INTRODUCTION
Fibrosing alopecia in a pattern distribution (FAPD) was initially described by Zinkernagel and Trueb in 2000,1 as a distinct type of lymphocytic scarring alopecia. It is characterized by a combination of clinical, trichoscopic and histopathological features of both lichen planopilaris (LPP) and androgenetic alopecia (AGA).1,2-11FAPD may also coexist with frontal fibrosing alopecia (FFA).2
AGA is the most common form of non-scarring alopecia, caused by hair thinning on androgen dependent scalp.3 In women, most often, a diffuse hair loss occurs in all androgenetic area with maintenance of the frontal hairline (Ludwig pattern). Male pattern is characterized by bi-temporal recession of the frontal hairline, followed by diffuse thinning at the vertex (Hamilton-Norwood pattern).3
Classic LPP is an immune-mediated alopecia with chronic lymphocytic inflammation that leads to the selective destruction of hair follicles, resulting in scarring alopecia, with hair loss in patchy areas.4 FFA was once considered a subtype of LPP with selective involvement of the frontal-temporal hairline and eyebrows, but nowadays is considered a separate clinical entity.5
In FAPD, unlike LPP, we find vellus hair and hair loss in a pattern distribution involving the androgen-dependent scalp (similar to AGA). Unlike AGA, we find many focal areas of cicatricial alopecia, peripilar erythema and peripilar hyperkeratosis in trichoscopy and lichenoid inflammation in histopathology.1,2,6-9
It has been first described in Caucasians but may also affect Hispanics and African-descents.2,6,9 It is more common in women, most often in post-menopause or peri-menopause. It is rare in men and may develop at a younger age.2,6,9,11-15
This entity may easily be misdiagnosis as AGA with concurrent seborrheic dermatitis, with delay in the diagnosis and consequent fibrosis progression, leading to irreversible alopecia.
PATHOGENESIS
It has been suggested that FAPD is a variant of LPP10 or a lichenoid scarring variant of AGA.11 The last hypothesis is favored by the variable peri-follicular micro-inflammation observed in histopathology in many cases of AGA.
The cause for the location of a lichenoid infiltrate primarily around miniaturized hair follicles is unknown. Some authors propose that the damaged hair follicles may express different cytokines, initiating a repairing inflammatory process or an apoptosis-mediated organ deletion.2,6 Others suggest that the lichenoid reaction may be caused by unknown antigenic stimulus on altered AGA hair follicles in immunogenetically susceptible patients.2,8Androgens may play a role, considering that anti-androgen therapy decreasesscalp inflammation in some cases and stabilizes hair loss progression.2,9,10
There is one report of familial occurrence of FFA and FAPD in both mother and daughter, suggesting nosological relationship between the two conditions with respect to both the androgenetic background and the inflammatory reaction pattern.10,13Further studies are necessary to understand the pathophysiology of FAPD.
DIAGNOSIS
FAPD can be diagnosed by combination of physical exam, trichoscopy and histopathology. The main differential diagnoses are AGA, AGA plus seborrheic dermatitis and classic LPP.
Clinically, FAPD presents with patterned hair loss involving androgen dependent scalp - Ludwig pattern in women (Fig. 1) and Hamilton-Norwood pattern in men - with slowly progressive course. Some patients complain of scalp symptoms such as dysesthesia, pain, burning sensation and pruritus.2,16Physical exam reveals low hair density and sometimes peri-follicular erythema, follicular hyperkeratosis and absence of follicular openings may be detected by open eye.2,9Rare skin findings are frontal hairline recession similar to FFA, red dots in reticulated pattern on the chest and facial papules.2,17,18FAPD may affect the eyebrows, but unlike FFA, FAPD is not known to affect eyelashes or other body hair.17,18Patchy or asymmetric hair loss should be excluded for the diagnosis of FAPD.2
Regarding trichoscopy, the most important distinguishing findings between FAPD (Fig. 2) and AGA (Fig. 3) are loss of follicular openings, perifollicular erythema, and perifollicular hyperkeratosis. The last may have a tubular shape around the hair: peripilar casts. When surrounding the emergence of a tuft of 2-3 hairs, they are very typical and represents the optimal biopsy site for histologic diagnosis.2,6-9Other trichoscopic features are common to AGA, like hair diameter variability and predominance of single hair follicles. The presence of vellus hair in FAPD helps to distinguish it from classic LPP (Fig. 4). In patients with dark skin, a honeycomb pigmented network and scattered white small patches may also be seen, similar in presentation to what is seen in central centrifugal cicatricial alopecia (CCCA).2,9Dermoscopy alone may not be sufficient to distinguish between CCCA and FAPD in dark-skinned patients.

Figure 2 FAPD Trichoscopy: coexistence of vellus and terminal hair, mild peripilar scaling activity, with peripilar casts surrounding the emergence of tuft of 4 hairs (white arrow), mild interpilar erythema and micro-islands with no follicular orifices (scarring alopecia).

Figure 4 Trichoscopy: absence of follicular orifices in a large extension of the field (cicatricial alopecia), mild interpilar erythema and marked peripilar activity, consisting of circumferential desquamation(peripilar casts) and follicular plugs. Note the absence of vellus hair.
Skin biopsy is important to confirm diagnosis and may be performed with a 4-mm punch biopsy, guided by trichoscopy and processed with horizontal sections. The best locations are peripilar casts. In early lesions, we find a lymphohistiocytic infiltrate surrounding the hair follicle in the isthmus and infundibular regions and follicular interface dermatitis, with vacuolar degeneration of the follicular epitheliocytes.
Interface dermatitis in inter-follicular epidermis is rarely found and lower portions of the follicles, including the hair bulbs, are usually spared. Advanced lesions show concentric peri-follicular lamellar fibrosis (Fig. 5) and fibrosed follicular tracts.2,6-13,16,17There is hair follicle miniaturization, apoptosis of the basal keratinocytes and a decrease in sebaceous gland number.2,6 In FAPD, the follicular lichenoid reaction affects both miniaturized and non-miniaturized follicles in the affected scalp.2
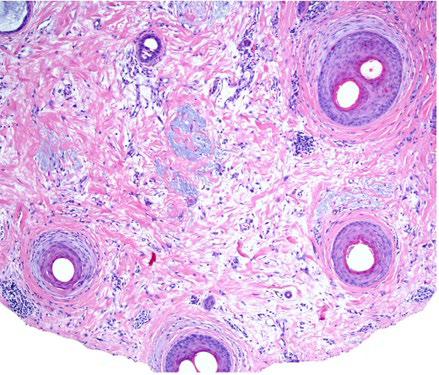
Figure 5 FAPD Histopahology: several follicles show perifollicular fibrosis and mild lichenoid infiltrate at the upper follicular level. Note the involvement of a vellus follicle. (horizontal sections, Hematoxylin and eosin, x10). Courtesy of Dr. Maryia Miteva (Miami University).
Combination of clinical pattern, trichoscopy and histopathology differentiates FAPD from AGA or classic LPP (Table 1).6,11,14The distinction between FAPD and AGA with seborrheic dermatitis is easy, because in the latter the scales are observed in the inter-pilar spaces and the follicular openings are present. The difference is important, especially in cases in which hair transplantation is being considered, because patients with FAPD, similarly to those with LPP, might not be good candidates for the procedure due to the potential risk of loss of the transplanted hair.2
Tabe 1 Differential diagnosis of FAPD. AGA, androgenetic alopecia; FAPD, fibrosing alopecia in a pattern distribution; LPP, lichen planopilaris.
| AGA | Classic LPP | FAPD | |
| Type | Non-scarring | Scarring | Scarring |
| Clinical Presentation | Alopecia in the androgen dependent scalp Men: Bitemporal and crown areas (Hamilton-Norwood pattern) Women: Crown and frontal areas (Ludwig pattern) No scalp symptoms | Patches of scarring alopecia occur anywhere on the scalp Scalp symptoms (pain, burning sensation) are frequent | Pattern distributed alopecia similar to as AGA Scalp symptoms (pain, burning sensation) can occur |
| Trichoscopy | - Hair diameter diversity - Perifollicular pigmentation / peripilar sign - Yellow dots | - Absence of vellus hair - Loss of follicular openings - Perifollicular erythema or/and perifollicular keratosis (peripilar casts) in multifocal scalp areas - White dots | - Hair diameter diversity - Loss of follicular openings - Perifollicular erythema and perifollicular keratosis (peripilar casts) limited to the area of androgenetic hair loss. - Hair tufting |
| Histopathology | - Miniaturized hair follicle - No interface dermatitis | - Lichenoid inflammation predominantly targeting isthmus and infundibular region of terminal hair follicle - Interface dermatitis in interfollicular Epidermis | - Miniaturized hair follicle - Lichenoid inflammation selectively targeting isthmus and infundibular region of miniaturized hair follicle - No interface dermatitis in interfollicular epidermis |
TREATMENT
There are few available data, limited to small retrospective studies and case reports.
The primary treatment goal is to stabilize the progression of hair loss and a secondary goal is to achieve hair regrowth. However, substantial improvement in advanced disease is impossible. Available agents aim to decrease inflammation and reverse miniaturization. Topical corticosteroids are the mostly used anti-inflammatory drugs, improving scalp symptoms alone and stabilizing hair loss in combination with other agents. Only in one case, stabilization in hair loss with topical clobetasol alone was reported.19,20Topical 0.05% clobetasol propionate (as foam, solution, and shampoo) has been successfully used combined with 5% minoxidil.16 Triamcinolone acetonide 0.2% solution used in combination with 5% topical minoxidil has also been a successful maintenance therapy.17
Oral hydroxychloroquine is commonly used in both FFA and LPP. A few data point its potential benefit in FADP in daily dose of 200-400 mg combined with topical therapy with clobetasol propionate and 5% minoxidil.2,16,17
Minoxidil is a hair growth promoter, thickening miniaturized hairs and is often used as complementary treatment in scarring alopecias. In FAPD, topical minoxidil is always used in combination with other agents to stabilize hair loss.1,16,17There are no data about using oral minoxidil in FAPD.
Antiandrogens drugs, even in monotherapy, may stabilize the disease. One man treated with 1 mg daily finasteride presented both decreased inflammation and hair loss.1
Finasteride seems to be beneficial in women with FAPD refractory to topical therapy with minoxidil and clobetasol.2,16There are two successful cases of women treated with oral cyproterone acetate combined with topical 5% minoxidil and clobetasol propionate,1 but recently there is concern about the association between oral cyproterone acetate and the occurrence of meningioma.19-21
Although topical retinoids may contribute to hair regrowth in patients with AGA, in FAPD no benefit was observed.2
CONCLUSION
FAPD is an entity to consider in the differential diagnoses of scarring alopecias. The scalp shows features of both LPP and AGA. Clinical findings, trichoscopic features and histopathology allows us to distinguish between them. Early recognition and proper treatment allow disease stabilization the and avoid permanent follicular hair damage.
KEY-POINTS
- Fibrosing alopecia in a pattern distribution is a scarring alopecia with lichenoid Inflammation involving miniaturized hair, in androgen-dependent scalp.
- Clues for diagnosis are hair loss resembling androgenetic alopecia and trichoscopic findings of peripilar casts and loss of follicular openings.
- Anti-inflammatory agents in combination with hair growth promoters and/or anti-androgen drugs can stabilize the disease decreasing hair loss.

















