INTRODUCTION
Carcinoma cuniculatum is a rare variant of verrucous carcinoma, described by Aird et al, in 1954. It is an indolent form of well-differentiated squamous cell carcinoma with a low grade malignancy. The tumor rarely metastasizes but it can slowly and progressively invade deeper tissues.1 It was originally described as a verrucous carcinoma of the soles, but, exceptionally, it can arise in other parts of the skin.2 Clinically, it presents as an exophytic lesion that can mimic several benign dermatoses, therefore with a frequent delay of months to years before the correct diagnosis.3 We report a case of carcinoma cuniculatum with atypical location and bone involvement, whose initial clinical and histopathological diagnosis was of common wart.
CASE REPORT
A 71-year-old male, Fitzpatrick skin type III, agricultural worker, hypertensive and with a previous history of basal cell carcinoma, presented with a painful warty lesion in the fourth left finger that was progressively growing for 1 year. Dermatological examination revealed a crateriform nodule with erythematous and infiltrated edges affecting the dorsal surface of the medial phalanx, with exudate drainage (Fig. 1A). No axillary lymph nodes were found on palpation. Cutaneous biopsy, performed in another hospital, was consistent with viral wart. Imiquimod applied 3 times a week, for 12 weeks, induced partial lesion regression (Fig. 1B). Radiography of the affected finger did not show particularities. Raising the hypothesis of squamous cell carcinoma, a new biopsy was compatible with keratoacanthoma in a regressive stage. Human papillomavirus typing was not performed due to unavailability in our hospital. Fungal culture was negative. Because of le-sion extension and histopathological reports compatible with benignity, it was decided to try chemical destruction before a surgical approach. So, 3 applications of trichloroacetic acid 90% were accomplished, with lesional reduction (Fig. 1C). However, he maintained intense local pain. After this treatment, a third biopsy was performed to check for lesion persistence, showing hyper- and parakeratosis, keratinocytes with karyomegaly, hyperchromasia and perinuclear halo, coarse keratohyaline granules in the upper layers, dermal papillomatosis, capillary ectasia in the papillary dermis, suggesting the diagnosis of wart viral again, without morphological evidence of malignancy. A new radiography showed erosion in the medial and distal phalanges (Fig. 1D). Patient sought assistance from an orthopedist, who amputated the affected finger based on radiographic findings. Anatomopathological examination of the surgical specimen showed a well-differentiated squamous cell carcinoma, infiltrating deep planes, with bone destruction, with 2.8 x 2.1 cm and free surgical margins (Fig. 3-5). Staging was performed with chest radiography and abdominal ultrasound which were normal. As lymph node chains are clinically free and no evidence for metasta-ses, the tumor was staged pT4, cN0, cM0. No signs of tumor recurrence have been noted after 12 months of follow-up.
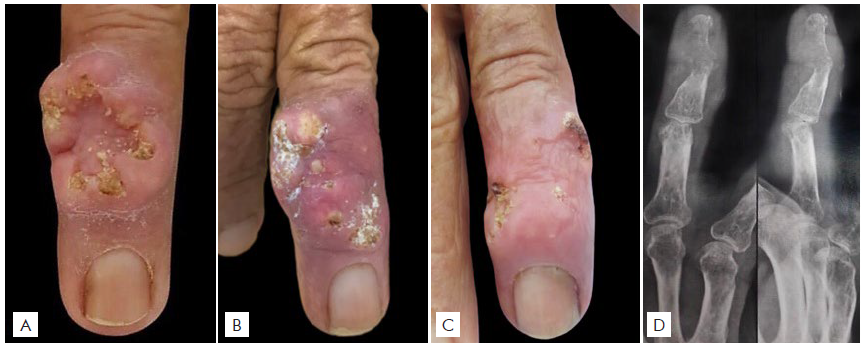
Figura 1 (A) Crateriform vegetating lesion in the medial phalanx of the 4th left finger; (B) After 12 weeks of using Imiquimod; (C) After 3 applications of trichloroacetic acid 90%; (D) Radiograph of the affected finger showing erosion in medial and distal phalanges.
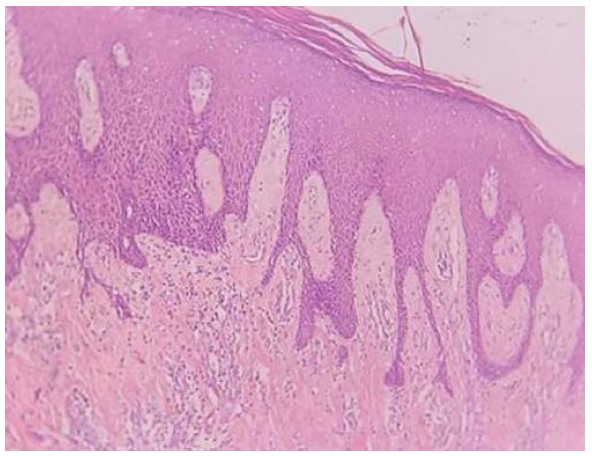
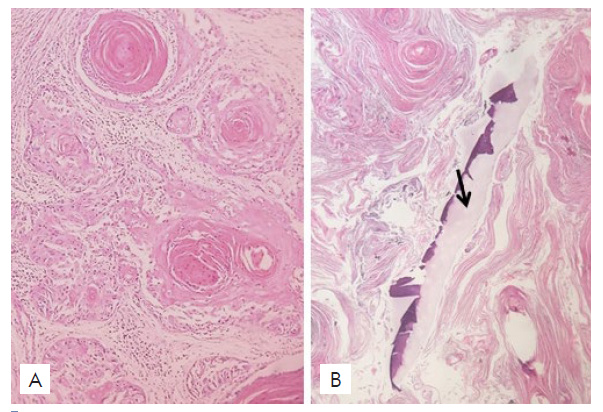
Figure 2 Superficial biopsy showing epidermal hyperplasia simula-ting pseudoepitheliomatous hyperplasia (HE 100x).

Figure 3 Neoplastic proliferation of well-differentiated epithelial cells invading the reticular dermis (HE 100x).
DISCUSSION
Verrucous carcinoma, first described by Ackerman in 1948, is distinguished into three different subtypes according to its location: the oral form, called oral florid papillomatosis or Ackerman tumour; the giant condyloma of Buschke and Löwenstein, that affects the anogenital region; and lastly, ephitelioma cunniculatum, described by Aird et al in 1954, in the plantar region.2,4Cuniculatum is Latin for “rabbit warren”, referring to this tumor’s many sinuses and keratin-filled crypts.5Carcinoma cuniculatum was originally named epithelioma cuniculatum, which was believed to be restricted to the plantar surface of the foot. However, since its first description, it has been reported to affect other anatomic sites, such hands and mucous membranes.6,7
The pathogenesis remains unknown, with theories proposing an association with human papillomavirus (HPV) infection, chronic inflammation and trauma. In the case of plantar injuries, the both oncogenic low and high-risk types of HPV have been reported, respectively HPV 6,11 and HPV 16,18.5 The relationship between oncogenesis of non-melanoma skin cancer and HPV viral warts is still controversial. An argument in favor of this pathogenesis is the increased prevalence of viral warts and squamous carcinoma in some conditions such as solid organ transplantation and epidermodysplasia verruciform.8 In both conditions, viral warts precede the onset of carcinoma.9 Another relevant factor is the higher prevalence of HPV in samples of squamous cell carcinomas (78%) when compared to basal cell carcinomas (36%) and even normal skin (32%).8 Nevertheless, the mere evidence of a viral infection is not enough to incur a malignant transformation, because most patients infected with HPV do not develop cancer. Co-factors are necessary.10
Carcinoma cuniculatum is more frequent in men, between the fifth and sixth decades of life. Clinically, it presents as a solitary exophytic, verrucous and painful tumor, that can ulcerate and drain a malodorous exudate. It has slow and progressive growth, with a tendency to local recurrence. In 90% of cases, the tumor is found on the feet, usually in the plantar region, mostly in the ball of the foot.11,12Exceptionally, other locations have been described: hands, fingers, buttock, penis, knees, abdominal wall, intertriginous areas and mucous membranes (oral and nasal cavity, larynx, pharynx, esophagus).2,7
Clinically and histologically, this tumor simulates a variety of benign skin lesions due to its indolent course and the presence of well-differentiated tumor cells. Therefore, early diagnosis is unusual.1,3The differential diagnosis includes verruca vulgaris, reactive epidermal hyperplasia, eccrine poroma, actinomycosis, adnexal tumours, giant seborrhoeic keratosis, giant keratocanthoma, hyperkeratotic basal cell carcinoma and squamous cell carcinoma.3,5,13Reports of injuries initially diagnosed as warts, with progressive growth despite topical treatment, are frequent in the literature, as in our patient.5 The delay in diagnosis allows the invasion to the underlying bones.1 The median time to diagnosis was 13 years in one study and 16 years in another case series. So, lesions that do not respond to appropriate therapy should be biopsied.14
On pathological examination, carcinoma cuniculatum looks as a well-differentiated squamous cell carcinoma with low-grade cytological atypia and burrowing sinus tracts, often filled with keratinous debris, descending to the subcutaneous fat and sometimes infiltrating the bone.1 The difficulty in histological diagnosis is because of the relatively benign-appearing columns of well-differentiated squamous epithelium with low mitotic activity and only slight cellular or nuclear atypia.11The superficial portions generally resemble a wart, as they present hyperkeratosis, parakeratosis and acanthosis.3 The invasion of deep tissues, sometimes confined to only a few foci in large samples, makes the diagnosis certain. Superficial biopsies may therefore result in misdiagnosis, being indispensable to obtain a large biopsy, including deep dermis and subcutaneous tissue.11In many reported cases, multiple biopsies were required. However, the correct diagnosis is often performed only by histological examination of the entire lesion after surgical excision, as in our case.3
The tumor rarely metastasizes, but is capable of a slow and progressive invasion of the deeper tissues, such as tendons and muscles, and may eventually reach the bone.1 The incidence of infiltrating adjacent bone is documented at 5%-10%, while regional lymphatic ganglia metastasis may be found in 5% of cases.10,11There is only one report of metastasis to lung.14 Patients with verrucous carcinoma generally have a favorable prognosis, with a 5-year survival rate of 75%.5
The current mainstay of treatment is surgical excision, with tumor-free margins of at least 5 mm.1 Amputations are necessary when the tumor is too extensive or recur after multiple attempts of local excision.14 Radiological assessment with computed tomography is useful to evaluate the evidence of possible bone involvement, which can show early typical signs of an aggressive tumor, as radiolucent lesions with illdefined margins and resorption of the adjacent cortical bone.15 Moh’s technique, which allows total tumor removal with maximum preservation of normal tissue structure, has been successfully implemented in patients with carcinoma cuniculatum.14 Other conservative therapeutic approaches, as electrodesiccation, cryotherapy and laser ablation, are not always effective and often result in tumor recurrence.1 Oral retinoid is an effective alternative therapy for the treatment of multiple cutaneous verrucous carcinomas or inoperative lesions.16 Some authors recommend radiotherapy in inoperable or metastatic cases, whereas others affirm that it can lead to the anaplastic transformation of the carcinoma.2,10Immunotherapy with ipilimumab or anti-PD-1 antibodies, such as nivolumab and pembrolizumab, may be a therapeutic alternative in the future.10 After treatment, patient follow-up is required, as recurrence has been reported despite clear histological resection margins.15
In conclusion, carcinoma cuniculatum is a well-differentiated squamous cell carcinoma with low intrinsic aggressive potential. However, it is often misdiagnosed and, like in the present patient, late diagnosis and inappropriate therapeutic approaches favor the invasion of the underlying bone, leading to a substantial morbidity. Early diagnosis depends on high clinical suspicion and adequate biopsy. Therefore, it is important to alert dermatologists to recognize and suspect this uncommon variant of squamous cell carcinoma.