explain the occurrence of the disease(3).
This observation indicates that additional, and yet undetected risk factors contribute to the development of atherosclerosis(3).
Inflammatory and immunological processes triggered by viral or bacterial infections can be the underlying cause of the atherosclerotic process, the so called «response to the lesion» theory(4).
Helicobacter pylori (HP) is a gram-negative microaerophilic spiral bacterium that occurs naturally and inhabits the mucous layer that covers the gastric epithelial cells. It is the most prevalent infection in the world, affecting approximately 50% of the worlds population and considered the causative agent of many gastrointestinal and extradigestive conditions(5). Chronic HP infection may cause arterial inflammation and has been epidemiologically linked to the occurrence of coronary artery disease and atherosclerosis(1). Studies about the association of HP infection with peripheral arterial disease are limited(6). Is HP a New Cardiovascular Risk Factor?(4)
Objective
Evaluate the presence of HP using a monoclonal antibody anti-HP in the atherosclerotic plaques of the superficial femoral artery in patients with grade IV lower limb ischemia, submitted to amputation above-knee.
Material and Methods
We searched for the presence of HP in 29 non-consecutive patients in superficial femoral artery plaque specimens obtained in patients with Leriche-Fontaine grade IV, classification scheme of peripheral arterial disease, ulcer or gangrene, submitted to amputation above knee(7). Femoral artery was isolated and an atherosclerotic plaque specimen of approximately 0.5-1 cm, immediately distal to the amputation level, was removed, fixed in formalin, and evaluated for HP, using a mono clonal antibody, anti-HP. All the specimens were obtained in the operating room under sterile conditions(2). The detection of HP was performed by immunocytochemistry, with the detection system "Optiview DAB IHC Detection Kit", Ventana (Roche). The primary antibody was anti-Helicobacter pylori (SP48), Ventana, Roche. Antigen recovery buffer elevated pH (CC1 40 min - 97ºC). Slide strainers were visualized by light microscopy. Gastric mucosa was used as a control.
The design of this study was approved by the Ethics Committee of Garcia de Orta. Hospital. Informed consent was obtained for all patients.
Risk factors for atherosclerosis were registered: arterial hypertension, diabetes, smoking, ischemic heart disease, previous cardio-vascular events, HP status, if previously know, blood lipids and previous amputation(1,8).
Patients were defined as hypertensive if they had a diastolic blood pressure > 90 mmHg, a systolic blood pressure > 140 mmHg or had been treated with antihypertensive therapy for at least 1 year. Patients were classified as diabetic if they had been treated with antidiabetic drugs for at least 1 year. Patients were defined as smokers if they reported smoking more than ten cigarettes daily for at least 1 year during the 10 previous years. Hypertriglyceridemia was defined as triglyceride levels >200 mg/dL, and finally, hyperlipidemia was considered if total cholesterol level was > 220 mg/dl or if they had been treated with lipid-lowering drugs for at least 1 year(1,9).
The statistical analysis was performed with SPSS Statistics 20.0 for Windows. Variables were assessed for a parametric distribution with Shapiro-Wilk test. This test showed that the variables of this study follow a non-parametric distribution. Therefore, the results are shown as median (interquartile interval) for continuous variables. As to qualitative variables, the results are shown as number (valid percentage) of subjects. In addition, the results were considered statistically significant if P<0.05.
Results
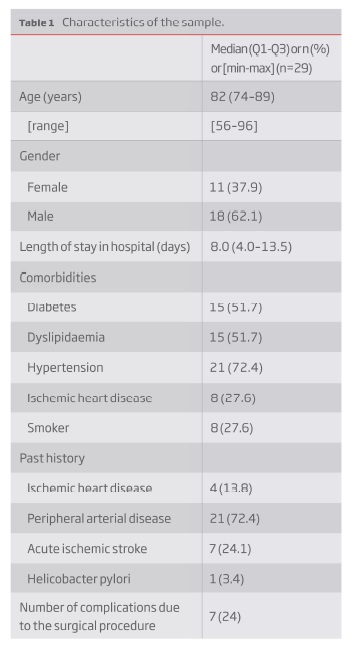
The demographic data af the patients in the study group are shown in Table 1.
Results are expressed as median (Q1-Q3) for non-parametric quantitative variables and number (percentage) of individuals for qualitative variables. Range [minimum-maximum] is also mentioned for age.
The mean age of the 29 patients was 82 years and 18 of them were men (62.1 %). The median of the length of the hospitalization was 8 days. Risk factors for cardiovascular disease were present in the majority: 72% had a history of hypertension, 52% had dyslipidemia, 28% were recent or former smokers and 19% had diabetes. Only one patient had known history of HP infection in the past.
In their past history, the majority had known peripheral arterial disease (72.4 %), ischemic stroke (24.1%) and ischemic heart disease (13.8 %). Morbidity rate was 24% due to 3 pneumonia, 2 stump infection and 2 stump hemorrhage. Mortality rate was 13.8 % (the equivalent of 4 cases) - data not shown.
In all cases anti-HP showed no evidence of HP at the atherosclerotic plaque.
Discussion
It is known that the traditional risk factors, for example, in the case of ischemic stroke do not explain all the clinical and epidemiological features of the atherosclerotic disease(10). A large body of evidence indicates that the inflammatory processes in the vascular wall are the decisive factors that account for the rate of lesion formation and clinical development in patients(11). The study of atherosclerosis has taken new directions, one of the most intriguing of these being the infectious theory of atherosclerosis that has been addressed in recent years.
Epidemiological studies have suggested a role of infections in the pathogenesis of atherosclerosis and bacterial DNA and viral structures have been identified in atherosclerotic lesions(8). Several serological studies indicate a significant association of HP with atherosclerotic disease, even after adjustment for risk factors(11).
Studies about the association of HP infection with peripheral arterial disease are limited. In a recent review article on HP and atherosclerosis only a brief reference was made on arterial peripheral disease and HP, due to the scarce studies on the subject(6). In a recent study HP rods were successfully isolated from 6.4% of atherosclerotic plaques from 31 femoral arteries and from 5.0% of samples from 20 iliac arteries. The authors concluded that HP rods remain viable in atherosclerotic plaques, which enables successful culturing on special media under microaerophilic conditions(12).
Several methods have been used for the detection of HP in atherosclerotic plaques, with conflicting results. Some studies have been performed using the polymerase chain reaction (PCR) for HPs ADN detection in the tissues analyzed. Still, they are very few and the results are contradictory. Immunohistochemistry (which was used in this study) is accepted as the gold standard method for the detection of HP in tissues and its sensibility and specificity is near 100 %(13).
To the best of our knowledge, our study is the first one where a mono-clonal antibody is used for the detection of HP in atherosclerotic plaques of the superficial femoral artery in patients with grade IV lower limb ischemia.
However, in our study no HP was identified at the atherosclerotic plaques. We can have several explanations for this result. One can be related to the mean age that was 82 years. Of note that in other studies where HP was found at the atherosclerotic plaques, the samples had younger patients and the arterial location and the methodology were different. Possible association of HP and arterial stiffness tends to be higher in younger subjects, whereas in the elderly, arterial stiffness is more often due to aging. So, it is possible that HP will not be found in aged populations, as it was the case in this study. Bloemenkamp et al. suggested that H. pylori infection was a risk factor for peripheral arterial disease in young women population(3).
Our study sample only includes patients with very advance stages of atherosclerotic disease, which needed amputation. In this patients the disease arteries are occluded, calcified, with no inflammatory activity, patients have ulcer or gangrene, the end stage of peripheral arterial disease. Therefore, it is possible that at this stage, the HP is no longer viable. Even so all, but one of our group of patients have not done the formal therapy for HP in the past, they were admitted with isquemic lesions or ulcers, submitted to antibiotic therapy and gastric protection in the moment of admission. This could interfere with the findings in the plaque.
Several mechanism related HP with atherosclerosis : induction of inflammatory response by circulating cytokines, secondary to chronic infectious state, endothelial damage, chronic low grade activation of coagulation cascade, low antioxidant levels, dysregulation of lipid metabolism resulting in increased total cholesterol and triglyceride levels and reduced high density lipoprotein levels and hyperhomocysteinaemia(3,5,6).
It is also known that HP can be found in the endothelial cells, although its presence is not required for atherosclerosis induction due to the hypothesis of molecular mimicry, where antibodies against an infective agent can cross react with structure of the organism, and inflammatory mediation(3,14). But this was not the objective of the present study as we studied specifically the atherosclerotic plaque.
The first Kochs postulate, postulates that a germ, should always be found microscopically in the bodies of animals having the disease and in that disease only; it should occur in such numbers and be distributed in such a manner as to explain the lesions of the disease(15). This is not the case of this study, as the HP was not identified in atherosclerotic plaques, and it does not seem to be an etiological agent in atherosclerosis, at least by direct local action.
Conclusion
No HP was found using a monoclonal antibody anti-HP in atherosclerotic plaques at superficial femoral artery in patients submitted to amputation above-knee. As the patients age seem to have an important impact on the results, we recommend that future research on this subject should be done with younger patients.
BIBLIOGRAPHY
1. Sawayama Y, Hamada M, Otaguro S, Maeda S, Ohnishi H, Fujimoto Y et al. Chronic Helicobacter pylori infection is associated with peripheral arterial Disease. J Infect Chemother (2008) 14:250-254 [ Links ]
2. Kaplan M, Yavuz SS, Cinar B, Koksal V, Kut MS, Yapici F et al. Detection of Chlamydia pneumoniae and Helicobacter pylori in atherosclerotic plaques of carotid artery by polymerase chain reaction. International Journal of Infectious Diseases (2006) 10, 116-123 [ Links ]
3. Bloemenkamp DG, Mali WP, Tanis BC, Rosendal FR, van den Bosch MA, Kemmeren JM et al. Chlamydia pneumoniae, Helicobacter pylori and cytomegalovirus infections and the risk of peripheral arterial disease in young women. Atherosclerosis 163 (2002) 149_/156. [ Links ]
4. Martínez AT and Martínez MG. Helicobacter pylori: a New Cardiovascular Risk Factor? Rev Esp Cardiol 2002;55(6):652-6 [ Links ]
5. Hamed SA, Amine NF, Gala GM, Helal SR, Tag El-Din, Shawky OA et al. Vascular Risks and Complications in Diabetes Mellitus: The Role of Helicobacter Pylori Infection. Journal of Stroke and Cerebrovascular Diseases, Vol. 17, No. 2 (March-April), 2008: pp 86-94 [ Links ]
6. Vijayvergiya R, Vadivelu R. Role of Helicobacter pylori infection in pathogenesis of atherosclerosis. World J Cardiol 2015 March 26; 7(3): 134-143 [ Links ]
7. Varu VN, Hogg ME, Kibbe MR. Critical limb ischemia. J Vasc Surg 2010;51:230-241 [ Links ]
8. Blasi F, Denti F, Erba M, Cosentini R, Raccanelli R, Rinaldi A et al. Detection of Chlamydia pneumoniae but Not Helicobacter pylori in Atherosclerotic Plaques of Aortic Aneurysms. Journal of Clinical Microbiology, Nov. 1996, Vol. 34, No. 11 p. 2766-2769 [ Links ]
9. Shmuelya H, Passarob DJ, Vaturic M, Sagie A, Pitlik S, Samra Z et al. Association of CagA+ Helicobacter pylori infection with aortic atheroma. Atherosclerosis 179 (2005) 127-132 [ Links ]
10. Grau AJ, Buggle F, Lichy C, Brandt T, Becher H and Rudi J. Helicobacter pylori infection as an independent risk factor for cerebral ischemia of atherothrombotic origin. Journal of the Neurological Sciences 186 2001. 1-5 [ Links ]
11. Ludewig B, Kreb P and Scandella E. Immunopathogenesis of atherosclerosis. J. Leukoc. Biol. 76: 300-306; 2004. [ Links ]
12. Kedzia A, Ciecierski M, Wierzbowska M, Kufel A and Kwapisz E. Isolation of Helicobacter pylori from femoral or iliac atherosclerotic plaques. Acta Angiol 2010; 16, 3: 129-134 [ Links ]
13. Kacar F, Çulhac N, Yukselen V, Meteo, E Dikicio and E Levi. Histologic demonstration of Helicobacter Pylori in gastric biopsies : Witch is the best staining method. The Internet Journal Pathology. 2004 Vol 3 N 1.
14. Birnie DH, Holme ER, McKay IC, Hood S, McColl KE and Hillis WS. Association between antibodies to heat shock protein 65 and coronary atherosclerosis. European Heart Journal (1998) 19, 387-394. [ Links ]
15. Lynch NA. Helicobacter pylori and Ulcers: a Paradigm Revised. Federation of American Societies for Experimental Biology. http://www.faseb.org/opar [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: diogo.albergaria@gmaiLcom (D. Albergaria),
Recebido a 31 de outubro de 2017
Aceite a 14 de agosto de 2018