INTRODUCTION
Vitiligo is an acquired disorder characterized by loss of pigmentation due to autoimmune destruction of melanocytes. It has a varied morphology manifesting as depigmented patches involving skin, hair and mucous membranes.1 Although it is an ancient disease, the pathogenesis still remains an enigma. Multiple hypothesis have been suggested to explain the etiopathogenesis including autoimmune theory, self-destructive theory, neural theory, biochemical theory, growth factor reduction hypothesis, melanocytorrhagy and stress.2 It has been accepted that all these factors synergistically play a role in melanocyte loss. Vitiligo is classified as segmental and nonsegmental. Other phenotypes include trichrome, pentachrome, red vitiligo, blue vitiligo or follicular vitiligo.3 Despite the fact that it is a benign disease, it carries the burden of social stigmatization leading to negative impact on quality of life of the patient. Several pseudo beliefs prevail in the society causing depression, low self-esteem and isolation amongst sufferers.4 With a plethora of therapeutic modalities available, none seems to give the ideal response. Management includes both non-surgical and surgical options. Medical treatment includes oral and topical corticosteroids, topical calcineurin inhibitors, phototherapy, topical vitamin D analogues, antioxidants and immunosuppressants.5 Tacrolimus is a frequently used immunosuppressive agent. It is a calcineurin inhibitor that has a direct effect on melanocyte growth and migration. It inhibits T cell activation and restores the altered cytokine network. It is commonly used in children and in sun exposed areas. Better outcomes have been observed with combination treatments.6 Microneedling is a method of transdermal drug delivery by creating micropores through the stratum corneum. It aug-ments drug absorption as well as causes mechanical migration of melanocytes from margins to amelanotic areas. It leads to therapeutic wounding and stimulates the release of multiple growth factors.7 Dermapen is a fractional microneedling device. Its automated needling motion increases effectiveness, minimizes pain and discomfort and promotes an even absorption of topicals.8Microneedling has been tried with several drugs and reported to be more beneficial than monotherapy.7
MATERIAL AND METHODS
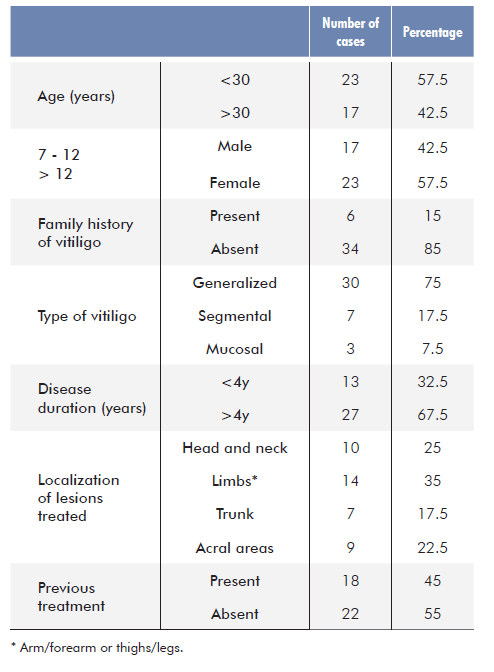
Forty patients with localized and stable vitiligo for more than one year were enrolled in this study. A written informed consent was obtained from each patient. This was a hospital based interventional study conducted in the outpatient Department of Dermatology, Venereology & Leprosy during the period from March 2019 to July 2020.
Exclusion criteria were as follows: pregnancy or lactation, history of keloid / hypertrophic scarring, active infection, bleeding or coagulation disorders, disease duration less than 1 year and patients receiving any treatment for vitiligo within the last 6 months. This study included patients aged 12-60 years with vitiligo diagnosed clinically for >1 year who were willing to come for regular follow-up. Single vitiligo patch measuring less than 10 cm2 was selected in each patient. Skin biopsy was performed in difficult to diagnose cases.
Under aseptic precautions local anaesthesia was infiltrated in the selected vitiligo lesion following which, a layer of tacrolimus oint-ment 0.1% was applied and microneedling was done with dermapen using the lowest speed with needle penetration depth ranging from 0.25 to 0.5 mm over face and 1 to 2 mm over body in horizontal and vertical directions until pin point bleeding was observed. After cleaning with a povidone iodine solution, tacrolimus ointment 0.1% was applied under occlusive dressing for the remaining of the day. This procedure was repeated every 2 weeks for a maximum of 10 sessions. Patients were advised to apply tacrolimus ointment twice daily in between the sessions and were followed up for 6 months after the last session. Any adverse effects or complications were recorded.
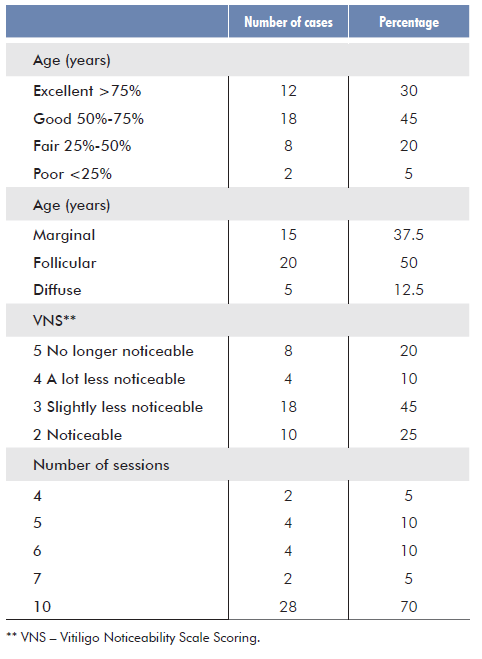
Repigmentation was assessed by two dermatologists (other than those involved in this study) with the help of photographs which were taken at baseline, before each session and at follow-ups. Repigmentation response was graded as: G0 <25% - poor; G1 25%-50% - fair; G2 50%-75% - good; G3 >75% - excellent.
Vitiligo noticeability scale (VNS) was also used to measure the outcome from the patient’s perspective. Scoring was done as followed: 1 more noticeable; 2 as noticeable; 3 slightly less noticea-ble; 4 a lot less noticeable; 5 no longer noticeable.
Statistical methods: Collected data was organized and statistically analyzed using SPSS software version 19. Frequency, mean and standard deviation were calculated. Pearson Chi Square test was used in this study. P value <0.05 was considered statistically significant.
Ethical considerations: Informed written consent was taken on a prestructured proforma from every adult patient and from guardians in case of minors. The study conducted was in accordance with the amended Declaration of Helsinki and approval for the study was obtained from the institutional ethics committee in February 2019. (Reference no. Patho 182/19)
RESULTS
This study comprised 40 patients with clinically diagnosed stable vitiligo. There were 23 females and 17 males with ages ranging from 12 to 60 years. Demographic and clinical data are presented in table 1. All patients completed the required treatment and follow-up period.
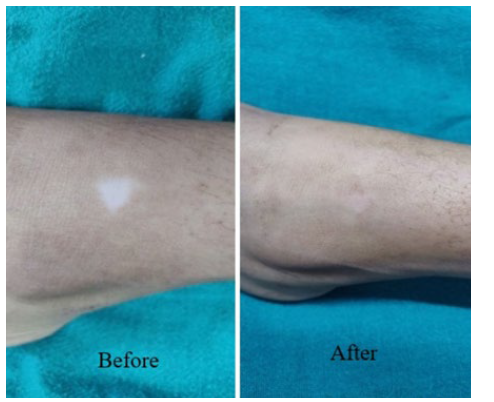
With regard to repigmentation evaluation, excellent response (>75%) was observed in 30% of the cases and good response (50%-75%) in 45% (Fig. 1-3). In terms of patient’s vitiligo noticeability scale scoring (VNS), 20% cases had a score of 5 (no longer noticeable) and 10% had a score of 4 (a lot less noticeable). The start of repigmentation was seen after a single session and excellent response was achieved within 2 months in 2 cases. Minimum number of sessions required to achieve excellent response was 4. Predominant pattern of repigmentation was perifollicular in 50% cases, followed by marginal in 37.5% cases and diffuse in 12.5% cases.
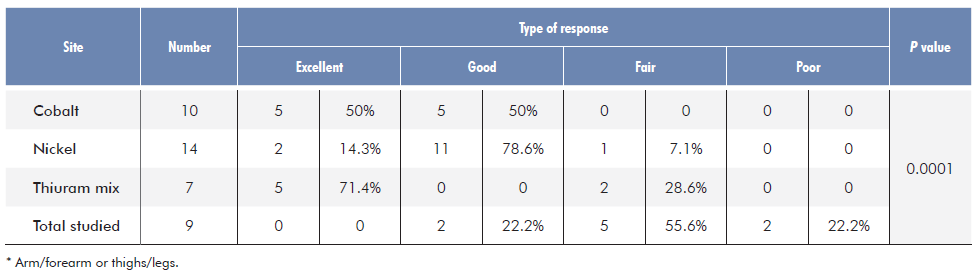
Comparison between the type of response and site is shown in Table 3. Maximum number of lesions were present over limbs (arms/forearms or thighs/legs) followed by head and neck, acral areas and trunk. Good to excellent (>50%) response was achieved in all head and neck cases and in 92.8% of limbs. Of the head and neck cases, 3 (7.5%) had mucosal vitiligo involving the lips, out of which 2 had excellent response and 1 had good response. Trunk showed excellent response in 71.4% cases and fair response in 28.6% cases. None of the cases showed excellent response over acral areas. The statistical comparison was highly significant (p= 0.0001).
Pain, reported in 1 case, was present for a few hours after the procedure and gradually subsided. No side effects were observed in the remaining 39 cases. Repigmentation was stable and neither recurrences nor long-term complications were reported during the follow-up period of 6 months.
DISCUSSION
Vitiligo is a depigmenting disorder due to autoimmune destruction of melanocytes. It affects 1%-2% of the world’s population.1
In a country of darker skin type, overwhelming psychological burden is seen due to the social outcast and stigma faced by affected patients. It has been observed that repigmentation decreases the suffering and improves quality of life. The natural course of the disease is unpredictable and difficult to control. Many treatment options have been tried in the past but none has produced satisfactory results. Medical treatment remains the mainstay in most of the cases, namely-tacrolimus. Recently described methods of therapeutic wounding have gained attention and microneedling is one such modality.9 It is an effective and simple technique that aims at stimulating and repopulating the melanocytes into depigmented lesion. It is a safe, simple to learn and easily accessible procedure. Great potential has been shown by this technique in recalcitrant lesions especially when used in combination with other drugs.7 Our aim was to use microneedling as a complementary approach to the traditional therapy in vitiligo.
The beginning of repigmentation was seen after the first session in the form of erythema or mild pigmentation, and excellent repigmentation was attained in 5% of cases within 2 months (4 sessions). This was faster than the results observed by Ebrahim HM et al who compared tacrolimus and microneedling with tacrolimus monotherapy and observed initiation of repigmentation after 3 to 4 sessions.10 This can be attributed to the difference in procedure as, with our technique, tacrolimus was applied prior to microneedling. This ensures uniform and deeper penetration of the drug. Mina M et al. studied the use of tacrolimus 0.03% with microneedling and observed initiation of repigmentation within 6 weeks.11 Good to excellent response was seen in 75% cases. In terms of patient’s vitiligo noticeability scale scoring (VNS), 20% cases had a score of 5 (no longer noticeable) and 10% cases had a score of 4 (a lot less noticeable). This was comparable to the grading of repigmentation of excellent response (>75%), which was seen in 30% of cases. A total of 45% cases had VNS score of 3 (slightly less noticeable) which was comparable to good response (50%-75%) seen in 45% of cases. Our study showed better response than Ebrahim HM et al where good to excellent response was seen in 70.8% cases.10 In a different study by Ebrahim HM et al, microneedling combined with tacrolimus showed a better outcome (excellent response in 66.6%) than isolated microneedling or tacrolimus.12 Good to excellent res-ponse (>50%) in 10 (40%) lesions with tacrolimus was reported by Mina M et al.11 Passerson T et al combined tacrolimus and 308 nm excimer laser and observed excellent repigmentation in 70% lesions.13 Nistico S et al combined tacrolimus with excimer laser and showed excellent response in 50% patients.14 Fai D et al concluded that combination of tacrolimus and NB UVB had better outcome than NB UVB alone. Their study showed excellent repigmentation in 53.3% cases.15
In our study, a better response was observed on the head, neck and limbs and a poorer response on the trunk and acral areas. We also evaluated the response of this combination in mucosal (lip) vitiligo: Out of 3 cases, 2 had excellent response and 1 showed good response. It was very well tolerated overall, with only one reported case of pain. As tacrolimus is a safe drug to treat mucosa, this combination may provide a scope of investigation for treatment of mucosal vitiligo, considered a hard to treat area and a possible in-dication for surgical management. In comparison to various surgical options, microneedling seems to be the safer, easier to perform and less time consuming with minimum complications.
Previous studies have shown that tacrolimus is an effective therapy for head and neck areas due to the greater density of hair follicles.16 Our findings were almost similar to Ebrahim HM et al, who reported that tacrolimus and microneedling showed maxi-mum repigmentation on the face, followed by limbs, trunk and acral areas.12 In a different study by the same authors, best results were seen on face followed by legs, trunk, elbows and knees. Acral areas also showed satisfactory improvement.10 In our study, none of the lesions present over acral areas showed excellent response and good response was only observed in 22.2% cases. The pattern of repigmentation was perifollicular in 50% of the cases followed by marginal in 37.5% and diffuse in 12.5%, which was consistent with previous studies.11,12
No major adverse effects were observed in our study. Pain was reported by one patient but it gradually decreased within a few hours. Some authors reported mild pain, itching and erythema in few patients but the procedure was also generally considered as well tolerated.11
Multiple options have been suggested for therapeutic wounding like TCA, phenol, needling, excimer laser, cryotherapy or dermabrasion. From these, microneedling stands out as a simple, quick and cost-effective method that can be used as a surgical intervention in stable vitiligo.9 It is a minimally invasive procedure that does not require hospital stay. There is no major blood loss and the patient is comfortable during the entire procedure. Microneedling is usually free of complications like cobblestoning, pseudomembrane formation, atrophy, scar formation or variegated appearance which are regularly observed with other surgical modalities. Response in mucosal vitiligo was positive in our study but these findings warrant further studies with larger samples. This technique should be considered as a viable option for dermatologists to treat resistant vitiligo lesions.
CONCLUSION
Microneedling with tacrolimus is an efficacious option for the treat-ment of stable vitiligo. The simplicity of the procedure and the results obtained can help patients and reduce the psychological burden due to the stigmatization associated with the disorder. Further research - should be undertaken to evaluate the response in mucosal vitiligo, the long-term stability of repigmentation and complications.