Original article
Venaseal: a good solution in the treatment of severe superficial venous insufficiency in very elderly patients
Venaseal: uma boa solução no tratamento da insuficiência venosa superficial grave em doentes muito idosos
Marta Machado1
2
3
Miguel Machado1
2
3
Arlindo Matos1
2
3
4
Rui Machado1
2
3
4
1 CUF Viseu; Portugal
2Luz Arrábida; Portugal
3Hospital de Riba de Ave; Portugal
4Centro Hospitalar Universitário do Porto, Portugal
Abstract
Introduction:
Chronic venous disease is a prevalent condition that worsens with age and is associated with poor quality of life.
The treatment of varicose veins (VV) has multiple alternatives, and different practices across Europe.
The aim of this article is to analyze the treatment of very elderly patients with severe forms of chronic venous disease using the VenaSeal technique.
Method, Material and Results:
Report of 5 very old patients with severe venous insufficiency treated with VenaSeal in 2021.
Clinical case 1:
A 86-year-old woman, with untreated bilateral varicose veins and recurrent ulcers, was observed in consultation, complaining of severe pain in left leg with an doppler ultrasound (DUS) showing bilateral great saphenous vein (GSV) insufficiency.
An outpatient basis treatment of the left great saphenous vein with VenaSeal associated with phlebectomies was performed in the left side.
After 6 months of follow-up, she is asymptomatic with small areas of repermeabilization of the proximal trunk of GSV.
Clinical case 2:
A 85-year-old man was observed in consultation describing two episodes of varicorrhagia in his right leg and and DUS with bilateral great saphenous vein insufficiency.
An outpatient basis treatment of the right great saphenous vein with VenaSeal associated with varicose veins foam esclerotherapy DUS guided was performed.
After a 3-month follow-up, the patient is asymptomatic with the imaging control showing occlusion of the trunk of the great saphenous vein.
Clinical case 3:
A 97-year-old woman was observed in consultation complaining of severe pain in left leg associated with an ulcer with severe interference with her quality of life and a DUS with bilateral great saphenous vein insufficiency.
An outpatient basis treatment of the left great saphenous vein with VenaSeal associated with varicose veins foam esclerotherapy DUS guided was performed.
After a 2-month follow-up, the patient is asymptomatic with a healed ulcer, with the DUS control showing occlusion of the great saphenous trunk.
Clinical case 4:
A 95-year-old woman was observed in consultation describing bilateral severe pain and ulcers in both legs and DUS with bilateral great saphenous vein insufficiency.
An outpatient basis treatment of bilateral great saphenous vein with VenaSeal associated with varicose veins foam esclerotherapy DUS guided was performed.
After 1-month follow-up, she is asymptomatic with healed ulcers and has occlusion of the right GSV´s trunk and areas of repermeabilization of left GSV´s trunk.
Clinical case 5:
An 84-year-old woman was observed in consultation with severe pain and severe pruritus of the left leg and a DUS with left GSV insufficiency.
An outpatient basis treatment of the left GSV with VenaSeal associated with phlebectomies was performed.
After 1 month of follow-up, the patient is asymptomatic with occlusion of the proximal left GSV´s trunk.
Discussion /Conclusion:
Treatment with Venaseal is not considered in the 2015 Guidelines of the ESVS, however the VeClose Study compared VenaSeal with radiofrequency ablation and reported equivalent improvement in symptoms scores and GSV occlusion.
VenaSeal treatment doesn´t require use of elastic compression after surgery and allows return to routine activity immediately, so it may be a good therapeutic option in this age group of patients with high clinical risk.
In our experience, VenaSeal resulted in complete resolution of the symptoms and ulcers in the short term. However, a complete occlusion of GSV was not observed in all cases, so new studies and protocols doses can be necessary.
Keywords: venaseal; eldery; Venous cronic disease; Varicose veins
Resumo
Introdução:
A doença venosa crónica é uma condição prevalente que piora com a idade e está associada a reduzida qualidade de vida.
O tratamento das varizes dos membros inferiores tem várias alternativas e diferentes práticas em toda a Europa.
O objetivo deste artigo é analisar o tratamento de pacientes muito idosos com formas graves de doença venosa crónica pela técnica de VenaSeal.
Método, Material e Resultados:
Descrição de 5 doentes muito idosos com insuficiência venosa grave tratados com VenaSeal em 2021.
Caso clínico 1:
Uma mulher de 86 anos com varizes bilaterais não tratadas e úlceras recorrentes de longa evolução, foi observada em consulta, referindo dores incapacitantes na perna esquerda observando-se no ecodoppler insuficiência da veia grande safena bilateralmente.
Foi realizado tratamento ambulatório da veia grande safena esquerda com VenaSeal associado a flebectomias do membro inferior esquerdo.
Com 6 meses de seguimento, encontra-se assintomática, observando-se no ecodoppler de controlo realizado pequenas áreas de repermeabilização do tronco proximal da veia grande safena.
Caso clínico 2:
Homem de 85 anos foi observado em consulta referindo dois episódios de varicorragia exuberantes na perna direita, observando-se no ecodoppler insuficiência da veia grande safena bilateralmente.
Foi realizado tratamento ambulatório de veia grande safena com VenaSeal associado a ecoesclerose de varizes.
Com 3 meses de seguimento encontra-se assintomático, observando-se no ecodoppler de controlo imagem de oclusão do tronco da veia grande safena.
Caso clínico 3:
Mulher de 97 anos observada em consulta referindo dor intensa na perna esquerda associada a úlcera com forte interferência com a sua qualidade de vida, observando-se no ecodoppler insuficiência da veia grande safena bilateralmente
Foi realizado tratamento ambulatório da veia grande safena esquerda com VenaSeal associado a ecoesclerose de varizes.
Com 2 meses de seguimento encontra-se assintomática com úlcera cicatrizada, observando-se no ecodoppler de controlo oclusão do tronco da veia grande safena.
Caso clínico 4:
Mulher de 95 anos observada em consulta referindo dor intensa associada a úlceras em ambas as pernas, observando-se no ecodoppler insuficiência da veia grande safena bilateralmente.
Foi realizado tratamento ambulatório de veia grande safena bilateralmente com VenaSeal associado a ecoesclerose de varizes.
Com 1 mês de seguimento encontra-se assintomática e com úlceras cicatrizadas, observando-se no ecodoppler de controlo oclusão do tronco da veia grande safena direita e áreas de repermeabilização do tronco da veia grande safena esquerda.
Caso clínico 5:
Mulher de 84 anos de idade observada em consulta referindo dor e prurido intenso na perna esquerda, observando-se no ecodoppler insuficiência da veia grande safena esquerda.
Foi realizado tratamento ambulatório da veia grande safena esquerda com VenaSeal associado a flebectomias.
Com 1 mês de seguimento, encontra-se assintomática observando-se no ecodoppler de controlo oclusão do tronco da veia grande safena esquerda.
Discussão / Conclusão:
O tratamento com Venoseal não é considerado nos guidelines da ESVS de 2015, no entanto, o Estudo VeClose comparou o tratamento com VenaSeal com o tratamento por radiofrequência e mostrou resultados equivalente nos scores sintomáticos e na taxa se oclusão das veias safenas .
O tratamento com VenaSeal não requer o uso de compressão elástica e permite o retorno imediato às atividades de rotina, podendo ser uma boa opção terapêutica em pacientes desta faixa etária que possuem um alto risco clínico.
Na nossa experiência, o VenaSeal resultou na resolução completa dos sintomas e úlcera no curto prazo. Porém, ao não ser observada uma oclusão completa da veia grande safena em todos os casos, são necessários novos estudos e novos protocolos de dosagem são necessários.
Palavras-chave: Venaseal; Idosos; Insuficiência venosa crónica; Varizes
Introduction
The surgical treatment of varicose veins of the lower limbs has multiple alternatives, each with advantages and disadvantages.
Modern conventional surgery has well-defined results but is more aggressive and has a longer recovery time. Thermal endovenous surgery has the advantages of being less aggressive than conventional surgery but involves tumescent anesthesia. Chemical intravenous surgery with cyanoacrylate has the advantage of being performed under local anesthesia and the return to normal activity is almost immediate. Chemical surgery with sclerosing agents can be performed under local anesthesia but is associated with higher recurrence rates.
However, no technique is validated for very elderly patients in whom the risk associated is increased due to a greater association with comorbidities.
The aim of this paper is to analyze the treatment of very elderly patients with severe forms of chronic venous disease using the VenaSeal technique.
Method, material and results
Descriptive analysis of 5 patients with more than 85 years diagnosed with severe superficial venous insufficiency with failed medical therapy, that were treated with VenaSeal in 2021.
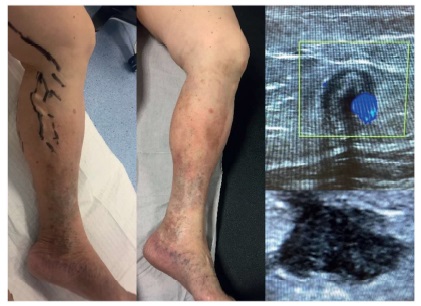
Clinical case 1 (image 1)
An 86-year-old woman, with untreated long-term bilateral varicose veins with recurrent ulcers in her left leg, comes to the consultation describing severe pain in her left leg with high interference in her quality of life.
On physical examination was observed a healed ulcer, white atrophy and stasis dermatitis and was very painful to touch.
The Doppler ultrasonography showed insufficiency of both great saphenous veins with a diameter greater than 8mm.
It was proposed, in an outpatient basis, treatment with venaseal catheter associated with phlebectomies, which was uneventful.
After 6 months of follow-up, the patient is asymptomatic with the imaging control showing small areas of proximal repermeabilization of the trunk of the great saphenous vein.
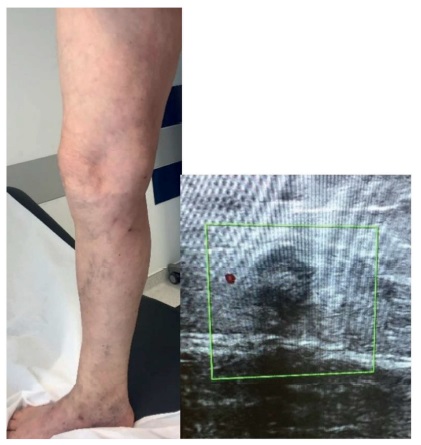
Clinical case 2 (image 2)
An 85-year-old man with untreated long-term bilateral varicose veins is referred for having had 2 episodes of violent nocturnal varicorrhagia in his right leg.
On physical examination, two areas of varicose erosion are observed without active bleeding.
The Doppler ultrasonography showed insufficiency of both great saphenous veins with a diameter greater than 8mm.
It was proposed to perform in an outpatient basis treatment with venaseal of the right great saphenous vein associated with varicose veins foam esclerotherapy DUS guided which was uneventful.
After a 3-month follow-up, the patient is asymptomatic with the imaging control showing occlusion of the trunk of the great saphenous vein.
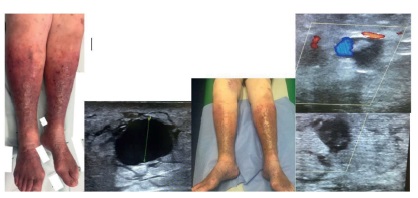
Clinical case 3 (image 3)
A 97-year-old woman with untreated long-term bilateral varicose veins is referred for pain in her left leg with severe interference in her quality of life.
She started medical treatment with NSAIDs, venotropic and topical corticosteroids associated with the use of elastic stockings with initial symptomatic improvement.
Symptoms then recurred associated with the appearance of an ulcer on the leg at 30 days.
The Doppler ultrasonography showed bilateral insufficiency of the great saphenous vein with a diameter greater than 8 mm.
It was proposed to perform, in an outpatient basis treatment, with venaseal of the left great saphenous vein associated with varicose veins foam esclerotherapy DUS guided which was uneventful.
In the second day an erythematous rash appeared on the face prompting systemic corticosteroid therapy.
After a 2-month follow-up, the patient is asymptomatic with a healed ulcer, with the imaging control showing occlusion of the great saphenous trunk.
Clinical case 4 (image 4)
A 95-year-old woman with untreated long-term bilateral varicose veins with recurrent ulcers since the year 2000 is referred for consultation with pain and leg ulcers in both legs, with severe interference in her quality of life.
She started medical treatment with NSAIDs, antibiotics, venotropic and topical corticosteroids associated with the use of elastic stockings without improvements.
The Doppler ultrasonography showed bilateral insufficiency of the great saphenous vein with a diameter greater than 10 mm in the right sized and a diameter greater than 20mm in the left side.
It was proposed to perform in an outpatient basis treatment with venoseal of both interna saphenous vein associated with varicose veins echosclerosis which was uneventful.
With a 2-month follow-up, the patient is asymptomatic with a healed ulcer, with the imaging control showing occlusion of the right great saphenous trunk and areas of proximal areas of repermeabilization of the trunk of the left great saphenous vein.
Clinical case 5: (image 5)
An 84-year-old woman with untreated long-term bilateral varicose veins, comes to the consultation complaining of a severe pain and pruritus in her left leg with severe interference in her quality of life.
On physical examination was observed stasis dermatitis and severe eczema that was very painful to touch.
The Doppler ultrasonography showed insufficiency of the right great saphenous veins with a diameter greater than 8mm.
It was proposed, in an outpatient basis, treatment with venaseal catheter associated with phlebectomies, which was uneventful.
After 1 month of follow-up, the patient is asymptomatic with the imaging control showing occlusion of the trunk of the great saphenous vein.
Discussion
Chronic venous disease (CVD) is a prevalent condition that tends to worsen with age. As the disease increases in severity (to include varicose veins, skin changes, and venous ulcer) and the quality of life (QoL) diminishes, the demand for treatment increases. The prevalence of CVD is highest in Western1.
The QoL of patients with venous ulceration (C6) has been reported to be comparable to that of patients with congestive heart failure or chronic lung disease, suggesting that, if CVD is allowed to progress to severe stages, the QoL of CVD patients can become very poor2.
A systematic review showed that the burden of varicose veins and treatment practices varies across Europe3.
Compression therapy remains the mainstay of therapy, though adherence can be poor, especially in the elderly, due to the sensation of warmth and deterioration of pre-existing pruritis associated with venous eczema4. According to Morikage et al the best adherence to compression terapy in eldery patients is achieved by using a moderate stocking, while the best efficacy is achieved by using bandages5. However, when the symptoms significantly interfere with the patient's quality of life, an aggressive approach has to be considered besides medical therapy. Surgical treatment of varicose veins of the lower limbs in very old patients (> 85 years) is usually avoided. The development of venous endovascular surgery, may be particularly useful for this group of patients due to is less invasiveness.
According to 2015 Guidelines of the European Society for Vascular Surgery for Management of Chronic Venous Disease, endovenous thermal ablation is referred as the first choice for treatment of saphenous vein insufficiency. Open surgery is considered to be effective but with slower post-operative recovery. Foam sclerotherapy can be considered in old and fragile patients despite a higher recurrence rate. Treatment with cyanoacrylate glue is not considered4.
In the VeClose Study, the VenaSeal (Cyanoacrylate) was compared with RFA and complete GSV occlusion at one year was 97.2% for cyanoacrylate and 97% for RFA. There were also equivalent improvements in symptoms scores6.
According to Proebstle et al, GSV occlusion at 12-month after Venaseal treatment was 92.9% and the mean Venous Clinical Severity Score improved from 4.3 ± 2.3 at baseline to 1.1 ± 1.3 at 12 months and Aberdeen Varicose Vein Questionnaire score showed an improvement from 16.3 at baseline to 6.7 at 12 months (P < .0001)7.
The treatment with VenaSeal can be performed under local anesthesia, allows the integral treatment of the saphenous vein and doesn't require the use of elastic compression. It also allows return to routine activity immediately, which is of particular interest.
The venoseal technique can be associated with phlebectomies or ecoesclerosis like we have done in our cases8.
A common complication of cyanoacrylate vein closure is phlebitis, with reports to occur from 11.4%9 to 23.5%10 and typically resolves within 2 weeks. One other adverse reactions associated with this treatment has been hypersensitivity that occurred in 6.3% of the patients, (mild in 4.2%, moderate in 1.3%, and severe in 0.3%) with no patient predictive factors and a trend to a decreased hypersensitivity in patients CEAP C4-C6, as we observed in clinical case 311.
Finally, an increased GSV diameter has been associated with a decreased glue extension length and, consequently, a longer remnant stump12. In our experience, an issue that needs to be study in future studies is the relationship between the diameter of the GSV and the amount of cyanoacrylate to be applied to achieve total occlusion of GSV.
Conclusion
In our recent experience in very elderly patients the use of the venaseal cateter resulted in a complete resolution of the symptoms and the cure of the ulcer in the short term. However, a complete occlusion of the great saphenous vein was not observed in all patients and so new studies and protocols doses can be necessary particularly in veins with large diameters.
References
1. The Seriousness of Chronic Venous Disease: A Review of Real-World Evidence. Adv Ther (2019) 36: S5-S12.
[ Links ]
2. Carradice D, Mazari FA, Samuel N, Allgar V, Hatfield J, Chetter IC. Modelling the effect of venous disease on quality of life. Br J Surg. 2011;98(8):1089-98.
[ Links ]
3. Moore HM, Lane TR, Thapar A, Franklin IJ, Davies AH. The European burden of primary varicose veins. Phlebology. 2013;28(Suppl 1):141-7.
[ Links ]
4. Wittens et al. Management of Chronic Venous Disease Clinical Practice Guidelines of the European Society for Vascular Surgery (ESVS) Eur J Vasc Endovasc Surg (2015) 49, 678-737.
[ Links ]
5. K, Morikage N, Yamashita O, et al. Adherence to and efficacy of different compression methods for treating chronic venous insufficiency in the elderly. Phlebology. 2016;31(10):723-728.
[ Links ]
6. Morrison, N.; Gibson, K.; Vasquez, M.; Weiss, R.; Cher, D.; Madsen, M.; Jones, A. VeClose trial 12-month outcomes of cyanoacrylate closure versus radiofrequency ablation for incompetent great saphenous veins. J. Vasc. Surg. Venous Lymphat. Disord. 2017, 5, 321-330.
[ Links ]
7. Proebstle T., Alm J, et al. The European multicenter cohort study on cyanoacrylate embolization of refluxing great saphenous veins. J Vasc Surg Venous Lymphat Disord. 2015;3(1):2-7.
[ Links ]
8. Kathleen Gibson, Renee Minjarez, Krissa Gunderson, Brian Ferris. Need for adjunctive procedures following cyanoacrylate closure of incompetent great, small and accessory saphenous veins without the use of postprocedure compression: Three-month data from a postmarket evaluation of the VenaSeal System (the WAVES Study). Article information. 2019; 34(4):231-237.
[ Links ]
9 Proebstle TM, Alm J.,Dimitri S, Rasmussen L., Whiteley M, Lawson J, Cher D, Davies, A. The European multicenter cohort study on cyanoacrylate embolization of refluxing great saphenous veins. J. Vasc. Surg. Venous Lymphat Disord201532-7
[ Links ]
10. Park, I et al. Initial Outcomes of Cyanoacrylate Closure, VenaSeal System, for the Treatment of the Incompetent Great and Small Saphenous Veins. Vasc. Endovasc. Surg. 2017, 51, 545-54
[ Links ]
11. Kathleen Gibson, Renee Minjarez, Elena Rinehardt, Brian Ferris. Frequency and severity of hypersensitivity reactions in patients after VenaSeal(tm) cyanoacrylate treatment of superficial venous insufficiency. Article information. 2019; 35(5):337-344.
[ Links ]
12. Insoo Park, MD1, Daehwan Kim, MD1. Correlation Between the Immediate Remnant Stump Length and Vein Diameter After Cyanoacrylate Closure Using the VenaSeal System During Treatment of an Incompetent Great Saphenous Vein. Article information. 2020; 54(1): 47-50.
[ Links ]