Introduction
The escalation in prevalence of diabetes mellitus, which is currently a global epidemic, has resulted in an increasing volume of cases of chronic limb-threatening ischemia (CLTI) in the context of distal and ultra-distal arterial disease.1 This pattern remains a huge challenge for vascular surgeons.
Endovascular treatment of tibial arteries, once reserved for focal lesions or high-risk patients, is currently the first option in most centers. However, scientific evidence regarding endovascular revascularization is very limited in distal disease patterns.2
The aim of this study was to analyze the results of open ultra-distal revascularization in patients with CLTI, in a single-centre specially dedicated to these techniques.
Methods
Inclusion criteria and data collection
All patients with CLTI undergoing infra-malleolar bypass between April 2012 and December 2019 were included in this single-center retrospective analysis. The inclusion criteria were all bypasses performed to the retromalleolar posterior tibial artery, common plantar artery, internal plantar artery, external plantar artery, dorsalis pedis and infra-malleolar collaterals.
Clinical end points and variable definitions
The primary end points were freedom from CLTI and freedom from new CLTI. The remaining end points were limb-based patency (LBP), primary (PP) and secondary (SP) patency rates, limb salvage, amputation-free survival (AFS) and mortality. We defined freedom from CLTI as the absence of rest pain and/or the complete healing of lesions, and freedom from new CLTI as the recurrence of trophic lesions or ischemic rest pain after achieving freedom from CLTI. According to the 2019 Global Vascular Guidelines, LBP was considered lost when anatomical failure (occlusion, critical stenosis or any reintervention in the target arterial pathway) or hemodynamic failure (CLTI symptoms in the ipsilateral limb with stenosis > 50% in the target arterial pathway) were observed. AFS was defined as patients alive without above ankle amputation.
Patients were categorized into subgroups based on age (above or under 75 years), presence of chronic kidney disease (CKD) on hemodialysis and wound and infection grade of the WIfI classification (0 and 1 versus 2 and 3).3
Revascularization patency was assessed by duplex ultrasound (DUS). We defined limb salvage as the maintenance of a part of the foot that allows ambulation without prosthesis, including toe and trans-metatarsal amputations.
The follow-up was performed by DUS at 1, 3, 6, 9 and 12 months and every 6 months thereafter, to allow the early detection of failing grafts. Patients with non-healed trophic lesions were observed more often.
Diagnosis and technical details
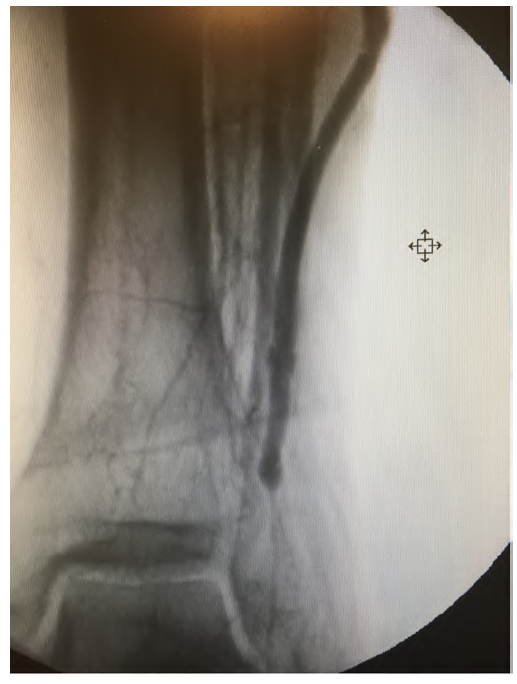
In this series, all patients underwent arterial and venous DUS of the lower limbs in the initial evaluation and, again, before the revascularization procedure. Conventional diagnostic angiography of the lower limbs was systematically performed, in order to plan the revascularization procedure, except in patients with advanced non-dialysis CKD. The contrast injection was performed by a retrograde common femoral artery puncture with a 4F introducer, in a single bolus of 80 cc at a flow rate of 6 mL/sec and 600 psi of pressure. This allows the recruitment of all collaterals responsible for irrigation of the leg and foot, many of them originating from the profunda femoral artery, thus obtaining a greater anatomical detail (Figure 1). In patients with contraindication to angiography, the procedures were planned according to arterial DUS findings.

Figure 1 Anatomical detail of an angiography where only a collateral of the peroneal artery is patent.
We chose to perform ultra-distal revascularization whenever the retromalleolar posterior tibial artery, common plantar artery, internal plantar artery, external plantar artery, dorsalis pedis or infra-malleolar collaterals were the only vessels allowing direct flow to the foot in the presence of CLTI.
Once the target artery was selected for revascularization, patients were once again evaluated by DUS to select the most appropriate conduit. In this series, all revascularizations were performed with autologous vein graft, preferably inverted single-segment great saphenous vein. In cases where this was not possible, we used the small saphenous vein, cephalic vein or vein splicing in this order.
Pre-operative marking of vein graft and the distal anastomotic site was performed (Figure 2). These practices reduce surgical time and incision related morbidity.

Figure 2 Pre-operative marking of a peroneal artery collateral. Red arrow pointing at the marking on the skin
All distal anastomoses were performed without the use of clamps, by means of an Esmarch bandage. Angiographic control was systematically performed at the end of the procedures (Figure 3).
All patients with poor run-off were anticoagulated with warfarin or, in cases of poor compliance or difficulty maintaining target INR, with direct oral anticoagulants.
Statistical analysis
Statistical analysis was conducted using Stata 12.1 (StataCorp®, Lakeway Drive, College Station, Texas, USA). Continuous variables were presented as median with interquartile amplitude range, between quartiles 25 and 75, according to the format [median (interquartile range)]. Categorical variables were presented as absolute numbers with corresponding percentage values [absolute number (percentage)]. Time-to-event end points were presented in Kaplan-Meier estimates, censored for major amputation, mortality or last follow up and compared using logrank test. All analyses were considered statistically significant if a two-tailed p value < 0.05 was observed.
Results
Between April 2012 and December 2019, 134 ultradistal revascularization procedures were performed, 75 of which to the dorsalis pedis artery, 40 to the retro-malleolar posterior tibial artery, 13 to plantar arteries, 3 to infra-malleolar collaterals and 3 simultaneous revascularizations of 2 arteries (plantar and dorsalis pedis n=2; peroneal and dorsalis pedis, n=1). These revascularizations were performed in 122 patients (111 men and 11 women) with a median age of 68 years (IQR 12). The demographics and basic characteristics of the studied population are presented in Table 1.
Table 1 Demographics and baseline characteristics of the studied population
| Characteristics | Ultra-distal bypass (n=134) |
|---|---|
| Male gender | 111 (83%) |
| Age, years (IQR) | 68 (12) |
| BMI, kg/m2 (IQR) | 26 (6) |
| Smoking status | |
| Active smoker | 22 (16%) |
| Former smoker | 33 (25%) |
| Comorbidities | |
| Hypertension | 123 (92%) |
| Diabetes mellitus | 107 (80%) |
| Coronary disease | 43 (32%) |
| CKD (eGFR<60 mL/min/1.73m2) | 52 (39%) |
| CKD on dialysis | 20 (15%) |
| WIfI | |
| Wound class | |
| 0 | 11 (8%) |
| 1 | 44 (33%) |
| 2 | 69 (51%) |
| 3 | 10 (7%) |
| Foot Infection class | |
| 0 | 66 (49%) |
| 1 | 27 (20%) |
| 2 | 40 (30%) |
| 3 | 1(1%) |
| Pre-operative medication | |
| Statins | 73 (54%) |
| Antiplatelets | 78 (58 %) |
This number of procedures accounts for 20% of the total number of revascularizations performed in this institution during the same time period.
Inflow was obtained from the infragenicular popliteal artery in 58% of the cases (n=78), the femoral artery in 34% (n=46) and tibial arteries in 8% (n=10). Alternative grafts were used in 12% of the cases, specifically, the cephalic vein (n=1), the small saphenous vein (n=9) and splicing of great saphenous vein (n=6). The inflow and conduits used are shown in Table 2.
Table 2 Conduits and inflow arteries
| Number of procedures | |
| Conduit | 111 (83%) |
| Great saphenous vein | 118 |
| Small saphenous vein | 9 |
| Cephalic vein | 1 |
| Splicing of great saphenous vein | 6 |
| Inflow artery | |
| Below-knee popliteal | 78 |
| Common femoral | 24 |
| Superficial femoral | 14 |
| Profunda femoral | 8 |
| Anterior tibial | 2 |
| Posterior tibial | |
| Peroneal | 6 |
| Tibioperoneal trunk | 1 |
The median follow-up was 33.7 months (IQR 38.6). Mortality at 30 days was 1.6% (2 patients) and perioperative complications occurred in 10% of patients, as indicated in Table 3.
Table 3 Perioperative complications
| Complications | n (%) |
|---|---|
| Myocardial infarction | 3 (2%) |
| Stroke | 3 (2%) |
| Surgical wound infection | 5 (4%) |
| Surgical wound dehiscence | 3 (2%) |
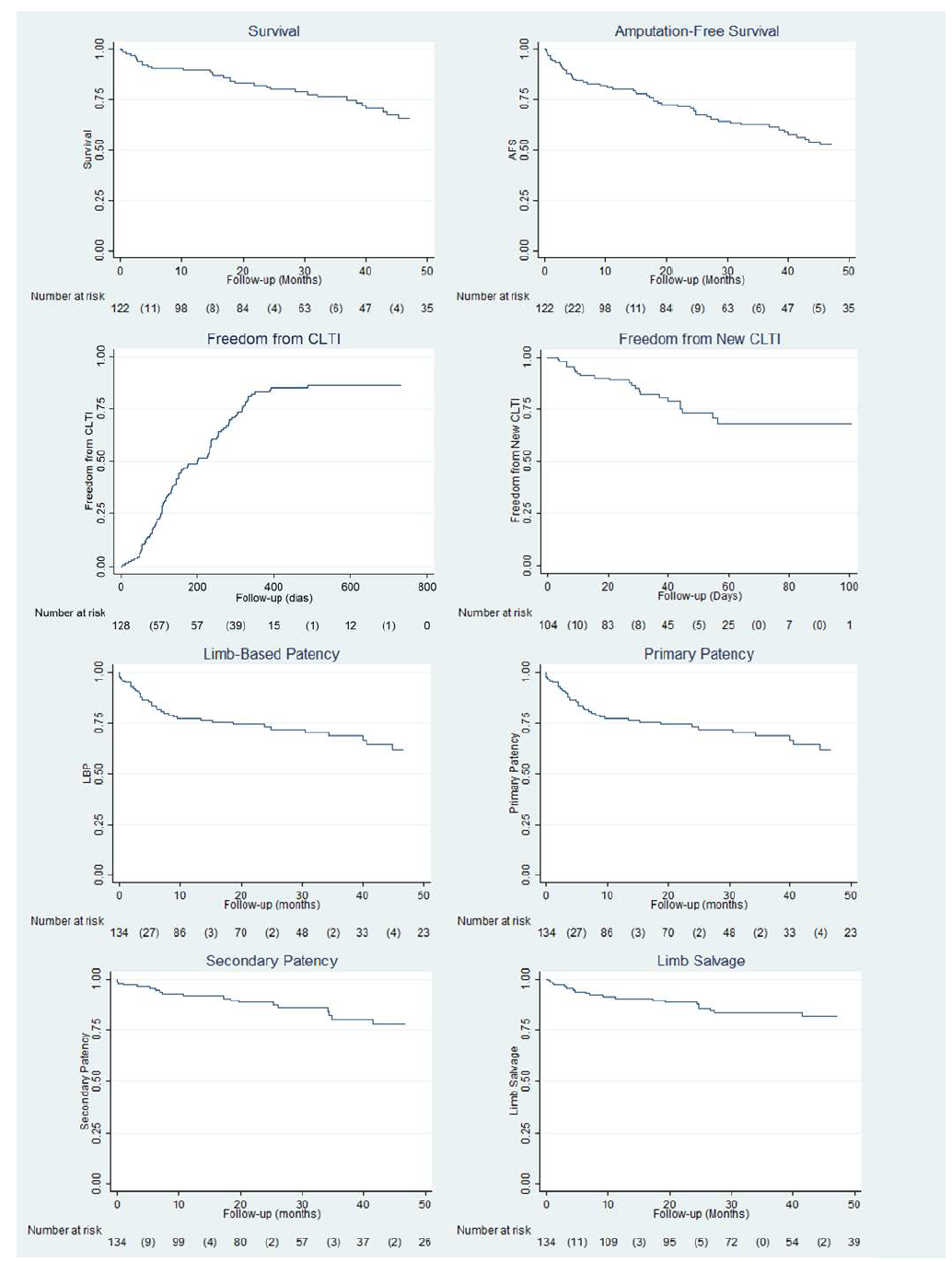
LBP, PP and SP were, respectively, 78%, 78% and 92% at 1 year, 73%, 73% and 88% at 2 years, and 62%, 62% and 79% at 4 years. At 1 year, 83% of the limbs were free from CLTI, and at 2 and 4 years of follow up, 89% and 74% of these patients remained free from new CLTI, respectively. Eighty-two percent of the patients were free of major amputation at 4 years. Survival at 1 year and 2 years was 90% and 81%, respectively. These variables are presented in Kaplan-Meier estimates (Figure 4). Revascularization, limb and survival-related end points are presented in table 4. There were 6 early graft occlusions (< 30 days), corresponding to 4.5% of patients.
Table 4 Revascularization, limb and survival related end points
| End points | Ultradistal bypass (n=134) |
|---|---|
| Revascularization-related end points | 111 (83%) |
| Limb-based patency (LBP) | |
| 1 year | 78% |
| 2 years | 73% |
| 4 years | 62% |
| Primary patency | |
| 1 year | 78% |
| 2 years | 73% |
| 4 years | 62% |
| Secondary patency | |
| 1 year | 92% |
| 2 years | 88% |
| 4 years | 79% |
| Limb-related end points | |
| Freedom from CLTI | |
| 6 months | 49% |
| 12 months | 83% |
| Freedom from new CLTI | |
| (n=104) † | |
| 1 year | 91% |
| 2 years | 89% |
| 4 years | 74% |
| Limb salvage | |
| 1 year | 90% |
| 2 years | 89% |
| 4 years | 82% |
| Survival-related end points (n=122) | |
| Survival | |
| 1 year | 90% |
| 2 years | 81% |
| 4 years | 65% |
| Amputation-free survival | |
| 1 year | 80% |
| 2 years | 70% |
| 4 years | 53% |
† Freedom from new CLTI focuses on a total of 104 revascularized limbs, which corresponds to the number of cases that previously achieved freedom from CLTI.
Subgroup analysis
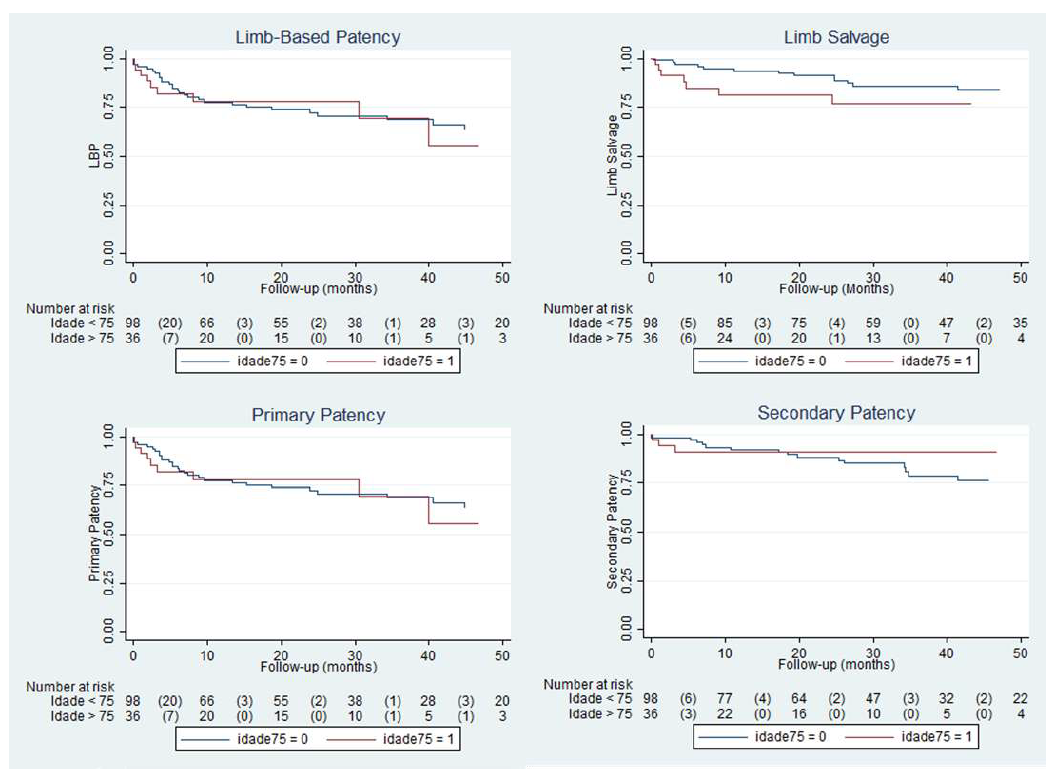
The subgroup analysis for age (>75 versus < 75 years) did not reveal statistically significant differences regarding LBP, PP and SP (Figure 5).
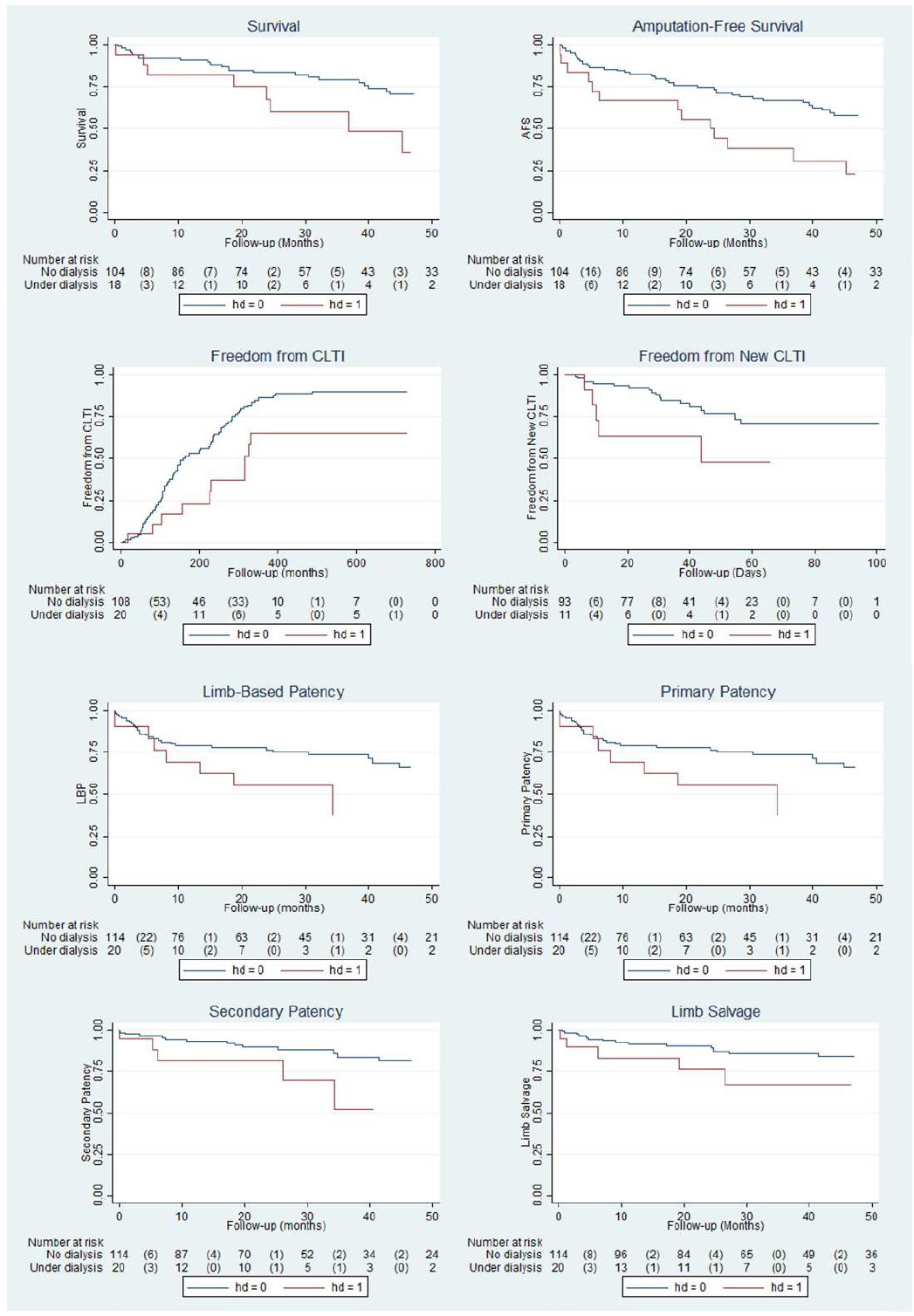
The presence of CKD on dialysis was statistically significant for the survival end point (p = 0.012), amputation-free survival (p = 0.003), freedom from CLTI (p = 0.012) and freedom from new CLTI (p = 0.031). However, in the patency and limb-related end points, there were no statistical differences (Figure 6).
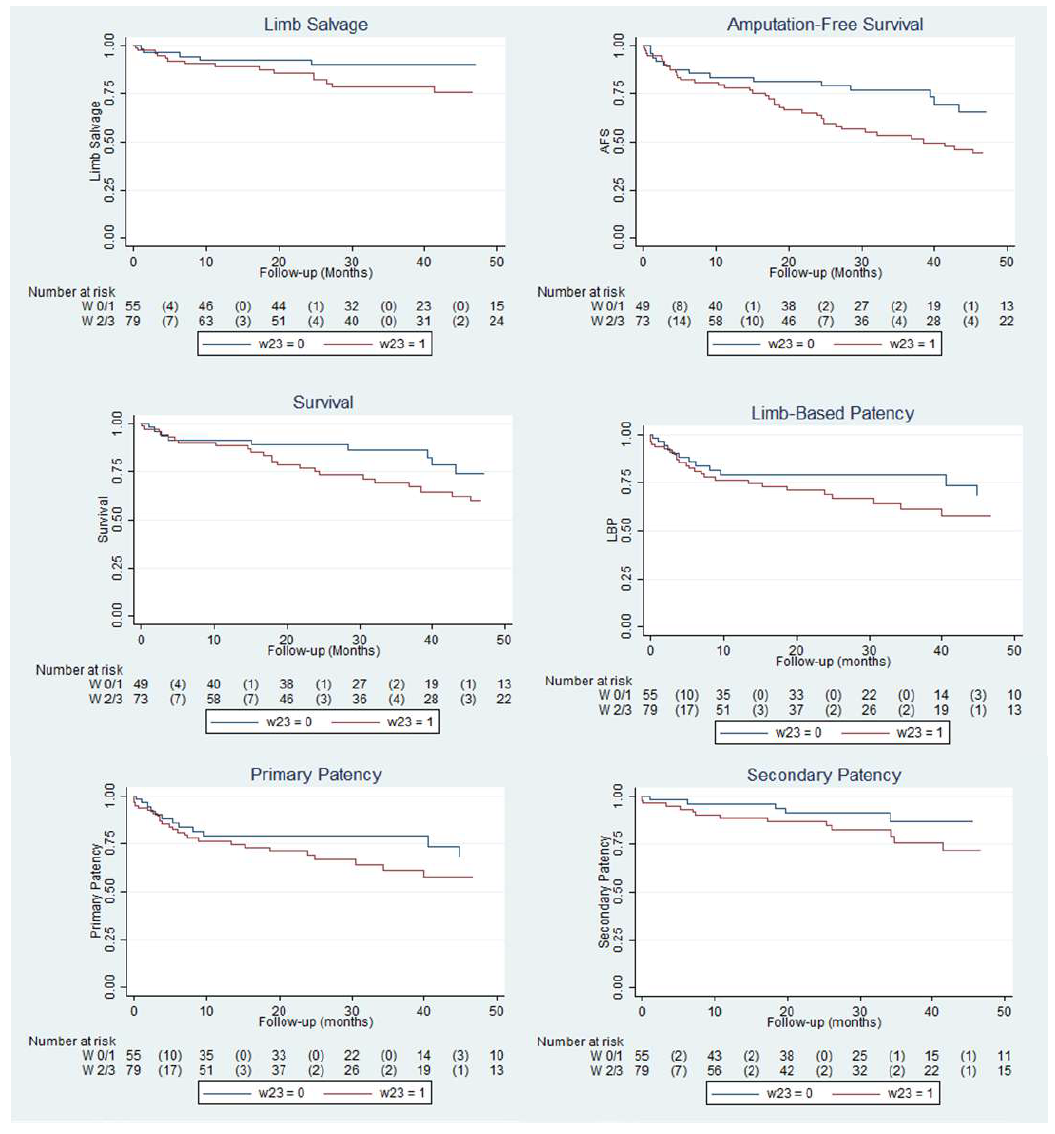
Regarding the foot infection class, we found that patients with more severe infection (grade 2 or 3 in the WIfI classification) had a lower survival (p = 0.042). There were no statistically significant differences for the remaining end points (Figure 7).
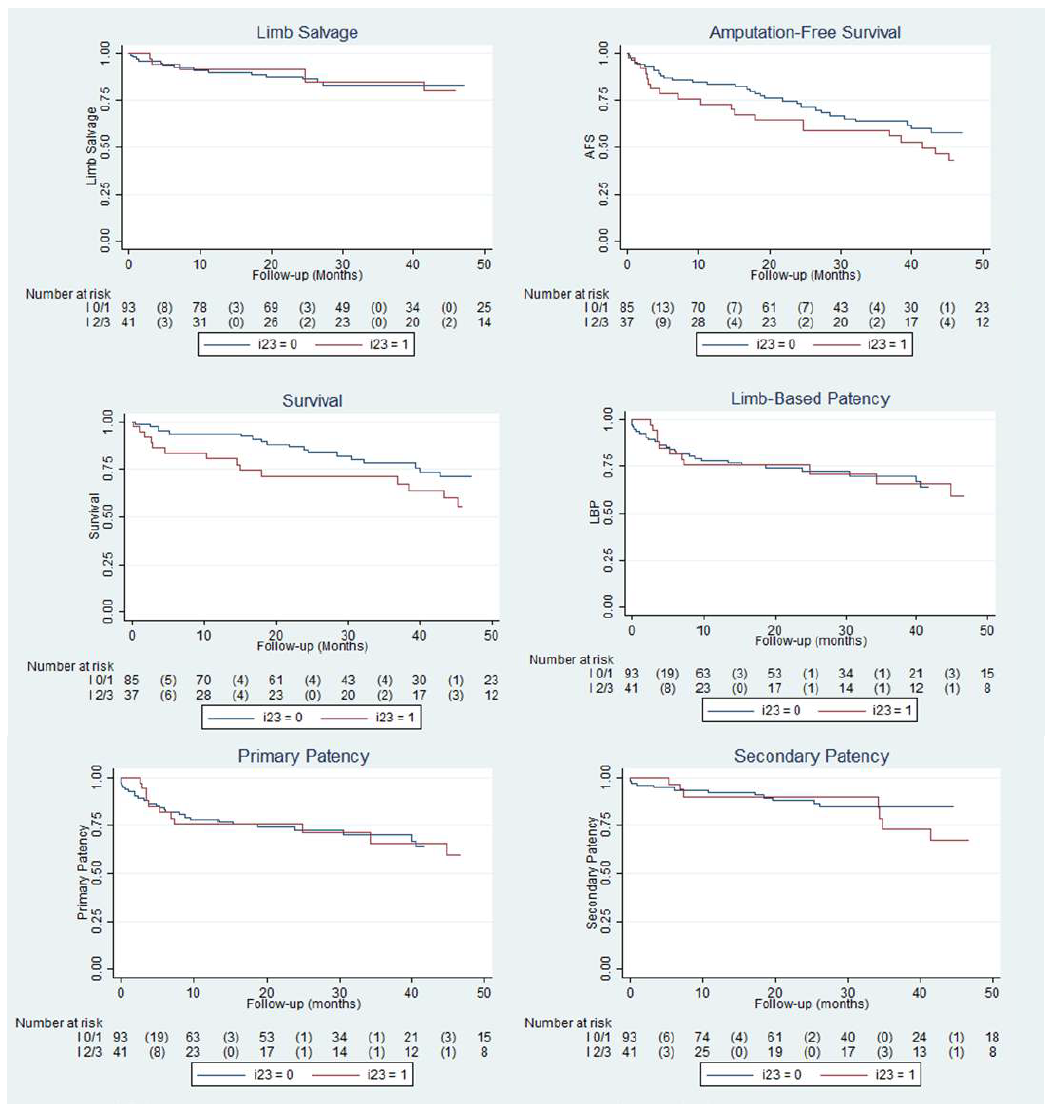
Figure 7 Subgroup analysis for infection status grade 0 and 1 versus 2 and 3 of the WIfI classification.
Finally, wound severity (grade 2 or 3 in the WIfI classification) was related to a lower survival (p = 0.0360) and a lower AFS (p = 0.030), without influence on the remaining variables (Figure 8).
Discussion
This study demonstrates that open ultra-distal revascularization in patients with CLTI is safe, effective and durable. LBP, PP, SP, limb preservation and AFS rates were very good, even at 4 years of follow up. We consider that a limb salvage rate of 82% at 4 years in patients submitted to infra-malleolar bypass is exceptional considering this challenging territory. This series had a long follow up (median 33.7 months), allowing assessment of limb and survival-related end points for a longer period than most published studies. Patency rates were high, reaching a secondary patency of 79% at 4 years. These results are comparable to Pomposelli et al, one of the largest series of ultra-distal bypasses (primary patency, secondary patency, and limb-salvage rates of 56.8%, 62.7%, and 78.2% at 5 years).4 Thirty-day mortality was 1.6% and the complication rate was 10%, acceptable for this population. One-year survival was 90% and 2-year survival was 81%, emphasizing that this group of patients, despite the high risk of major adverse cardiovascular events (MACE), benefit of durable revascularization procedures. We highlight that 15% of the patients in this series had CKD on dialysis, an unequivocal marker of clinical severity and complexity of arterial disease. Another aspect that deserves to be stressed, is the fact that 49% of our patients achieved CLTI remission at 6 months and 83% after at one year. These data are explained by the complexity of the wounds, highlighting the efficacy of revascularization and the absolute need for durability in the treatment of distal CLTI. Spillerova et al demonstrated that bypass surgery is associated with better healing rates when compared to endovascular surgery (p = 0.014; HR, 1,536; 95% CI, 1,091-2,162), supporting our results.5 However, in this same study, the limb preservation rate was similar for both strategies (HR, 0.791; 95% CI, 0.437-1,434). This type of results is often interpreted as favorable to endovascular treatment, but these considerations should be the subject of deeper reflection. We hypothesize that the main reason why major adverse limb event (MALE) rates tend to be similar for open and endovascular surgery in distal disease is the fact that this end point is composed by amputation, major reintervention, and untreated patency loss. When the end point amputation is analyzed separately, the advantages of open surgery usually become more evident. The relevance of the revascularization procedure is only achieved when complete healing of wounds is obtained. A meta-analysis on distal angioplasty in patients with CLTI by Romiti et al, rightly highlights the large gap between patency rates and limb salvage.6 In his paper, it is advocated that this gap may be due to unhealed wounds, secondary patency achieved through bypass surgery or even the fact that not all patients had CLTI.6
The recently published BEST-CLI trial reaffirmed the superiority of venous bypass in infra-inguinal CLTI.7 We look forward to the results of the BASIL-2 trial.8
Our results support this strategy even in older patients (> 75 years), with no significant differences regarding limb-related end points and morbidity (Figure 4).
Survival, AFS, freedom from CLTI and freedom from new CLTI were significantly worse in patients on hemodialysis. These findings are expected given their higher incidence of MACE and the severity of arterial disease, that characterizes these patients. However, surprisingly, the limb and revascularization-related results, specifically, limb preservation, LBP, PP and SP, were not statistically different between groups. These results are evidence of the good performance of open surgery even in the most unfavorable patients (Figure 5).
Increased infection severity (grade 2 or 3 of the WIfI classification) was a predictor of lower overall survival. However, revascularization and limb-related results showed no differences. In cases of severe infection, we consider that the restoration of high-quality flow to infected tissues warrants adequate local antibiotic concentrations, maintaining excellent limb preservation rates, even in the most complex cases.4
Wound class 2 and 3 of the WIfI classification was a predictor of lower amputation-free survival and survival rates, when comparing to less extensive wounds (grade 0 and 1), with no repercussion on the remaining analyzed variables, namely, on limb preservation. These results suggest that complex wounds are associated with higher mortality, inferring a greater clinical severity in this subgroup of patients.
The limitations of the present study reside in the fact that it is a retrospective, single-center study, in a department particularly dedicated to open ultra-distal bypass. Additionally, it is a non-comparative observational study regarding the endovascular approach, so the discussion is centered on results from the literature.
Conclusion
This series demonstrates the excellent results of infra-malleolar bypass in distal and ultra-distal CLTI. In high volume centers, this technique is safe, effective, and durable in the treatment of patients with CLTI. Limb salvage, primary and secondary patency rates, LBP and wound healing are very good, in one of the most demanding territories for open and endovascular revascularization. These results were not negatively influenced by age, wound severity or infection, nor by the presence of CKD on hemodialysis.
These results are reproducible, although dependent on planning, technical details and follow-up, specific to distal and ultra-distal disease.
We consider that these techniques should be mastered by all vascular surgeons involved in the treatment of CLTI, implying an educational effort from all institutions.