Introduction
Abdominal aneurysm repair suffered tremendous transformation over the last decades, due to the appearance and development of endovascular techniques. Endovascular repair of aortic aneurysms has allowed for faster and safer treatment of patients with high surgical risk and is currently widely established, as a simpler and less invasive solution. However, anatomical limitations remain an important disadvantage to the endovascular approach. Iliac arteries involvement in abdominal aortic aneurysm disease is reportedly as high as 40%1, therefore, aorto-iliac aneurysms pose a challenge, regarding distal sealing. A frequent solution and classical approach to this problem is extending the iliac limb to the external iliac artery (EIA) with occlusion of the internal iliac artery (IIA). This may lead to varying degree of pelvic ischemia, from buttock claudication and peripheral nervous damage to critical life-threatening ischemia, with rates as high as 55%2,3,4 in some series and causing significant morbidity 5-7
Iliac branched devices (IBD) allow for the creation of distal landing zones in the EIA and IIA, maintaining antegrade pelvic perfusion and excluding iliac artery aneurysms, while considerably diminishing the risk of ischemic complications. In this modern setting of endovascular surgery, they are becoming increasingly used for treatment of aneurysm disease.8
The aim of the present study is to evaluate clinical and technical results of the application of IBD in our center,
Methods
This study followed the reporting guidelines from the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) Statement for cohort studies. (von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014 Dec;12(12):1495-9. doi: https://doi.org/10.1016/j.ijsu.2014.07.013.)
An observational, descriptive, single-centre, retrospective cohort study was performed, form January 2008 to December 2020.
All consecutive patients submitted to endovascular repair of isolated iliac or aorto-iliac aneurysm in which an IBD was used were included. We included all patients with implantation of IBD irrespective of the type of adjunctive aortic repair or other procedures performed. There was no restriction regarding instructions for use compliance, diagnosis, extension of the aneurysm or the aortic repair.
Patients submitted to other techniques such as “coil and cover”, open repair, parallel grafts or bell-bottom were excluded if at least one iliac was not treated with an IBD.
Patient identification was retrieved from the operating room log and the remaining data obtained from the hospital records. Imaging data regarding pre, intra-operative and post-operative imaging was obtained from the hospital imaging database.
Data regarding pre-operative diagnosis, previous abdominal surgery and planned procedure were collected. Pre-operative CTA’s were measured to evaluate vessel diameter, patency and seal endpoints. Systematic description of procedure and endoprosthesis characteristics and dimensions was obtained. Medication prescribed at time of discharge was obtained, to evaluate for the institution of simple or dual antiplatelet therapy or anticoagulation.
Technical success was defined as correct implantation of the IBD with confirmed patency of both EIA and IIA. We included all patients where at least one IBD was deployed, irrespective of additional procedures.
In hospital logs were consulted with recovery of data regarding post-operative complications, namely stroke - with neurological signs and CT scan lesions; myocardial infarction (MI) - with clinical signs and myocardial enzymes elevation; acute kidney injury (AKI), defined as urinary output bellow 0,5mL/kg/h or an increase in at least 1.5x basal serum creatinine (AKIN I AKI); intestinal ischaemia, with endoscopic, CTA and/or operative confirmation; and paraparesis, with documented de novo motor deficit. In ambulatory, appointment logs were consulted and data regarding gluteal claudication, atheroembolism or lower limb claudication was collected. Re-evaluation CTA’s were evaluated, and recovered data regarding vessel diameter after surgery, presence of endoleak, limb kinking or occlusion. In hospital mortality and attributed cause was registered. We also consulted al patients records to establish, in every case, if patients had passed since their last evaluation. Time from surgery to most recent imaging control and appointment was evaluated.
We performed a descriptive analysis of our data. Continuous variables are presented as mean (standard deviation) if normally distributed and median (minimum-maximum) if not. Dichotomous and categorical variables were expressed in numbers (percentage). Mann-Whitney test was used when comparing continuous variables and Chi-Square/Fisher’s exact test to compare dichotomous variables. All analyses were considered statistically significant if a two-tailed p-value < 0.05 was observed. Statistical analysis was carried out using STATA 16 (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC).
Results
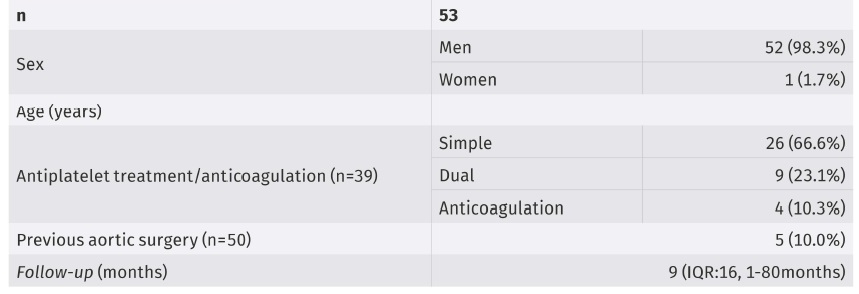
A total of 54 patients were initially analyzed, of which only 53 were finally included. One patient was excluded due to inability to catheterize the IIA, which didn’t allow for the deployment of the IBD. , Fifty-two were men (98.2%), with a mean age of 73.5 years (SD 8.1) (table 2). Mean aortic diameter was 56.4mm (SD 13.4), mean CIA aneurysm diameter 37.0mm (SD 12.7) .
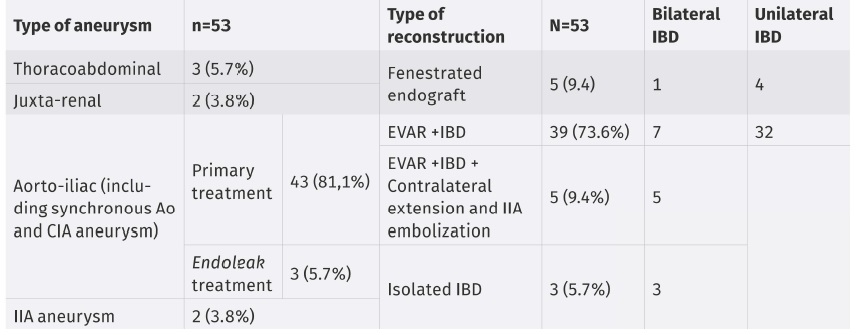
Of the patients included in this study, 3 had type III thoracoabdominal aneurysms, 2 juxta-renal abdominal aortic aneurysms, 43 aorto-iliac aneurysms, 2 IIA aneurysms and 3 previous EVAR procedures with type Ib endoleaks.
A total of 60 IBD’s were performed. In all patients, the COOK® Medical’s Zenith Iliac Branch Device (straight branch)-ZBIS device was used.
Only 3 patients were treated with isolated IBD, of which 1 presented type Ib endoleak form a previous EVAR procedure and 2 presented Common Iliac Artery (CIA) aneurysms, both with previous procedures for repair of aortic aneurysms. Of the remaining 50 patients, 5 were submitted to complex aortic treatment with fenestrated endografts, 32 to EVAR with unilateral IBD, 7 to EVAR with bilateral IBD, 5 to EVAR with unilateral IBD and contralateral extension to the EIA with embolization of the IIA and 1 to EVAR with unilateral IBD and embolization of an IIA branch. In total, sixteen patients were treated with bilateral IBD, the remaining thirty-seven with unilateral IBD (table 2). IBD’s were used in patients with CIA and IIA aneurysms, with arterial diameters over 25mm in the CIA (unfit for bell-bottom), younger patients with long life-expectancy after procedure, and low to moderate surgical risk patients, fit for longer and more complex surgical procedures.
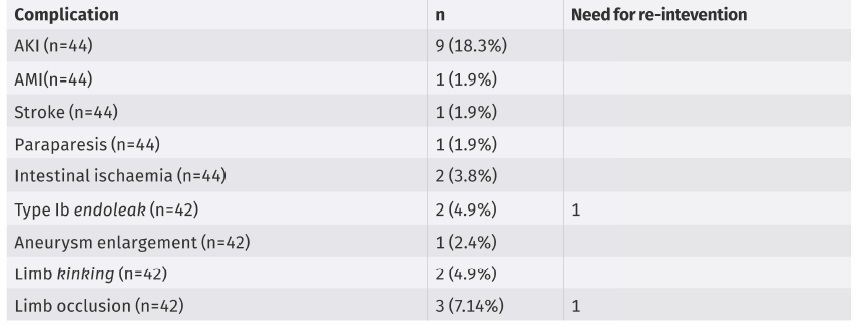
The technical success rate was 98.1%. The rate of peri-operative complications was 24.5%, mostly minor and transitory. These included AKI (18.3% - 8/44), paraparesis (1.9%), intestinal ischemia (3.8%, one of which transitory), one embolic intra-operatory stroke (1.9%) and one acute MI (1.9%). There were no mention of events of buttock claudication or atheroembolism. It was not possible to obtain data regarding erectile/sexual dysfunction.
Median follow-up was 9 months (IQR:16, 1-80months), with several losses to follow-up over time, during which 4.9% (2/42) developed type IB endoleaks, 4.9% (2/42) iliac aneurysm enlargement, 2.4% (1/42) limb kinking, 4.9% (2/42) limb occlusion, with a 7.14% (3/42) re-intervention rate. Of these, one was re-operated for endograft infection, with replacement of the endograft, one had acute limb occlusion and was submitted to lower limb thrombectomy and femoro-femoral bypass and one presented a type Ib endoleak with aneurysm enlargement, having been submitted to extension of the external iliac artery limb (table 3).
We found no association between limb patency and antiplatelet treatment (single or dual) or anti-coagulation (p=0.6).
There was no significant difference in AKI incidence between bilateral or unilateral IBD (irrespective of contra-lateral procedure - embolization of IIA or no intervention).
There was one case of in-hospital death due to post-operative MI (1.9%). The overall mortality of 17% (9/53), all caused by concurring conditions, unrelated with aneurysmal disease or treatment.
Discussion
The main findings in the analysis of our series were that, in the evaluated time span we were able to treat a significant amount of patient, with high technical success rates, high limb patency few endoleaks and a very low rate of re-intervention.
In previous large series, endoleak rates related to IBD appear to be low with 3% of patients with iliac-related endoleak at 5 years in Wong et al9, 76% at 109 months in Loth e al10, a freedom of iliac-related reintervention rate of 81% at 5 years in Parlani et al11 and 75% in Loth et al.
Sacrificing the internal iliac artery in favor of adequate sealing in endovascular repair of aorto-iliac aneurysms has long been accepted and practiced in vascular surgery. Risks include buttock claudication, erectile/sexual dysfunction, ischaemic colitis and buttock/pelvic necrosis7,12. The complications associated to loss of hypogastric perfusion, therefore, range from debilitating conditions to severe, life-threatening disease. These complications, however, range in frequency over several series and are mostly associated to loss of both IIA or sacrifice of an internal iliac artery in an already poorly perfused territory.
The choice to preserve the IIA is limited by anatomy and surgeons’ experience but is increasingly widespread since the introduction of iliac branched devices.
At our hospital, in a span of 12 years, a total of 53 patients were treated using this technique, with good results regarding the primary outcome of pelvic ischeamic complications and also adequate seal and technical complications. The most common complications were, in fact, not related to these outcomes but to secondary medical lesion following endovascular procedures, namely AKI, probably associated with increased contrast doses and surgical times, which we were unable to assess in our analysis of patient logs. Most complication related to the procedure itself did not warrant further surgical treatment. Complications such as limb occlusion, kinking or endoleak happened in 7 of 42 patients (16%) and consequent need for re-intervention, though considerable in the group of patients with complications, was minimal in the overall cohort, although the accuracy of our data may be limited by losses to follow-up and widely different follow-up time throughout the cohort.
Our series reflects a real world population, since our center receives refferals form primary care and hospital care physicians, irrespective of type of vascular disease and center differentiation. Another strength of this study is the systematic use of the same platform in every patient, across all surgeons in our department. However, we find an important limitation in our follow-up periods, many patients have been lost to follow up over time, some very early, resulting in extremely heterogeneous logs and unavailability of information, which means, although overall mortality and mortality associated with aneurysm disease appears to be low, our long term success rates may be lower than evidenced in this analysis.
Conclusion
IBD are an effective alternative for treatment of aneurysm disease in the aorto-iliac sector, either isolated or as part of a more complex procedures, allowing adequate seal and preservation of pelvic perfusion, with important reduction of extremely limiting complications. When adequately planned and executed, there appears to be no increase in loss of seal over time, though follow up period are still short. Follow up programs, systematized and organizes throughout the vascular surgery department is paramount for adequate follow up of patients and for a true perspective of results.