Introduction
We report the case of a 71-year-old woman diagnosed in the past with a left infiltrating ductal breast carcinoma for which she underwent breast-conserving surgery, axillary lymph node dissection and adjuvant chemotherapy. Thirteen years after surgery, she noticed a pigmented papule which rapidly grew into a hyperkeratotic black plaque surrounding her left nipple. Multiple adjacent black macules were also noticed.
Histopathological analysis revealed intraepidermal and dermal infiltration by atypical epithelioid cells, displaying pagetoid intraepidermal spread. Immunostaining showed positivity for estrogen, progesterone receptors and human epidermal growth factor receptor-type 2 (HER-2). It was also pan-cytokeratin (pan-CK) positive and cytokeratin-7 (CK7) negative.
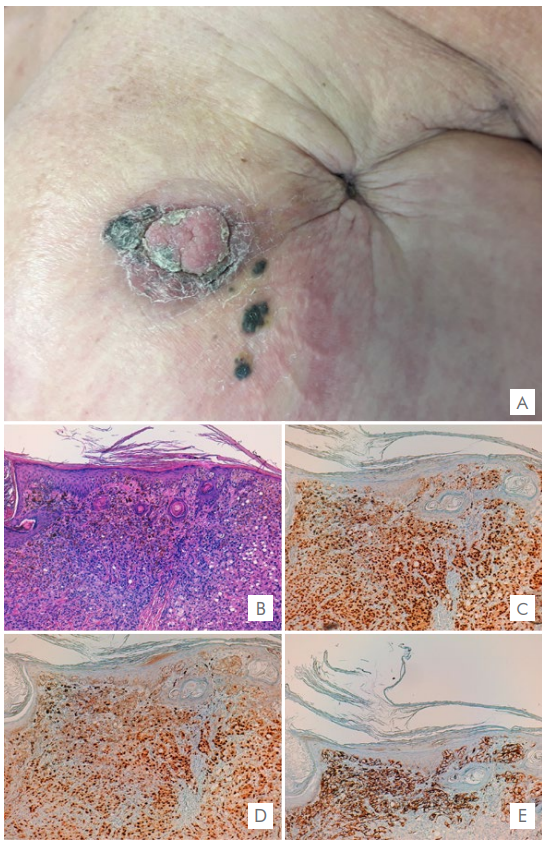
Figure 1 (A) Hyperkeratotic pigmented plaque surrounding the nipple and multiple black macules in the adjacent area; sequel retraction from previous breast-conserving surgery. Skin biopsy (hematoxylin-eosin stain and immunohistochemistry x100) shows: (B) Intraepidermal and dermal infiltration by atypical epithelioid cells, displaying pagetoid intraepidermal spread. Dense pigmentation of the superficial dermis and epidermis. (C) Estrogen receptors; (D) Progesterone receptors; (E) Melan-A showing positivity of dendritic melanocytes surrounding tumor cells.
Pigmented epidermotropic metastases from breast carcinoma
Cutaneous metastases of a primary internal malignancy are relatively uncommon, accounting for 0.7%‐9% of all metastases. 1 They often occur later in the course of the disease and may manifest years after treatment of the primary tumor. They usually represent a sign of poor prognosis. 2
Breast carcinoma is the most frequent malignancy causing cutaneous metastases3 with a wide range of clinical manifestations and histological appearances. 2 Nodules are the most common clinical presentation but numerous other patterns are described.
Pigmented epidermotropic metastases from breast carcinoma are rare and have not often been described on the literature. 4 They are generally found on the chest and abdominal wall, near the mastectomy scar. 2,5The presence of pigment can be explained by the melanin release from damaged epidermis due to invasion and destruction by tumor cells and consequent phagocytosis by melanophages. 5 Other theories suggest that there is a transfer of melanin from the melanocytes into the carcinoma cells or even that the tumor cells themselves can produce melanin. 2,6,7
On histology, cords, nests and large aggregations of neoplastic cells are present in the dermis and often communicate with the epidermis in a pagetoid spread. 5 The intraepidermal and dermal tumor cells contain melanin in their cytoplasm, and numerous dermal melanophages can be also seen. 4,8
Immunohistochemistry is another helpful tool used to differentiate these findings from clinically indistinguishable entities such as malignant melanoma.8Breast carcinomas are typically cytokeratin 7 positive and cytokeratin 20 negative. 9 S100, HMB45, and Melan-A staining are negative in the majority of cases, in contrast to malignant melanoma. In this case, Melan-A expression was limited to dendritic melanocytes surrounding tumor cells, which did not show cytological atypia or mitotic activity. The presence of estrogen and progesterone hormone receptors and HER2 expression can be evaluated and, as in our case, are frequently positive. 8
In conclusion, this case describes the occurrence of epidermotropic pigmented metastasis manifesting 13 years after the diagnosis of a ductal breast carcinoma. Due to their clinical and histological similarity, pigmented epidermotropic metastases can mimic malignant melanoma which can ultimately lead to a delay in diagnosis of anactive or recurrent internal malignancy. 2 Therefore, the onset of a new pigmented lesion especially close to the surgical scar in patients with an history of internal malignancy should raise suspicion for cutaneous metastasis. Prompt and adequate diagnosis of this condition can significantly impact the patient’s overall prognosis.















