Introduction
The high mortality rate associated with ruptured abdominal aortic aneurysm demands treatment as soon as possible. This obvious concept is included in recent clinical practice guidelines.1 The acceptable time frame from door-to-intervention is defined and should not exceed 90 minutes: 30 minutes for the initial management in the first-line hospital, 30 minutes for transport and 30 minutes for preparation in the referral institution.2 However, perhaps even more important is the time elapsed before the admission in a tertiary hospital when patients are referred from distant hospitals, often located in different regions of the country.
Since there was no recent study addressing this issue in Portuguese populations, the authors sought to analyse the accomplishment of the recommended time goals in a national tertiary referral centre for this pathology.
The main aims of this study were: (1) the description of the median times between the diagnosis of ruptured or symptomatic abdominal aortic aneurysm and the start of treatment, both pre-hospital and intra-hospital; (2) evaluation of the differences between the geographical regions referring to our centre; and (3) assess the relationship between the diagnosis-to-intervention time interval and mortality rates at 24 hours, 48 hours, and 30 days post-surgery.
Methods
An observational study of a single-centre cohort of retrospectively collected data was performed. We included all patients with ruptured or symptomatic abdominal aortic aneurysm who underwent aneurysm repair, either open or endovascular, at Centro Hospitalar Universitário Lisboa Norte (CHULN) between January 2012 and December 2021.
The cohort included both ruptured and symptomatic aneurysms. Symptomatic patients were defined as patients with tender aneurysms or with abdominal pain with no other cause. The inclusion of symptomatic aneurysms in the study was due to the institutional policy of treating symptomatic patients with similar priority as overt rupture cases.
We analysed the data regarding age, gender and the exact time of the following events:
time of CT angiography that established the diagnosis- assumed as the moment of diagnosis.
time of admission in CHULN.
time of admission in the operating room (OR)- assumed as moment when treatment started.
The time interval between diagnosis and treatment, which will be referred hereon as Interval of Referral.
The time interval between arriving to CHULN (door) to the OR was defined as Interval Door-OR.
Statistical analysis was performed using SPSS software, version 26 (Statistical Package for the Social Sciences, Inc., Chicago, IL), for Mac. Continuous variables are presented as mean (standard deviation-SD) if normally distributed and median (interquartile range- IQR) if not. Categorical variables are presented as frequency (percentage). Mann-Whitney test was used when comparing continuous variables and Fisher’s exact test to compare categorical variables. All analyses were considered statistically significant if a two-tailed p-value <0.05 was observed.
Results
Demographic data and clinical presentation
One hundred and fifty patients were included (91% men; mean age 78.3 years, SD 8.7). Of these, 129 (86%) presented with ruptured aneurysms and the remaining 21 (14%) with symptomatic aneurysms.
One hundred and forty-three were treated by open surgery and only 7 by endovascular aneurysm repair (REVAR) as we started our regular REVAR program in 2021.
Interval of Referral
The overall median Interval of Referral was 3 hours-180 minutes (+/-126) in both symptomatic and ruptured aneurysms. In the group of ruptured aneurysms, the median interval of referral was 2.5h- 150 minutes (+/-132), Figure 1.
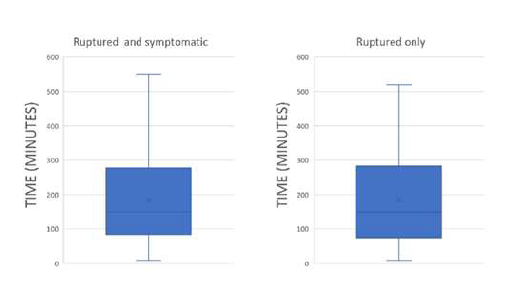
Figure 1 Median Interval of Referral on total cohort. Ruptured and symptomatic abdominal aortic aneurysms (left) and ruptured abdominal aortic aneurysms only (right)
Considering the group of patients with ruptured aneurysms, 32 were treated under 90 minutes, 64 between 90 minutes and 360 minutes and 15 more than 360 minutes after diagnosis. In 20 patients it was not possible to assess the CT-OR time because of missing data. This means that only 22% of the patients with ruptured aneurysm (not symptomatic) were treated under the recommended 90-minute interval. When analysing only the group of patients referred from centres outside our hospital, this percentage dropped to 7%, Figures 2 and 3.
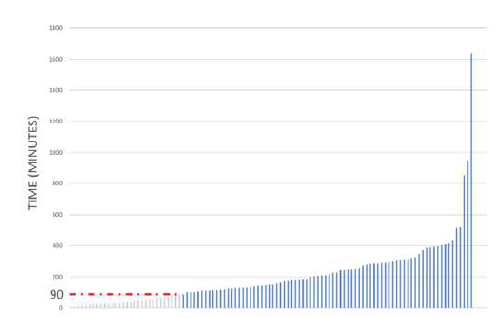
Figure 2 Subgroup of ruptured abdominal aortic aneurysm cases, ordered by Interval of Referral - from shortest to longest. Red line represents the 90-minute recommended threshold for time between diagnosis and repair.
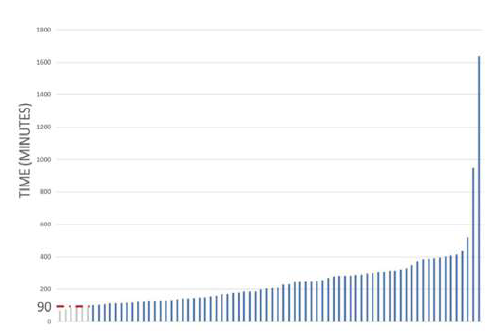
Figure 3 Subgroup of ruptured abdominal aortic aneurysm cases referred from outside hospitals - ordered by Interval of Referral, from shortest to longest. Red line represents the 90-minute recommended threshold for time between diagnosis and repair.
When analysing the evolution of the Interval of Referral through the period of the study, no significative changes or improvements were demonstrated, Figure 4.
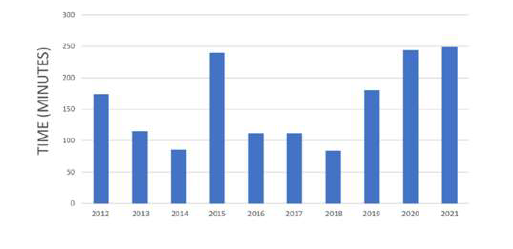
Figure 4 Subgroup of ruptured abdominal aortic aneurysm cases - median Interval of Referral per year, from 2012 to 2021
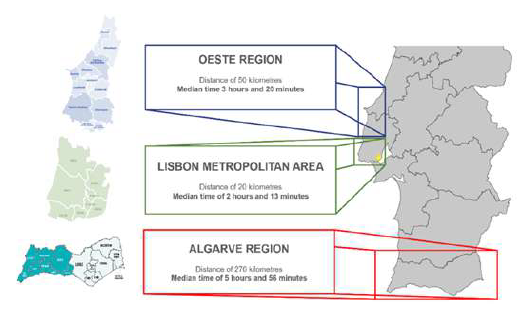
To analyse the Intervals of Referral relatively to the geographic region, the patients were divided according to the areas that refer to our hospital. We included four large groups: (1) Arriving directly through CHULN Emergency Department; (2) Metropolitan Area of Lisbon- mean distance of 20 kilometres; (3) Oeste Region- mean distance of 50 kilometres; (4) Algarve Region- mean distance of 280 kilometres.
Considering the ruptured aneurysm group (excluding the symptomatic group), the median Interval of Referral was 133 minutes (2 hours and 13 minutes), 200 minutes (3 hours and 20 minutes) and 356 minutes (5 hours and 56 minutes) respectively in the groups referred form the Metropolitan Area of Lisbon, the Oeste Region and the Algarve Region, Figure 5.
Door-OR Interval
In the whole group of patients referred from outside hospitals (Metropolitan Area of Lisbon, Oeste Region and Algarve Region), the median time between the admission at CHULN and the OR was 28 minutes. Interestingly, it was 37 minutes in patients with "in-house" diagnosis at the Emergency Department of our Institution (time between CT-angio and OR).
Influence of the median Interval of Referral on mortality rate
The overall post-surgery mortality rate in the whole population (ruptured and symptomatic) was 27% at 24 hours, 33% at 48 hours and 43% at 30 days. When analysing only those presenting with ruptured aneurysm, these rates rise to 30% at 24 hours, 37% at 48 hours and 47% at 30 days, Figure 6.
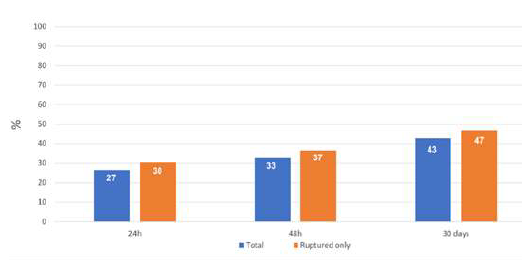
Figure 6 Overall mortality of patients treated with ruptured or symptomatic abdominal aortic aneurysms at Centro Hospitalar de Lisboa Norte, from 2012 to 2021. The blue bars represent include symptomatic patients, while the orange bars include only patients with confirmed rupture.
The median Interval of Referral was 182 (+/- 110) minutes (3 hours and 2 minutes) for survivors, it was 129 (+/-149) minutes (2 hours and 9 minutes) for patients dying within the first 24h and 129 (+/-114) minutes (2 hours and 9 minutes) in both the 48h and 30 days-deceased patients. No significant differences were observed between the Interval of Referral of the survivors and deceased patients at 24 hours (p = 0.907), nor at 48 hours (p = 0.743) nor at 30 days (p = 0.650).
The post-surgery mortality rate for those treated under 90 minutes was 29% at 24 hours, 42% at 48 hours and 55% at 30 days. Comparing them with those treated more than 90 minutes after the diagnosis, again no significant impact on the mortality was found, with mortality rate of 31% at 24 hours (p = 0.867), 35% at 48 hours (p = 0.465) and 43% at 30 days post-surgery (p = 0.286).
When analysing the data by geographic region of referral in ruptured aneurysms only, the mortality rate at 24 hours and at 30 days post-surgery was respectively 25% and 59% for those arriving directly at our Emergency Room, 35% and 48% for the Metropolitan Area of Lisbon, 30% and 38% for the Oeste Region and 19% and 29% for the Algarve Region, Figure 7.
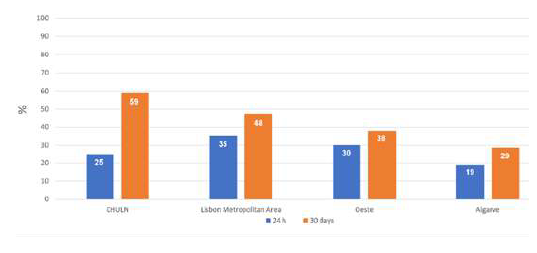
Figure 7 Mortality rate per different geographic regions, for the subgroup of patients with ruptured abdominal aortic aneurysm.
Comparing the mortality rates throughout the four areas of referral, no significant differences were observed between them, either by including only ruptured cases (p = 0.50 at 24h; p = 0.66 at 48h; p = 0.19 at 30 days) or for entire group of patients (p = 0.81 at 24h; p = 0.86 at 48h; p = 0.32 at 30 days).
When comparing the mortality rate between two clusters: (1) patients arriving at CHULN combined with those from Lisbon Metropolitan Area and (2) patients from Oeste and Algarve regions, there are also no significant difference in overall mortality at 24h (p = 0.52), 48h (p = 0.48) and 30 days (p = 0.06). These differences are not statistically significant although the net mortality is lower in patients coming from the Algarve.
DISCUSSIOn
The main results of our study are: (1) ruptured and symptomatic abdominal aortic aneurysms treated in our centre in a 10-year period exceeded largely the recommended time goals for this type of pathology and only 22% accomplished those targets; (2) this reality did not change over the study period; (3) nevertheless, there was no significant impact of these negative time goals on the mortality.
Regarding the first issue, a multifactorial explanation should be considered when analysing the Intervals of Referral. A low clinical awareness for the need of an urgent management in symptomatic and ruptured AAA may be the first problem raising possible training limitations in vascular pathology. Secondly, there is a clear and well-known dysfunction in the distribution of the 24/7 emergency departments with availability of Vascular Surgery in Portugal. In fact, and for example, our centre receives patients for the whole Algarve region located 280 kilometres away. This may be acceptable if a fast transport network is available what is not always the case.
We found no significant differences in the Intervals of Referral between the three regions connected to our centre. This may signify that even in geographically closer areas, like the Oeste and the Lisbon Metropolitan Areas, the referral times and transport system are still problematic leading to median times as high as nearly 4 times the recommended in the guidelines. For regions further away, like the Algarve, it reaches 6 hours. This problem was also recognized in other countries2 but the failure to accomplish the recommended time goals in 93% of patients is indeed an alarming sign.
After the referral notice of an incoming patient with AAA rupture, the time door-OR is relatively low but, interestingly, it is higher when the diagnosis is made in-house (in this case Interval CT-OR). This may be explained for the pre-preparation of the OR and teams after the notice of inbound patients during transport what is not the case in patients with an unexpected diagnosis in our hospital emergency department.
Our study confirms that the referral times are mainly a pre-tertiary centre issue, involving pathways that are not under the responsibility of the centres that will ultimately treat the patients. The recognition of all these referral and transport issues should be an opportunity for the Health System to improve fast track routine transport pathways for emergent pathology between different regions of the country and probably improve the disparity in the distribution of vascular surgery departments with an effective role in the treatment of urgent and emergent patients.
This is even more important as there were no signs of improvement in the last 10 years.
We found no relation with longer Intervals of Referral and mortality with patients from the Algarve, with median time between the CT and OR around 6 hours, showing the lower mortality. Of course, a "natural selection phenomenon" should explain this finding as patients with ruptured aneurysm with overt hemodynamic collapse will not make it while waiting several hours for treatment. The ones that can reach our centre alive are probably the ones with lesser hemodynamic and multiorgan compromise, thus more likely to survive. However, to prove this point, the information about the number of patients that died in peripheral centres, during transport or before reaching the OR in the four geographical areas of the study would be essential but, unfortunately, is not available.
Our study has some limitations. The main limitation is the lack of information about patients with ruptured aortic aneurysms that died before reaching our tertiary centre and the OR. The relatively small number of cases limits some comparative analysis. Finally, it is a retrospective study from a single centre.
conclusion
Only a small fraction of patients with ruptured abdominal aortic aneurysm in this cohort is treated within the recommend time frame, after the diagnosis is established. Even though this finding has no statistical impact on mortality, efforts should be made to improve the current timings of referral of acute abdominal aneurysm patients.